Chronic obstructive pulmonary disease (COPD) exacerbation increases mortality and resources used associated with hospitalization. We studied whether early home monitoring reduces the rate of readmission and if there are any predictor variables.
Patients and methodsWe performed a prospective, controlled, parallel-group study in patients who were hospitalized for COPD. Patients whose residence was within less than 15km from the hospital were assigned to an interventional group (home visits by nurses about 48–72h after discharge), the remaining patients were assigned to a conventional care group. The rate of rehospitalization within the first month was compared between the 2 groups, as well as those variables that showed a predictive capability.
ResultsSeventy-one patients were included: 35 in the conventional care group and 36 in the interventional group. In the latter, the treatment was modified in 13 patients (36%). The hospital readmission rate was 17%, which was similar in both groups (P=.50). For every 5-year increase in age, the risk for readmission was 2.54 (95%CI 1.06–5.07) and for each increase of 10mmHg in PaCO2, the risk of readmission was 8.34 (95%CI 2.43–18.55).
ConclusionsEarly home monitoring did not decrease the readmission rate during the first month. Older age and high PaCO2 are factors that identify the group with a high risk for rehospitalization.
La enfermedad pulmonar obstructiva crónica (EPOC) agudizada aumenta la mortalidad y los recursos asociados con la hospitalización. Se estudia si un control domiciliario precoz disminuye la tasa de reingresos y si existen variables que puedan predecirlo.
Pacientes y métodosSe realiza un estudio prospectivo, controlado en grupos paralelos en pacientes ingresados por EPOC. Los pacientes que residían a menos de 15km del hospital fueron asignados a un grupo de intervención (visita domiciliaria por una enfermera en las 48–72h tras el alta) y los restantes a un grupo de cuidados habituales. Se compararon en ambos grupos la tasa de reingresos hospitalarios en el primer mes y las variables capaces de predecirlo.
ResultadosFueron incluidos 71 enfermos, 35 en el grupo de cuidados convencionales y 36 en el grupo de intervención; en este último se modificó el tratamiento en 13 sujetos (36% de los enfermos). La tasa de reingreso fue del 17%, siendo similar en ambos grupos (p=0,50). Por cada aumento de 5 años en la edad, el riesgo de reingreso fue de 2,54 (IC 95%, 1,06 a 5,07) y por cada incremento de 10mmHg en la PaCO2, el riesgo de reingreso fue de 8,34 (IC 95%, 2,43 a 18,55).
ConclusionesEl control domiciliario precoz no disminuyó la tasa de reingresos durante el primer mes. Una mayor edad y una PaCO2 elevada son factores que identifican a un grupo con elevado riesgo de reingreso.
Chronic obstructive pulmonary disease (COPD) is characterized by reduced airflow that is not totally reversible, generally progressive and associated with an inflammatory response of the lungs to toxic particles and gases, especially from tobacco, which shows important systemic repercussions.1,2
The prevalence of COPD is high. The EPI-Scan study observed that 10.2% of the general population in Spain aged between 40 and 80 has COPD.3 Due to the increase in smoking and the change in the age pyramid in developed countries, an increase in the incidence and prevalence of COPD is foreseen. It has been predicted that by the year 2020 COPD will be the third cause of death worldwide.
Patients require medical attention in advanced stages of the disease, generally with the appearance of exertional dyspnea that limits their daily activities or exacerbations. This is the cause of the decline in quality of life and increase in mortality. The result is first-rate health-care problem due to the increased health-care load and high consumption of resources.4 This aspect is directly related with hospitalization, which represents approximately 45% of the total expense.1,5 It is therefore important to identify and treat patients with repetitive exacerbations, since they represent only 12% of patients but 57% of hospitalizations and close to 60% of ER visits.6 Furthermore, these cases entail different treatment and prognostic repercussions.2
Exacerbations are a good opportunity to recruit patients in a health-care education program involving home treatment and continuous care, while avoiding hospital readmittance.1,2,7 To meet this objective, it is essential for there to be coordination between the different health-care levels as well as technical and human resources to facilitate home care. These are aspects that make such studies so scarce in our setting.
Nonetheless, new technologies currently provide real-time transmission of clinical and functional data from the patients’ residences to the hospital. In addition, patients with recent hospitalization have data available that can be very useful for making clinical decisions in emergency situations.
For these reasons, we designed a study that included patients who had been hospitalized due to COPD in order to determine, first of all, whether home follow-up of patients by a nurse and telephone support with a pulmonologist could reduce the rate of readmittance in the 4 weeks following hospital discharge. Secondly, we aimed to determine whether at the time of hospital discharge it is possible to determine clinical variables that could help predict readmittance.
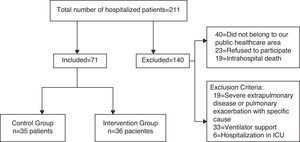
Patients and MethodsStudy DesignOur study is a controlled clinical assay in parallel groups of patients hospitalized due to COPD designed to assess the effectiveness of early home intervention. During hospitalization, the patients were stabilized in the Pulmonology Unit following accepted clinical practice guidelines, and upon discharge they were assigned to one of the study groups (Fig. 1). The study was authorized by the Ethics and Research Committee of the Hospital.
Patient SelectionIncluded in the study were consecutive patients with COPD exacerbations who were admitted to the Pulmonology Unit at a tertiary hospital following the accepted criteria for clinical practice,1,7 aged <75 and belonging to our regional public healthcare area. Excluded from the study were those patients with severe comorbidity (grade IV heart failure and renal failure with hemodialysis) immunosuppression or specific exacerbation cause (pneumonia, pneumothorax, thromboembolic disease, heart failure), ventilatory support or admittance in the ICU, or if the patient could not be contacted by telephone.
Before hospital discharge, we explained to patients the standardized treatment plan (Appendix A) and scheduled follow-up, and they gave their written informed consent in order to participate in the study. Likewise, the following data were recorded: baseline clinical data, comorbidity measured by the Charlson index, the degree of dyspnea according to the Borg scale, arterial blood gas and FEV1 (forced expiratory volume in the first second) levels. This was measured with a portable device (Vitalograph® Ltd., Buckingham, England) in order to be able to be used at the patients’ homes. All patients and their caretakers were informed about the standard recommendations and guidelines to follow in cases of exacerbation in our regional healthcare area.7
The present study was done in standard clinical practice conditions. Due to logistic reasons involved in the nursing staff's going to patients’ homes, the patients were classified according to distance from the hospital.
Intervention: The intervention group included the patients who resided in the city within 15km of the hospital. After discharge, they were assessed within the first 48–72h in their homes by a nurse who supervised adequate treatment compliance (including inhalation techniques), recorded clinical information, measured SapO2 and carried out spirometry. These data were sent to the pulmonologist in real time, who was able to make a phone call to change the treatment if the results required it. Patients living more than 15km away from the hospital were assigned to the control group. These patients were controlled by the Primary Care Team following the criteria established in our health-care setting.7,8 All the subjects were instructed that, if their symptoms worsened, they should consult with their Family Physician or go to the hospital emergency room.8 After 4 weeks, all the patients were assessed in the outpatient clinic of the Pulmonology Department.
The results variable was a new hospitalization due to COPD exacerbation. We did not analyze the number of exacerbations that did not require hospitalization due to the difficulty to unequivocally determine this variable.
Statistical AnalysisThe quantitative variables were expressed as mean±standard deviation and the qualitative variables in absolute variables and percentages. The comparison of means between the study groups was done using Student's t-test for independent samples; for the qualitative variables, we used the χ2 or Fisher's exact test if an expected frequency was less than 5.
In order to assess whether in the total group of hospitalized subjects there were variables associated with rehospitalization, first of all, univariate logistic regression analyses were done with each of the following variables: group, age, number of previous hospitalizations, antibiotic treatment more than 3 times a year, BMI, GOLD grades 3 and 4 (Global Initiative for Chronic Obstructive Pulmonary Lung Disease), Charlson index, Tabaco consumption, and data upon discharge: dyspnea (Borg), PaO2, PaCO2 and FEV1. In the multivariable model, we used those variables that had shown statistical significance of less than .25; with the Wald statistic, the variables with a P greater than .15 (backward selection method) were eliminated one by one from the model; the Hosmer–Lemeshow statistic was used to assess the goodness of fit and the area under the curve in order to determine the discriminating capacity of the model, and the Box–Tidwell procedure was used to assess the linear scale of the quantitative variables.
The PASW 18 (Predictive Analytic Software) statistical package was used, and for all statistical tests P values <.05 were considered statistically significant and the hypothesis contrasts were bilateral.
ResultsDuring the study period between October 2010 and November 2011, a total of 211 patients were hospitalized due to severe COPD exacerbation. The study flowchart is shown in Fig. 1. The characteristics of the patients of both groups are shown in Table 1. As can be observed, there were no significant differences between the groups for age, sex, smoking, degree of dyspnea, Charlson index, previous hospitalizations in the previous year and severity according to the GOLD classification. The only difference was that the patients in the intervention group had a lower body mass index (BMI) with a tendency toward significance (P=.06).
Baseline Characteristics of the Patients Prior to Hospitalization. The Quantitative Variables are Expressed as Mean±Standard Deviation, and the Qualitative as Absolute Frequency and Percentage.
| Variables | Intervention Group | Control Group | P Value |
| Age, years | 60±9.3 | 59±7.4 | .87 |
| Sex, female | 2 (5%) | 1 (3%) | .97 |
| Body mass index, kg/m2 | 28.5±4.8 | 30.6±5.2 | .06 |
| Smokers, n, % | 14 (39%) | 14 (40%) | .98 |
| Baseline dyspnea, 3–4 (MRC) | 16 (50%) | 12 (34%) | .18 |
| GOLD grades 3–4 | 20 (55%) | 23 (66%) | .39 |
| Charlson index (%) | 2±1 | 1.7±0.8 | .19 |
| Antibiotic >3 times a year | 19 (59%) | 21 (60%) | .90 |
| Previous hospitalizations | 0.8±0.76 | 0.5±0.7 | .18 |
| Inhaled corticosteroids, n, % | 31 (86%) | 25 (74%) | .11 |
| SABA, n, % | 14 (39%) | 12 (34%) | .44 |
| LABA, n, % | 31 (86%) | 26 (74%) | .17 |
| Ipratropium, n, % | 2 (5%) | 4 (11%) | .32 |
| Tiotropium, n, % | 24 (66%) | 21 (60%) | .37 |
MRC, Medical Research Council; GOLD, Global Initiative for Chronic Obstructive Pulmonary Lung Disease; SABA, short-acting beta agonist; LABA, long-acting beta agonist.
It should be emphasized that 21% (15/71) of the subjects had been hospitalized in the 3 months prior to inclusion in the study, 7 of them belonging to the intervention group and 8 in the control group. In addition, 59% (42/71) of the total number of patients included had taken more than 3 rounds of antibiotics over the course of the previous year (20 subjects from the intervention group and 22 in the control group). As for treatment, a high percentage of inhaled corticosteroids and LABA (Long-Acting Beta Agonists) was recorded, although with similar levels in both groups, probably due to the frequent association of both drugs. At the time of hospital discharge, dyspnea grade, FEV1 and arterial blood gas values were similar in the 2 groups (Table 2).
Values at Hospital Discharge. Data Are Expressed as Mean±Standard Deviation.
| Variables | Intervention Group | Control Group | P Value |
| Hospital stay, days | 10±4 | 9±4 | .34 |
| Dyspnea (Borg) | 5.7±1.1 | 5.5±1.1 | .81 |
| FEV1, % | 40.4±16.4 | 45.7±19.6 | .15 |
| PaO2, mmHg | 51±8.3 | 51±8 | .88 |
| PaCO2, mmHg | 49±13.1 | 47±15.9 | .67 |
| pH | 7.39±0.02 | 7.37±0.06 | .57 |
During the home visit by a nurse and with the telephone support of a pulmonologist, a total of 13 interventions (36% of patients) took place. In 4 cases the diuretic dose was increased, in 2 an antibiotic was either prescribed or changed, in 2 the oral corticosteroid dosage was increased, in 2 oral theophylline was withdrawn due to gastric intolerance, and lastly, in 3 patients the oxygen supply was increased in order to maintain SapO2 between 89% and 91%.
During the 4 weeks following discharge, there were 12 hospital readmittances (17%) due to exacerbated COPD: in 4 cases in the first 2 weeks and the remainder in the following two. In the intervention group there were 5 readmittances, 16% of the total of 32 subjects of the group, while in the conventional care group there were 7 readmittances (20%). Thus, the rate of rehospitalization was similar in both groups (P=.50). During the study period, there were no deaths of included patients.
In order to assess whether in the total group of subjects who were hospitalized there were variables associated with readmittance, a multivariate analysis was done and variables that showed statistical significance were input into the model (age, BMI, PaCO2, PaO2, FEV1, dyspnea upon discharge (Borg) and GOLD classification. The results are shown in Table 3.
Factors Associated With Readmittance in the First 4 Weeks After Hospital Discharge.
By eliminating those variables that did not influence the model, only older age and higher PaCO2 were the variables that were independently associated with hospital readmittance.
For every increase of 5 years in age, the risk for readmittance was 2.54 (95%CI 1.06–5.07) and for every increase of 10mmHg in PaCO2, the risk for readmittance was 8.34 (95%CI 2.43–18.55)
DiscussionThe study included patients admitted for COPD exacerbation in a Spanish tertiary hospital. In this context, in addition to conventional care, the patients received home visits from a nurse and telephone support by a pulmonologist for early detection, but the rate of readmittance during the 4 weeks following discharge did not decrease. Nonetheless regardless of the group that the patients belonged to, those who were older or had a higher PaCO2 at the time of the hospital discharge were more likely to be readmitted. While later validation is still needed, this finding is clinically interesting as it could identify a subgroup of fragile patients with accessible clinical information (age and hypercapnia) in whom medical controls should be reinforced in order to reduce the number of rehospitalizations.
The period immediately after hospital discharge is a stage of clinical instability that is crucial for avoiding new exacerbations. Different strategies have been established to avoid them,8 including hospital care programs for early discharge and later home control9,10 and others based on patient self-management or caretaker care.11 Studies that analyze early intervention after hospital discharge are less frequent.12,13
Early treatment in exacerbations can be associated with faster recuperation and less risk for exacerbation. Models have been published to improve the access to information based on 24-h telephone support. Robert et al.14 showed that this intervention was cost-effective based on the reduction of hospital visits; however, only one-fourth of the patients used this service, with a predominance of patients who lived with family members and had more severe disease. Recently, a study for treating high-risk COPD patients has shown promising preliminary results.15 Nevertheless, our intervention was done in subjects who were hospitalized for COPD and required distinct health-care management.14,15 In our study, an early therapeutic intervention did not lower the number of readmittances. If the home visits and telephone contact were maintained over a long period of time, this objective would likely have been achieved.13
In this study, it must be kept in mind that the Primary Care Team reviewed the patients after hospital discharge and can affirm that the results were similar in both groups.
To evaluate COPD prognosis, multidimensional models have been used that have demonstrated their validity in clinical stability16,17 and, together with other newer models, may be applicable to exacerbations.18 Among these, one frequently cited model is indication of antibiotic therapy due to exacerbation in the previous year.8 In our cohort, up to 60% of patients were prescribed more than 3 cycles of antibiotics during the previous year and 20% had been hospitalized in the last 3 months, so they therefore belong to a fragile group with special risk for new hospitalizations.8,19 In fact, our patients had a mean of nearly 1 hospitalization in the previous year, with a predominance of GOLD functional grades 3 and 4. In this clinical context, the number of previous hospitalizations was not independently associated with hospital readmittance. In this population of severe patients with frequent exacerbations, a relatively simple, single early home intervention is not effective, and it may be necessary to increase the intervention time to meet the objetive.13
Another of the prognostic markers used is hypoxemia determined in the emergency room, although these data are a reflection of the severity of the acute disease and is therefore more closely related with hospital mortality.20,21 This is why PaO2 was measured and recorded upon hospitalization, but in our study these data did not contribute to predicting the following exacerbation. A similar result was observed in FEV1 measured in the same day of the discharge, which, however, is a good predictor for mortality in clinical stability.16 Although it has been reported that BMI is associated with mortality in COPD patients (both stable and exacerbated22,23), in this present study it did not influence the rate of readmittances. This result has been described in other studies that show that BMI is not always an independent predictive factor for exacerbation.20,21,24,25
There are reports of increased relative risk for mortality attributable to ages over 70.26,27 Nevertheless, in our population with a mean age of 60, those who were older had a greater risk for readmittance, which agrees with the results of other authors.28,29 Likewise, a greater level of PaCO2 increased the possibilities of a new hospitalization. Hypercapnia at the time of hospital discharge probably better reflects severe respiratory failure that has exhausted compensation mechanisms, a reason why it is associated with long-term mortality and also increases the risk for hospitalization.20,21
The present study, done in standard clinical practice conditions, presents some limitations. Among these is the impossibility to randomize the patients due to the difficulties entailed in visiting some patients’ homes. Nevertheless, we opted for a quasi-experimental assignation as the patients were only assigned depending on the possibility of making a home visit. This circumstance did not influence the results. The shorter distance of the patients to the hospital might have facilitated office visits and hospitalization, but this aspect was not significant in our study. We did not analyze the conventional care provided by Primary Care teams due to the difficulty to determine this care reliably in each of the patients of the control group. Nonetheless, it is possible that it was not that different from the care given by our group, which would partially explain the results. Lastly, it must be kept in mind that these results are applicable to our healthcare region and the characteristics of our patients. Therefore, they are not valid for excluded patients, meaning those with a greater degree of comorbidity and those requiring ventilatory support or admittance in the ICU.
In short, early home intervention, including nurse visits and telephone support with a pulmonologist, did not reduce the rate of readmittances in the first 4 weeks. Until the inclusion of new drugs, it is possible that the current therapeutic ceiling has been reached; thus, it is necessary to advance in strategies that involve patients and their caretakers while connecting them with the medical team. Telephone support or other models based on telemedicine are promising advances, but their actual roles need to be established. Nonetheless, these results have practical repercussions as, in patients who had previously been hospitalized for COPD, the variables with the greatest influence for predicting rehospitalization were older age and high PaCO2.
FundingPartially funded by Asociación Neumocor and Boerhringer Ingelheim, Spain.
Conflict of InterestsThe authors declare having no conflict of interests.
The authors would like to thank the nursing staff of the Linde Medicinal group.
- -
Check that the inhalation maneuver is being done correctly.
- -
Bronchodilator treatment: using a combination of tiotropium together with a long-acting beta2-agonist and an inhaled corticosteroid, at the following dosage:
Tiotropium, 1 inhalation every 24h. Salmeterol 50μg plus 500μg fluticasone every 12h or formoterol 9μg and 320μg of budesonide every 12h.
- -
Oral antibiotic according to Anthonisen criteria)
- -
Oral corticosteroids: 40mg of methylprednisolone every 24h (or equivalent dosage of another corticosteroids), decreased by 10mg every 3 days until suspension
- -
Supplemental oxygen (if necessary)
- -
Low-molecular-weight heparin (if necessary)
- -
Other (specify active ingredient and dosage).
Please cite this article as: Jurado Gámez B, et al. Intervención domiciliaria y variables predictoras para reingreso hospitalario en la enfermedad pulmonar obstructiva crónica agudizada. Arch Bronconeumol. 2012;49:10–4.