Thymolipoma is an uncommon benign neoplasm of the thymus composed of mature adipose and thymic tissue. The diagnosis of thymolipoma should be considered in the case of a mediastinal mass with fat density, especially if it is interspersed with strands of soft tissue attenuation on computed tomography scans. However, it is sometimes difficult to differentiate radiologically between a thymolipoma and other mediastinal fatty tumors.
Here we present a patient with a huge mediastinal mass that proved to be a thymolipoma.
El timolipoma es una neoplasia benigna infrecuente del timo, formada por tejido tímico y tejido adiposo maduro. El diagnóstico de timolipoma debe considerarse en presencia de una masa mediastínicacon densidad de tejido adiposo, sobre todo si está entremezclada con bandas de atenuación de tejidoblando en las imágenes de tomografía computarizada. Sin embargo, a veces resulta difícil diferenciarradiológicamente entre un timolipoma y otros tumores adiposos mediastínicos.
Presentamos aquí el caso de un paciente con una masa mediastínica enorme que resultó ser un timolipoma.
Thymolipoma is an uncommon benign tumor of the thymus consisting of thymic tissue and mature fatty tissue. Diagnosis of thymolipoma should be considered in the case of a mediastinal mass with fat density, especially if it is interspersed with strands of soft tissue attenuation on computed tomography (CT) scans. However, it is sometimes difficult to differentiate radiologically between a thymolipoma and other mediastinal fatty tumors.
We present a patient with a huge mediastinal mass that proved to be a thymolipoma.
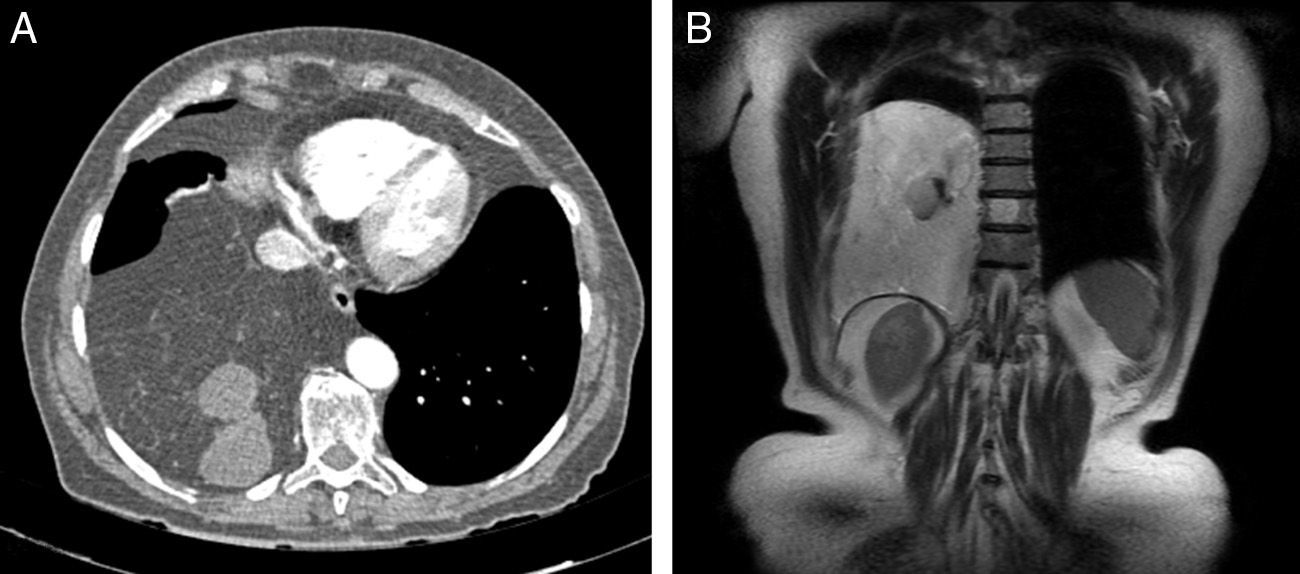
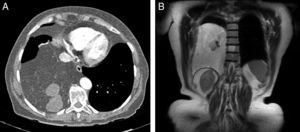
Clinical CaseA 78-year-old woman was referred to our center for evaluation of a giant mediastinal mass. Four months prior to admission, the patient began to develop a clinical picture of persistent cervical pain and postprandial nausea and vomiting. There were no changes in vital signs and physical examination. Results of clinical laboratory tests were normal, with the exception of hypercholesterolemia (285mg/dl) and hypertriglyceridemia (164mg/dl), already observed on prior testing. Other additional laboratory tests, such as IGF-I, leptin, chromogranin-A and various tumor markers (CEA, NSE, CYFRA 21.1, SSC) were not suggestive of any disease process. Blood gases breathing room air were pH 7.41, pO2 80.0mmHg, pCO2 41.0mmHg and HCO3 26.0mmol/l. Initial chest computed tomography (CT) (Fig. 1B) showed a large heterogeneous fatty mass in the right hemothorax. Magnetic resonance imaging (MRI) of the chest (Fig. 1B) confirmed the extrapulmonary intrathoracic mass identified on CT. Several cystic and solid nodules were seen within the fatty mass that was in contact with the right diaphragm, parietal pleura, right lower lobe and mediastinum (esophagus, descending aorta and pericardium). There was no infiltration of the adjacent structures. Positron emission tomography (PET) showed only slightly increased fluorodeoxyglucose (FDG) uptake in two nodular foci located within the mass (SUV 1.4g/ml and 1.5g/ml). On completion of the preoperative evaluation, a right posterolateral thoracotomy was performed via the sixth intercostal space. The mass arose in the anterior mediastinal fat, increasing in size as it extended above the superior vena cava to the right inferior pulmonary vein. After tumor dissection and sectioning of the blood vessels, the mass was resected (Fig. 2). The post-operative period was incident-free, and the patient was discharged 5 days after surgery.
Pathology examination results showed a tumor measuring 21×17×5cm, consisting of fatty tissue and thymic parenchyma. There were also foci of collagenous fibrosis and accumulation of cholesterol crystals. No signs of malignant disease were observed. These observations were suggestive of thymolipoma.
The patient remains alive and disease-free, 18 months after the intervention.
DiscussionThymolipomas are very rare, slow-growing mediastinal tumors, accounting for only 2%–9% of all thymus tumors.1 Thymolipomas are characterized by mesodermic (fatty) and endodermic (thymic epithelium) elements. They are lobulated and well encapsulated, with septal divisions. They consist of large lobules of mature adipose tissue interspersed with small areas of thymic tissue.
Thymolipomas usually present as asymptomatic tumors. When the patient does have symptoms, these are usually due to compression of adjacent structures. In our case, nausea and vomiting may have been due to esophageal compression. Occasionally, this benign tumor may be associated with certain autoimmune disorders, such as myasthenia gravis, hypogammaglobulinemia or red cell aplasia. None of these were observed in our patient.
Although the finding of soft fatty tissue within the tumor with no invasion of adjacent structures on imaging studies clearly suggests a diagnosis of thymolipoma, it is impossible to make a definitive diagnosis or to even distinguish benign disease from malignancy. Nevertheless, although radiological signs may be non-specific, CT and MRI can still offer useful data. The characteristic signs of thymolipoma on CT consist of a fatty tissue with strands of white tissue, probably corresponding to islets of normal thymic components. On T1-weighted MRI, fatty tumor tissue is isointense, and in T2-weighted sequences it is suppressed, while the thymic tissue remains are enhanced. Differential diagnosis includes other adipose tumors, such as prominent epicardial fat pad, lipomas, liposarcomas or thymoliposarcomas.
Definitive diagnosis is based on histopathological findings. We must consider whether a preoperative fine needle biopsy aspirate (FNAB) is really necessary in all patients with radiological suspicion of thymolipoma. Heimann et al.2 published the first description of a thymolipoma diagnosed using this technique in 1987. However, the role of FNAB in these cases is controversial. It is not always easy to differentiate between a thymolipoma and other fatty mediastinal lesions, such as well-differentiated liposarcoma. Romero Guadarrama et al.3 reported a false positive result on FNAB in a patient with an erroneous diagnosis of well-differentiated liposarcoma. On the other hand, Gupta et al.4 recently published the case of a child diagnosed from a cytology specimen obtained by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). We decided not to perform FNAB in our patient, as this would not have ruled out the need for surgery.
The only curative treatment of thymolipomas is surgical excision. This treatment is helpful in reducing symptoms caused by the compression of adjacent structures and autoimmune diseases. Various surgical approaches have been described, including thoracotomy, sternotomy or video-assisted thoracoscopy.5 The decision must be tailored to tumor size and site.
To conclude, thymolipoma is a very rare benign mediastinal tumor, consisting of thymic and fatty tissue. Preoperative diagnosis is frequently based on CT and MRI findings. The use of FNAB remains controversial. Surgical intervention is the only cure and also provides the definitive diagnosis.
Please cite this article as: Obeso Carillo GA, García Fontán EM, Cañizares Carretero MÁ. Timolipoma gigante: presentación de un caso de tumor mediastínico inusual. Arch Bronconeumol. 2014;50:557–559.