Journal Information
Vol. 60. Issue 12.
Pages 784-785 (December 2024)
Vol. 60. Issue 12.
Pages 784-785 (December 2024)
Clinical Letter
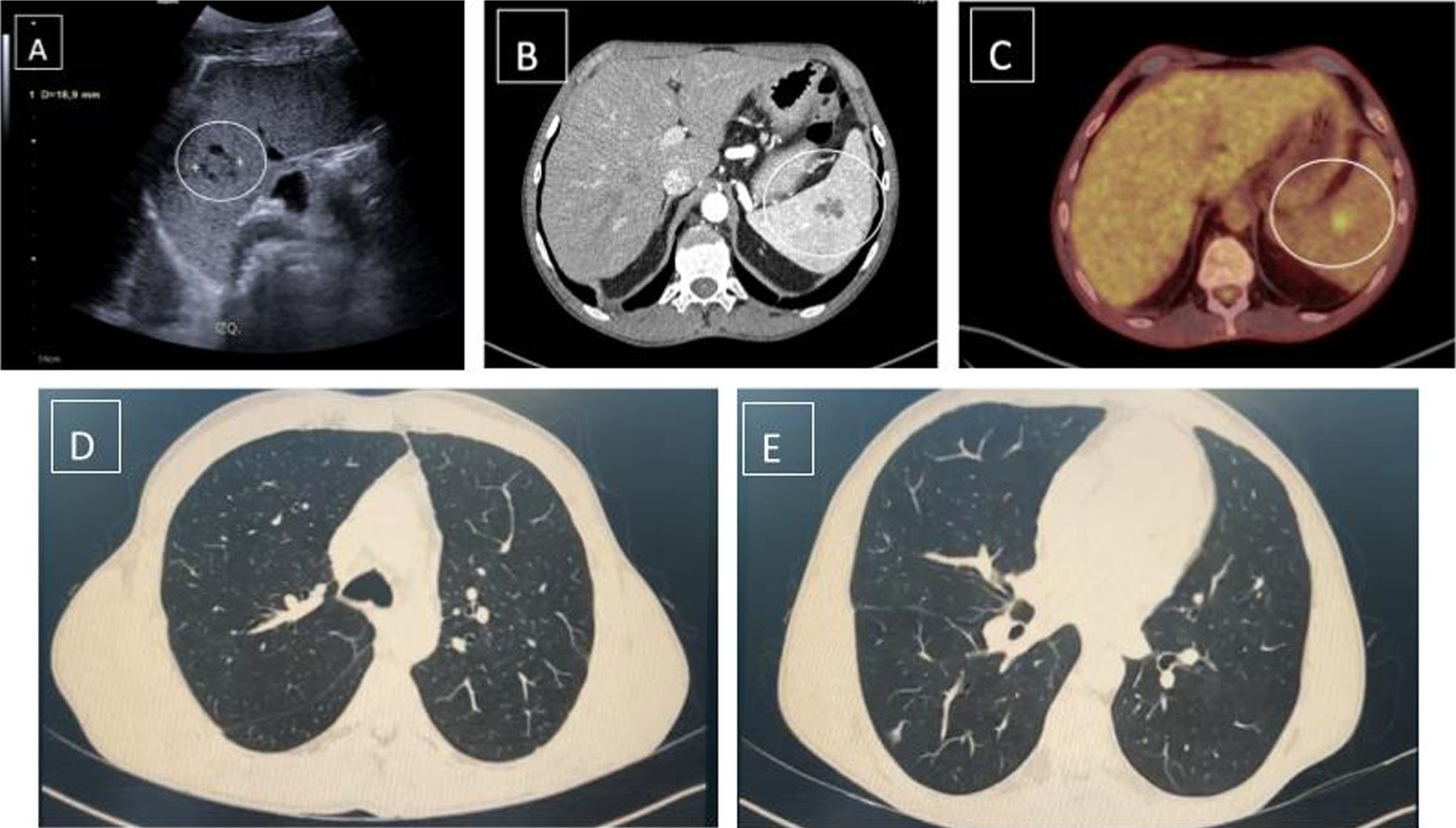
Intermittent Fever of Unknown Origin in a Lung Transplant Recipient
Visits
739
Andrea Expósito Marrero
, Myriam Aguilar Pérez
Corresponding author
Hospital Universitario Puerta de Hierro, Madrid, Spain
This item has received
Article information
These are the options to access the full texts of the publication Archivos de Bronconeumología