Acute non-cardiogenic pulmonary edema consists of the rapid appearance of alveolar edema for causes other than increased pulmonary capillary pressure.1 One of the etiologies of this entity is acute high-altitude pulmonary edema (HAPE), an uncommon but potentially fatal presentation (50% mortality in untreated patients).
It is one of the so-called “altitude sicknesses”, the benign form of which occurs in 75% of the population exposed to an altitude of between 2500 and 3000m, manifesting as symptoms such as nausea, vomiting, asthenia, anorexia, headache, dizziness, sleep disturbances or even dyspnea. The malignant form is less frequent, and develops with acute pulmonary edema and/or cerebral edema syndrome.2
We report the case of a 40-year-old white man with no significant clinical history, regular athlete, former smoker, normally resident at about 11m above sea level, who had ascended to Sierra Nevada (maximum height 3300m) in less than 3h. He skied intensively for a 48h period before experiencing a feeling of tiredness that forced him to interrupt his activity.
He notified the emergency department of the ski resort of symptoms of sudden dyspnea, more intense in the supine position, and cough with bubbly pinkish expectoration. On arrival in the medical center, the patient was normotensive, with signs of hypoperfusion and cyanosis, tachycardiac at 120bpm, tachypneic (>30 breaths/min), with SatO2 of around 90% and FiO2 of 0.6 with work of breathing and low-grade fever of 37°C. Auscultation revealed moist rales, mainly in both lung bases. ECG showed sinus tachycardia at 110bpm with normal axis along with the ST depression in the inferior and anteroseptal aspects. After administration of empirical treatment (oxygen therapy by reservoir cannula with FiO2 of 1.0, furosemide, acetylsalicylic acid and antibiotic coverage), the patient was transferred to the tertiary hospital.
On arrival at the hospital, arterial blood gases (FiO2 0.6) were determined, showing normal pH, oxygen partial pressure of 69.9mmHg, and normal carbon dioxide and lactic acid. Clinical laboratory tests were significant for slightly raised CRP and leukocytosis with neutrophilia, with normal D-dimer and cardiac markers.
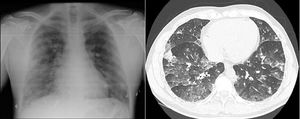
Chest X-ray showed a normal cardiothoracic index with a bilateral reticular cotton–wool pattern with no central predominance (Fig. 1). The CT-angiogram ruled out pulmonary thromboembolism and concluded findings indicative of acute pulmonary edema. Alveolar opacities and ground glass opacities were also observed, with a symmetrical, generalized distribution in the parenchyma of both lungs, slightly more predominantly in the lower lobes, which showed thickening of the interlobular septa and a significant increase in pulmonary arterial trunk diameter (35mm) (Fig. 1).
Transthoracic echocardiogram showed signs of pulmonary hypertension with slight tricuspid insufficiency and an estimated 70mmHg systolic pressure in the pulmonary artery, without pericardial effusion.
The patient was admitted to the ward, and his oxygen requirements decreased progressively in the first 24h. Treatment continued with the patient placed in a sitting position, receiving low-flow oxygen therapy (nasal prongs at 2l/min), and minimum-dose furosemide. After 3 days of hospitalization, he was completely asymptomatic at discharge. Follow-up echocardiography and cardiopulmonary exertion test one year later were both normal.
HAPE generally occurs within 2–5 days after arrival at high altitudes, and around 50% of cases are associated with acute mountain sickness. High altitude is considered to be between 1500 and 3700m, 3700–5500m very high (the incidence of HAPE at this altitude is 0.6–6%), and >5500m extreme (2–15%).3
Onset of clinical symptoms is insidious, with decreased exercise tolerance, progressive dyspnea, orthopnea, wet cough, hemoptysis, chest pain, headache, and confusion.3,4 Saturation is estimated to be 10% lower than expected according to the altitude, and the patient's general status is usually better than expected from their level of hypoxemia.4
The main risk factor is individual susceptibility due to a low hypoxic ventilatory response.5The risk factor most susceptible to modification is the rate of ascent,6 and altitude gained during sleep is more significant than that gained during the day. Other factors include the intensity of the exercise (more than the exercise itself), male sex, anxiolytic medication, and low temperatures. A previous episode of HAPE carries a risk of recurrence of 60%, so it is very important that the patient is warned. A gradual ascent of about 500m per day to levels above 2500m allows the physiological processes in the body to compensate adequately for the reduced partial pressure of oxygen at the new altitude. Avoiding exercise and alcohol during the first 48h until acclimatization also minimizes the risk. Pre-existing conditions that lead to increased pulmonary blood flow, such as pulmonary hypertension, increased pulmonary vascular reactivity, or a patent foramen ovale, are predisposing factors for the appearance of the HAPE.
The key factor in the pathophysiology of the disease is the initial adaptation to altitude, in which the individual will typically increase ventilation. Activation of the pulmonary and cerebral hypoxic vasoconstriction reflex results in an exaggerated vasoconstriction response, raising pulmonary artery systolic pressure.3 The subsequent transudative capillary leak and the increase in perfusion increase blood pressure and hydrostatic pressure, causing damage to the alveolar–capillary barrier, and ultimately, increased vascular permeability leading to acute, non-uniform pulmonary edema.
Treatment consists of oxygen therapy and descending around 1000m or to a level where symptoms resolve, minimizing exertion during the descent. Pharmacological treatment mentioned in the literature includes vasodilators, such as nifedipine (dihydropyridinic calcium channel blocker antagonists)4 or sildenafil,3 phosphodiesterase inhibitors,4 and dexamethasone. Acetazolamide is also used as a treatment because it creates alkalemia, which leads to increased ventilation by increasing the arterial oxygen content of blood, and study is ongoing into its prophylactic use for ascents to more than 2700m.3,6,7 Potential new therapies, such as ibuprofen, nitrates, and intravenous iron supplements are recommended.3
Please cite this article as: García Flores PI, Caballero Vázquez A, Herrera Chilla Á, Romero Ortiz AD. Edema agudo de pulmón por altura tras 48 horas de estancia en una estación de esquí. Arch Bronconeumol. 2019;55:107–108.