Lipoid pneumonia (LP) is an uncommon condition that occurs as a result of the deposit of exogenous or endogenous fatty materials in the lung tissue. The incidence of LP is between 1% and 2.5% according to some series of autopsies.1
We report the case of a 15-year-old male patient with a history of jaundice at the age of 4 days, febrile seizure at one year and 4 months, scarlatiniform syndrome at 5 years, erysipeloid rash at 7 years of age, and hip synovitis. He has been monitored by the pediatric department since he was 8 years old due to delayed growth and development, with episodes of coughing and exertional dyspnea. He was diagnosed with mild episodic asthma, and was treated with montelukast and albuterol as rescue medication, without improvement. The following analyses were performed: ANA, C3, C4, CD3, Nk, IgE, eosinophils, granulocyte function, immunoglobulins, TSH, test for celiac disease, sweat test, skin prick and radioallergosorbent test for food allergies; all results were normal. He has had contact with 2 canary birds from an early age, and with spray paints at 11–12 years of age (graffiti).
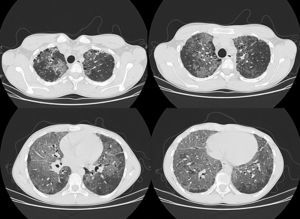
Upon admission to the pulmonology unit, the patient had dyspnea grade I–II. Physical examination revealed good coloration of the skin and mucous membranes, and finger clubbing. Baseline O2 saturation was 93% and good vesicular breath sounds were perceived upon auscultation, with no added noises. Spirometry indicated FEV1: 44%, FVC: 47%, FEV1/FVC: 79, MMEF: 29%, although patient cooperation was incomplete. The chest X-ray showed an extensive bilateral alveolointerstitial pattern with multilobar involvement. The examination was completed during hospitalization with high-resolution computed tomography (HRCT), in which marked alteration of the lung parenchyma was observed, with large ground-glass fields in all lobes, but predominantly basal. There was overlapping septal thickening, forming a crazy-paving pattern (Fig. 1). Furthermore, honeycombing areas were visible in the subpleural lung parenchyma at the level of both upper lobes, although predominantly in the right side.
In view of these findings, a transbronchial biopsy was performed. The histological study showed giant cells phagocytosing foreign body cholesterol crystals in the alveolar interstitium and alveolar spaces, along with both isolated and accumulated macrophages with microvacuolated cytoplasm. There was occasional eosinophilic pseudo-proteinaceous material in the alveolar spaces that was negative on PAS and Congo red staining. No micro-organisms were observed. Histological findings were compatible with LP.
Currently the patient is receiving oral and inhaled corticosteroids, which have resulted in a clinical improvement, although the radiographic findings have shown no change.
In the absence of frequent use of laxatives, balms, oils or other lubricants, other causes of endogenous pneumonia should be assessed,1 such as bronchial obstruction produced by a pulmonary tumor (clearly ruled out in our case), repeated episodes of respiratory fungal infection (not recorded in the patient's medical history nor suggested by histological or laboratory data), alveolar proteinosis (ruled out by pathology) and Niemann-Pick disease (mainly type B), in which crazy-paving pattern has also been described.2 However, the patient did not present hepatosplenomegaly or any laboratory abnormality suggesting this possibility. Thus, in the absence of any other identifiable cause, this case was classified as idiopathic LP.3
The most common HRCT radiological findings in LP4,5 are the presence of condensation with low attenuation coefficient (between −75 and −35 UH) that is very specific and prevalent in endogenous LP,1 ground-glass opacities, crazy-paving pattern, and presence of centrilobular opacities. In addition, lung involvement is mainly basal.4
The crazy-paving pattern was initially described in alveolar proteinosis, although it was later shown to appear in several processes,4 including sarcoidosis, non-specific interstitial pneumonia, organizing pneumonia (both cryptogenic organizing pneumonia and bronchiolitis obliterans organizing pneumonia) pulmonary infections (mainly viral and mycoplasma), malignancies such as bronchoalveolar carcinoma, hemorrhage, pulmonary edema and LP.
Conflict of InterestNone of the named authors have conflicts of interest related to this manuscript.
Please cite this article as: Eisman Hidalgo M, Nuñez-Delgado Y, García Espona MÁ. Hallazgos en la tomografía computarizada de tórax de alta resolución de la neumonía lipoidea idiopática. A propósito de un caso. Arch Bronconeumol. 2014;50:83–84.