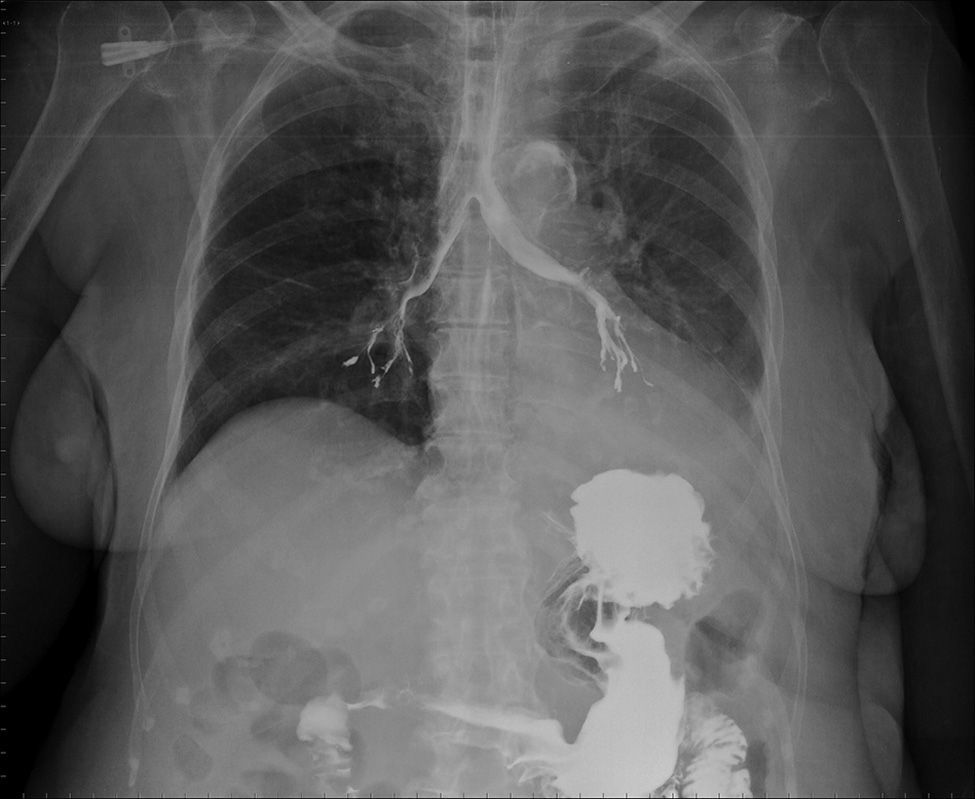
An 81-year-old woman with a history of cognitive impairment, diabetes mellitus type 2, hypertension, and cerebrovascular disease with a previous atherothrombotic ischemic stroke in the territory of the right middle cerebral artery, causing residual hemiparesis, was admitted for the study of chronic diarrhea, intestinal malabsorption, and protein-losing enteropathy. A small bowel follow-through was performed with no findings of interest, with the exception of the incidental radiological observation of contrast medium passing into the bronchial tree (Fig. 1).
Functional oropharyngeal dysphagia is a specific geriatric syndrome, common in fragile patients, that affects from 38% to 51% of institutionalized elderly individuals, depending on the series. Prevalence in senile patients with a history of stroke can be as high as 81%.1 The impact on functional performance and quality of life is considerable, as it can cause malnutrition, dehydration, and tracheobronchial aspiration, that are frequently silent and undetected, but which can cause pneumonia in up to 50% of cases.1,2
Please cite this article as: Guirao-Arrabal E, García-Castro JM, Parra-García GD. Broncografía incidental. Arch Bronconeumol. 2016;52:613.