Radiofrequency ablation is an effective procedure for patients with paroxysmal atrial fibrillation refractory to treatment with anti-arrhythmic drugs.1 Its use is increasingly widespread, with some 40000–50000 procedures performed annually in the United States. One of the most commonly described serious complications is pulmonary vein stenosis, which presents in up to 1%–3% of cases.
We present the case of a 49-year-old male, ex-smoker, with a history of hypertension and thrombotic thrombocytopenic purpura resolved with plasmapheresis and prednisone. He had undergone pulmonary vein ablation in another hospital due to paroxysmal atrial fibrillation. After remaining asymptomatic for 2 years, he was admitted to our centre for study after presenting 2 episodes of spontaneous haemoptysis, as well as dyspnoea on moderate exertion. A complete blood count, coagulation study, basal arterial blood gases, electrocardiogram, chest radiograph and autoimmunity study were carried out, but did not show any noteworthy abnormalities.
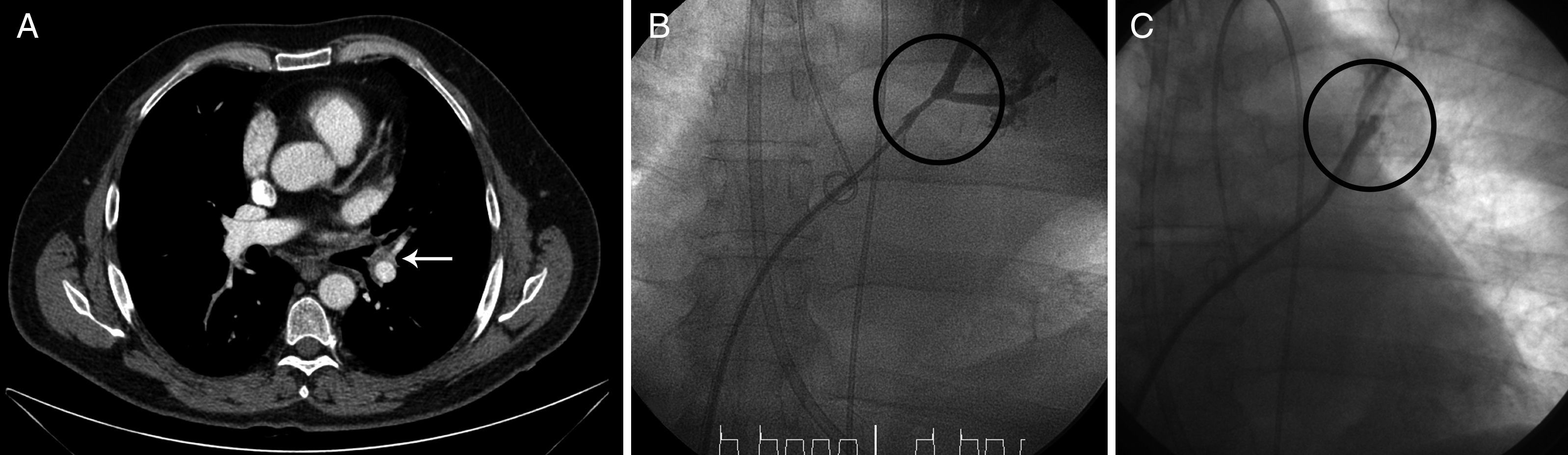
In the chest computed tomography (CT) study, a “cuff-like” soft tissue lesion with peribronchovascular distribution was identified in the left upper lobe, which was initially interpreted as a possible tumour (Fig. 1A, arrow). Although there was clinical suspicion of pulmonary vein stenosis as the cause of the haemoptysis, due to the radiological finding, it was decided to perform bronchoscopy with a flexible endoscope to take a biopsy in order to exclude a tumour at that level; the bronchoscopy revealed a mucosa with petechiae which bled easily as the bronchoscope passed. During the procedure, the patient experienced major bleeding from the left main bronchus, which required selective orotracheal intubation of the right main bronchus and transfer to the intensive care unit.
A pulmonary angiography was performed, showing stenosis of the left upper pulmonary vein (Fig. 1B, in which a decrease in the vascular calibre can be observed at the level of this vein). Balloon angioplasty was then performed at this level, achieving repermeabilisation, with subsequent good angiographic results (Fig. 1C). After the patient had been stabilised and then discharged, he was admitted on a scheduled basis 2 months later for angioplasty with stent placement.
Haemoptysis has been described in the literature as a rare form of presentation of pulmonary vein stenosis,2 but the aetiopathogenesis of the haemoptysis in these patients has not yet been clarified. Aguilar-Cabello et al.3described a similar case in which histopathological examination of a lobectomy sample showed congested lung tissue. The increase in venous pressure in the pre-stenotic zone would explain the lung tissue congestion and the risk of bleeding at the level of the mucosa in this area. In our patient, the image observed initially on the chest CT scan (Fig. 1A) appears to correspond to oedema and peribronchovascular fibrosis secondary to congestion due to thrombosis of the vein. This radiological finding may help to understand the pathophysiology a little more, and serve as a reference to help other clinicians to support the diagnosis of this entity.
Pulmonary vein ablation is a relatively safe procedure, although it is not free of complications. Among the late complications of this procedure are: cardiac tamponade, pulmonary vein stenosis, embolisms, vascular complications, phrenic nerve lesion, gastro-oesophageal fistula and gastric hypomotility secondary to lesion of the vagus nerve at peri-oesophageal level. All these complications, although rare, should be included in the differential diagnosis of unexplained symptoms in patients who have undergone pulmonary vein ablation in the past.
Pulmonary vein stenosis, although it presents asymptomatically in most cases,4 can manifest, as well as with haemoptysis, as dyspnoea on exertion, cough, chest pain or repeated infections,5 which appear between 2 and 5 months after the procedure. For this reason, it is important to be aware of this complication, and to suspect it when these symptoms are present, in order for its early diagnosis and correction.
The therapeutic option in these patients is balloon angioplasty, with or without stent placement. At present, there are no definitive data that suggest that stenting obtains better results than balloon dilation alone.6 In our patient, we initially opted for isolated angioplasty, although given the serious clinical repercussions, it was finally decided to place a stent in a second procedure.
Regardless of the therapeutic procedure chosen, and despite the high re-stenosis rate, recent studies show that early intervention is recommended in symptomatic patients.6 In the case of asymptomatic patients, the treatment appears to show benefits, although the indication is not as clear.
Our patient's subsequent progress to date has been favourable, with no new episodes of haemoptysis and remission of the dyspnoea on exertion.
Please cite this article as: Demelo-Rodríguez P, et al. Hemoptisis y estenosis de venas pulmonares tras ablación por fibrilación auricular: fisiopatología y opciones terapéuticas. Arch Bronconeumol. 2013;49:366–7.