Patients with chronic obstructive pulmonary disease (COPD) and chronic respiratory failure have high levels of morbidity and mortality. The clinical efficacy of long term home oxygen therapy has been well documented in this patient group but despite the efficacy of non-invasive ventilation (NIV) during acute decompensated respiratory failure the addition of home NIV has been associated with equivocal results. The physiological efficacy of home NIV to improve gas exchange in chronic stable hypercapnic respiratory failure has been proven in small studies but larger clinical trials failed to translate this into clinical efficacy. Criticisms of early clinical trials include the use of marginally hypercapnic patients and failure to demonstrate effective delivery of home NIV. When considering recent trial data it is important to clearly evaluate the patient phenotype and timing and delivery of NIV. Recent data supports the delivery of home NIV in patients with chronic hypercapnia (PaCO2>7kPa or 50mmHg) and the frequent or infrequent exacerbator phenotype. Importantly in the frequent exacerbator the timing of the assessment needs to be in the recovery phase, 2-4 weeks after resolution of acute acidosis, to delineate transient from persistent hypercapnia. In patient with persistent hypercapnia NIV must be titrated to achieve control of sleep disordered breathing with the aim of improving daytime respiratory failure. Furthermore there are observational data to support the use of home positive airway pressure therapy (NIV or continuous positive airway pressure; CPAP) in patients with COPD and obstructive sleep apnoea (OSA) both with and without hypercapnia.
Los pacientes con enfermedad pulmonar obstructiva crónica (EPOC) e insuficiencia respiratoria crónica tienen morbilidad y mortalidad elevadas. La efectividad de la oxigenoterapia domiciliaria a largo plazo ha sido bien documentada en esta población pero, aunque está demostrada la eficacia de la ventilación no invasiva (VNI) durante la insuficiencia respiratoria descompensada aguda, añadir VNI domiciliaria se ha dado lugar a resultados conflictivos. La eficacia fisiológica de la VNI domiciliaria para mejorar el intercambio de gases en la insuficiencia respiratoria hipercápnica crónica estable se ha demostrado en estudios pequeños, pero ensayos clínicos de mayor tamaño no han logrado mostrar eficacia clínica. Las críticas a los primeros ensayos clínicos comprenden la inclusión de pacientes marginalmente hipercápnicos y la imposibilidad de demostrar que la VNI domiciliaria se administrara correctamente. Al considerar los datos de ensayos recientes, es importante evaluar claramente el fenotipo del paciente y el momento y administración de la VNI. Datos recientes respaldan el uso de VNI domiciliaria en pacientes con hipercapnia crónica (PaCO2>7 kPa o 50 mmHg) y fenotipo de exacerbador frecuente o poco frecuente. Es importante destacar que, en el exacerbador frecuente, la evaluación se debe realizar en la fase de recuperación, 2-4 semanas despuèc)s de la resolución de la acidosis aguda, para diferenciar la hipercapnia transitoria de la persistente. En pacientes con hipercapnia persistente, la VNI se debe ajustar para controlar el trastorno respiratorio del sueño y así mejorar la insuficiencia respiratoria diurna. Además, hay datos observacionales que apoyan el uso de ventilación mecánica domiciliaria con presión positiva (VNI o presión positiva continua en las vías respiratorias, CPAP) en pacientes con EPOC y apnea obstructiva del sueño (OSA) con y sin hipercapnia.
The use of non-invasive ventilation (NIV) to support patients during acute decompensated respiratory failure secondary to an exacerbation of chronic obstructive pulmonary disease (COPD) has unequivocal evidence of benefit in terms of reduction in the need for intubation, length of hospital stay and mortality.1,2 The clinical impact of the treatment effect with acute NIV, coupled with the high levels of morbidity and mortality experienced by COPD patients with chronic hypercapnic respiratory failure,3 provides an appealing clinical rationale for treating such patients with home NIV.
When examining the evidence for home NIV in COPD patients with hypercapnic respiratory failure, it is important to phenotype the patients by (1) the frequency of exacerbations and stability of the clinical condition; infrequent stable exacerbators with low acute hospital admission rate vs. frequent unstable exacerbators with high acute hospital admission rate requiring acute NIV and (2) the presence of co-existent obstructive sleep apnoea, termed COPD-OSA overlap syndrome.
Patients with stable chronic hypercapnia with low exacerbation frequency may have NIV added to standard care and indeed this can be timed to augment the response to pulmonary rehabilitation.4 The addition of home NIV to the high exacerbation frequency and high acute admission group is more challenging. Despite these differences, it is essential to assess and optimise NIV treatment delivery and demonstrate effective management of chronic respiratory failure during initiation and maintenance treatment with NIV.
Delivery of NIV in COPD: How?The optimal approach to deliver effective NIV in COPD has been debated, but there is consensus that overnight physiologically titration of NIV is required to control nocturnal hypoventilation and treat chronic respiratory failure. The use of ‘high intensity tm) NIV in COPD has been reported, but concerns have been raised regarding tolerability and adherence as well as physiological coherence of such a strategy in patients with expiratory airflow limitation. These concerns have been addressed, in part, in a small randomised controlled crossover trial performed in a highly specialist centre [4]. Dreher and colleagues showed that high inspiratory positive airways pressure and high back up rate (‘high intensity tm) NIV) had superior physiological efficacy, reflected as greater control of nocturnal carbon dioxide, compared with low inspiratory positive airways pressure and low back up rate (‘low intensity tm) NIV).5 Whilst greater pressure support is expected to enhance alveolar ventilation and increase carbon dioxide clearance, interestingly, far from ‘high intensity tm) being associated with lower NIV adherence it was, in fact, associated with improved adherence compared to ‘low intensity tm) NIV (mean difference in ventilator usage of 3.6hours; 95%CI 0.6 to 6.7hours, p=0.024). In a subsequent study, the same group of investigators demonstrated that ‘high intensity tm) NIV has a similar effect on sleep disruption as ‘low intensity tm) NIV.6 However, there remain concerns that the ‘high intensity tm) approach may have negative short term cardiovascular consequences7 with the long-term cardiovascular consequences largely unknown.
Although the benefit of a ‘high intensity tm) approach is clear in terms of the management of chronic respiratory failure, it remains unclear if both delivery of high pressure and high backup rate are required. Indeed, the use of ‘high intensity tm) NIV (high inspiratory pressure support and high back up rate) has demonstrated similar benefit as ‘high pressure tm) NIV only (high inspiratory pressure support and low back up rate) in COPD patients.8 Furthermore, the use of a ‘high pressure tm) strategy was associated with greater improvement in respiratory specific health related quality of life over the ‘high intensity tm) approach.8 Finally, a ‘high intensity tm) ventilator strategy requires a slower acclimatisation for patients with a duration of admission of greater than 5 days.5,9
Studies that have failed to demonstrate control of nocturnal hypoventilation, and subsequent failure to improve chronic respiratory failure, have shown limited clinical benefit in COPD patients,10,11 whereas those studies demonstrating improvement in chronic respiratory failure have generally shown a clinical benefit.9,12 This supports the rationale that the major factor when treating chronic respiratory failure in COPD patients is to ensure the treatment is delivered to ameliorate nocturnal hypoventilation and improve daytime gas exchange. The clinical strategy of ‘high intensity tm) or ‘high pressure tm) that is employed to achieve the target of management of chronic respiratory failure is probably less important.
COPD Phenotype: Who and When?Stable Chronic Respiratory FailureDetailed physiological studies have previously demonstrated the mechanism of action of home NIV in stable COPD with chronic hypercapnia.13•15 Until recently, the physiological science has failed to translate to a beneficial clinical outcome in randomised clinical trials. Careful consideration must always be given to the target population, intervention type and delivery, comparator group and the primary outcome when considering trial design. Indeed, a number of the earlier clinical trials investigating the effect of home NIV enrolled stable COPD patients with only borderline hypercapnic respiratory failure with, as expected, limited physiological efficacy demonstrated, which resulted in a lack of clinical benefit.10,11 Furthermore, these early NIV studies failed to show a physiological effect (Table 1) because they employed a ‘low intensity tm) (low inspiratory pressure and low back up rate) ventilator strategy as the intervention.16,17
Comparison of selected trials of domiciliary non-invasive ventilation in COPD.
| Trial Design | NIV settings (IPAP/EPAP Mode Back Up Rate) | Home NIV Titration strategy | Reduction in PaCO2 >0.5kPa in first 6 weeks | Primary outcome | Other reported effects | |
|---|---|---|---|---|---|---|
| Casanova, 200017 | RCT | 12cmH2O/4cmH2O S mode No back up rate | To reduce WOB | No | Mortality (No benefit) | Reduced admission rate |
| Clini, 200210 | RCT | 14cmH2O/2cmH2O S/T mode BUR 8 bpm | To improve nocturnal SpO2 | No | PaCO2 (No benefit) | Reduced self-reported dyspnoea |
| McEvoy, 200911 | RCT | 13cmH2O/5cmH2O S mode No back up rate | To achieve 3hours sleep | No | Mortality (Equivocal) | Worse health related quality of life in the home NIV group |
| Windisch, 200516 | Cohort | 28cmH2O/0cmH2O S/T mode BUR 20 bpm | To maximally tolerated by patient | Yes | Mortality (Benefit) | Non-randomised |
| Kohnlein, 20149 | RCT | 22cmH2O/5cmH2O S/T mode BUR 16 bpm | 20% reduction in PaCO2 | Yes | Mortality (Benefit ARR 21%) | Stable COPD with low admission rate and preserved exercise capacity |
Abbreviations: ARR • Absolute risk reduction; bpm • Breaths per minute; BUR • Back up rate; EPAP • Expiratory positive airway pressure; IPAP • Inspiratory positive airway pressure; NIV • Non-invasive ventilation; PaCO2 • Partial pressure of carbon dioxide in arterial blood; RCT • Randomised clinical trial; S • Spontaneous mode ventilation; S/T - Spontaneous-timed mode ventilation.
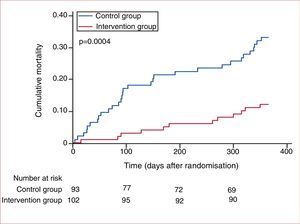
Whilst the lack of clinical effectiveness demonstrated in earlier trials can be attributed to the inappropriate target population and suboptimal intervention delivery, the randomised clinical trial from Kohnlein and colleagues has provided evidence that a moderate inspiratory pressures and back up rate are beneficial in terms of mortality in stable COPD patients.9 Kohnlein and colleagues randomised 195 patients with stable severe COPD (GOLD stage IV) and chronic respiratory failure (PaCO2>7kPa or 53mmHg). Patients were excluded if they had significant co-morbidity, obesity (body mass index, BMI>35kg/m2) or severe heart failure (New York Heart Association, NYHA stage IV). Patients underwent a 4-week run-in period to demonstrate clinically stability and were randomised to home NIV and long-term oxygen therapy (n=102) or long-term oxygen therapy alone (n=93). All patients were admitted to hospital for optimisation of both home NIV and LTOT (intervention) as well as LTOT (control) delivery. Unlike previous studies, the a priori NIV titration protocol was to reduce daytime PaCO2 by>20% or to a PaCO2 below 6.5kPa (49 mmHg). The ventilator settings required were lower compared to earlier reports for ‘high intensity tm) NIV (inspiratory positive airway pressure IPAP 22±5 cmH2O; expiratory positive airway pressure EPAP 5±2 cmH2O; back up rate 16±4 bpm), but achieved significant improvement in chronic respiratory failure. Over the following 1 year follow up period, 33% of control compared to 12% of home NIV and LTOT group died (Hazard ratio 0.24, 95%CI 0.11 to 0.49, p<0.001) [Figure 1]. This impressive treatment effect on mortality was also coupled with benefits in specific (severe respiratory insufficiency questionnaire and St George's respiratory questionnaire) and general (Short form-36 questionnaire) health related quality of life measures. This is of particular importance given the concerns raised by earlier work of impaired quality of life in the NIV and LTOT group compared to LTOT group in the AVCAL trial.11 As a clinician interpreting these data, it is important to understand the target population. The patients randomised had (1) severe COPD (FEV1 28%) (2) chronic respiratory failure (PaCO2 7.7kPa or 58mmHg) (3) stable clinical phenotype with infrequent exacerbations and emergency hospital admissions and (4) preserved exercise capacity (6minute walk test>200m). The results of this clinical trial should be restricted to this COPD phenotype and it would be inappropriate to expand this treatment to include those patients with the frequent exacerbator phenotype with recurrent hospital admission and poor exercise tolerance. In this trial, the clinician should also be cognisant to the fact that acute NIV was withheld from the control population irrespective of pH as long as PaCO2 was less than 10kPa. Furthermore, the cause of death was not reported and thus the proportion of patients dying from decompensated acute respiratory failure was unknown. Irrespective of these caveats, these data represent landmark seminal work for domiciliary NIV and it is the first study to demonstrate a mortality effect of the therapy.
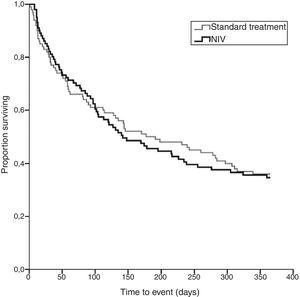
Post-acute exacerbation of COPDThe prognosis of patients who have acute exacerbations of COPD, complicated by decompensated acute respiratory failure with persisting hypercapnia, is poor.18 Previous small studies have suggested a potential benefit in reducing readmission rate when home NIV was added to LTOT.19,20 However, two recent randomised control trials focussed on this post-acute target population providing contrasting results. Struik and colleagues conducted a multi-centre randomised clinical trial in the Netherlands (RESCUE study)21 and recruited patients with hypercapnia 48hours after cessation of NIV for an acute exacerbation of COPD. In contrast to the Kohnlein study, these patients were the frequent exacerbator phenotype with a poor exercise tolerance, albeit the walk test distance was not reported as failure to complete the test was high. The patients had severe COPD (FEV1 26%) and hypercapnia (PaCO2 7.7kPa or 58mmHg). They were randomised to moderate pressure NIV in addition to LTOT (n=101; IPAP 19±3 cmH2O, EPAP 4±1 cmH2O, backup rate 15±3) or LTOT alone (n=100). There was no difference in the primary outcome of admission-free survival [Figure 2] and, furthermore, the extended period of recruitment required for trial completion enabled a detailed mortality analysis but, again, there was no benefit of NIV in addition to LTOT. The cause of death in the majority of patients was of a respiratory cause. Although Struik and colleagues were able to demonstrate physiological efficacy and control of nocturnal hypoventilation with improvement in respiratory failure in the home NIV and LTOT group, there were similar improvements in PaCO2 in the LTOT group. The resolution of hypercapnia during early recovery requires careful consideration as this had a role, in part, in reducing the physiological and clinical effect of home NIV. Indeed, the target population had hypercapnia assessed at the cessation of NIV therapy during an acute admission. Previous data have shown that those patients with reversible acute hypercapnia, with resolution to a eucapnic state during the recovery phase following an exacerbation, have (1) a similar prognosis to patients who were eucapnic during their acute episode and (2) a superior prognosis to those who have chronic persistent hypercapnia following recovery from the acute episode.22 Importantly, home NIV and LTOT has less physiological and clinical effect in patients with the reversible hypercapnic phenotype as these patients do not have chronic respiratory failure.
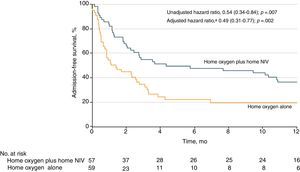
More recently, the results of the HOT-HMV UK study were reported. This multicentre clinical trial investigated the effect of home mechanical non-invasive ventilation (HMV) and home oxygen therapy (HOT) on admission-free survival in patients with severe COPD and persistent hypercapnia (PaCO2>7kPa or 53mmHg) in the extended recovery phase following an acute life threatening exacerbation.23 The study population had severe airflow limitation (FEV1 23%), persistent hypercapnia (PaCO2 7.9kPa or 59mmHg) when evaluated at 2 to 4 weeks post-resolution of hypercapnic acidosis. Patients were excluded if they had morbid obesity, obstructive sleep apnoea, respiratory decompensation following initiation of oxygen therapy or had significant life limiting co-morbidity. Patients were randomised to HOT (n=59) or HOT-HMV (n=57). The HOT-HMV group had NIV titrated to control nocturnal sleep disordered breathing targeting nocturnal transcutaneous CO2 with moderately high pressure NIV delivered (IPAP 24 [22-26] cmH2O, EPAP 4 [4-5] cmH2O, backup rate 14 [14-16]). Over the 1 year follow up, the intervention arm had a delay in time to death or first readmission (adjusted hazard ratio 0.49, 95%CI 0.31 to 0.77, p=0.002; median time to event HOT 1.4 months vs. HMV 4.3 months) [Figure 3]. As would be expected in this group of patients the majority of readmissions were respiratory in nature. Over the 12 months of the study there was no significant effect on mortality, although the trend favoured the HOT-HMV arm (adjusted hazard ratio 0.67, 95%CI 0.34 to 1.30, p=0.232). As well as a reduction in time to first admission or death there was a reduction in annual exacerbation frequency (HMV 3.4 [1.7 to 6.0] exacerbations per year vs. HOT 5.1 [1.0 to 9.2] exacerbations per year; adjusted hazard ratio 0.66, 95%CI 0.46 to 0.95, p=0.026). There was no evidence of a negative effect of home NIV on quality of life with measures either indicating equivalence or mild improvement in quality of life in the HOT-HMV arm. The main criticism of the trial design was the lack of use of a sham intervention, although this is consistent with other trials in this area. In addition the trial required an extension in order to reach the recruitment target; when examining the reasons for non-randomisation significant numbers were treated with NIV on clinical grounds due to other indications for NIV (e.g. obesity, OSA or acute decompensation with oxygen therapy) or were unable to consent for the trial, stressing the importance of prospectively following up these patients to assess for persistent hypercapnia. In terms of streamlining the patient flows in clinical practice, the clinician should remember that almost 50% of the patients had resolution of hypercapnia at 2-4 weeks post resolution of respiratory acidosis. This allows stratification of the high risk of readmission from the low risk of readmission COPD patients.
In conclusion, the data would strongly support the assessment of COPD patients admitted with an episode of decompensated respiratory failure requiring acute NIV at 2-4 weeks following resolution of respiratory acidosis. If at 2-4 weeks, the patient has persistent hypercapnia then home NIV should be added to home oxygen therapy. The clinician would have to treat only 6 patients to prevent 1 readmission to hospital with and accompanying reduction in exacerbation rate and 28-day readmission.
Future considerations: Home NIV or CPAP in COPD-OSA overlap syndromeIn the three recent trials investigating the clinical effectiveness of home NIV in COPD, the presence of morbid obesity and sleep apnoea have been exclusion criteria.9,21,23 The consensus is that such patients benefit from positive airway therapy based on clinical trial data from obesity related respiratory failure cohorts, including OSA and obesity hypoventilation syndrome.24•26 This is also supported by observational data in COPD-OSA overlap syndrome.27 COPD-OSA is of growing concern and indeed the prognosis of patients with COPD-OSA overlap, in terms of exacerbation frequency and mortality, has been shown to be worse than in patients with uncomplicated OSA.27 Furthermore, there appears to be an amelioration of this risk with treatment with CPAP compared to patients who decline or are non-compliant with therapy. A dose response effect has been shown, with a compliance of less than 2hours per night conveying a poorer prognosis than patients achieving higher levels of compliance.28 Previous data has suggested that the mortality benefit is restricted to those COPD-OSA patients who with chronic respiratory failure,29 although the exact number of patients with hypercapnia in previous studies has been unclear. Worthy of note is that in each of the studies examining the effectiveness of CPAP in COPD-OSA, the non-compliance rates were approximately 50% with these non-compliant patients used as control subjects.27,29 As expected, this clearly limits the generalisability of the data as non-compliant patients may have different disease severity and make poor health care choices, which influence their outcomes compared to compliant patients.30 Quality of sleep in COPD is related to the degree of hyperinflation31 and the severity of hyperinflation may exacerbated by application of high pressure CPAP as this will worsen expiratory flow limitation. Indeed, application of high pressure CPAP during the daytime has been shown to be associated with worsening breathlessness,32 which in dyspnoeic COPD may be associated with poor CPAP tolerance. Few data exist to guide the choice of therapy in these patients with guidelines advising against the use of auto-titrating devices and advocating the use of inpatient attended titration. The major concern with auto-titrating devices is that the presence of expiratory flow limitation, due to lower airway obstruction rather than upper airway closure, could result in inappropriate up-titration of CPAP pressure due to misinterpretation by the flow based algorithm of the devices. The use of novel auto-titrating devices which use advanced technology rather than flow wave analysis to detect upper airway occlusion may overcome the difficulties with inappropriate over pressurisation with previous observational data demonstrating that a novel comprehensive auto-titrating device (Auto-IPAP, Auto-EPAP and Auto-backup rate) can safely and effectively control sleep disordered breathing in patients with hypercapnic COPD-OSA with improved NIV comfort and compliance.33
SummaryThere is now evidence to support home NIV as an important tool in the management of patients with advanced severe COPD with chronic respiratory failure. These patients require detailed clinical phenotyping to identify treatable characteristics to maximise the clinical effectiveness of home NIV. COPD patients with chronic respiratory failure (PaCO2 above 7kPa or 53mmHg), in either the recovery phase from a life-threatening exacerbation or in the chronic stable state should be considered for treatment with home NIV and oxygen therapy. The home NIV should be titrated as an inpatient to control nocturnal hypoventilation with a moderate high inspiratory positive airways pressure approach. Based on current evidence, those patients with COPD-OSA overlap syndrome and chronic respiratory failure should be established on home NIV.
Competing InterestsThe Lane Fox Clinical Respiratory Physiology Research Centre has received unrestricted research grants from ResMed, Abingdon, Oxfordshire, UK; Philips-Respironics, Murrysville, PA, USA; Fisher & Paykel Healthcare, Auckland, New Zealand and B&D ElectroMedical, Stratford-upon-Avon, Warwickshire, UK. PBM has received expenses for travel to conferences, hospitality and lecturing from Philips-Respironics, ResMed, Fisher & Paykel and B&D Electromedical. NH has received fees for lecturing from Philips-Respironics and Fisher & Paykel.