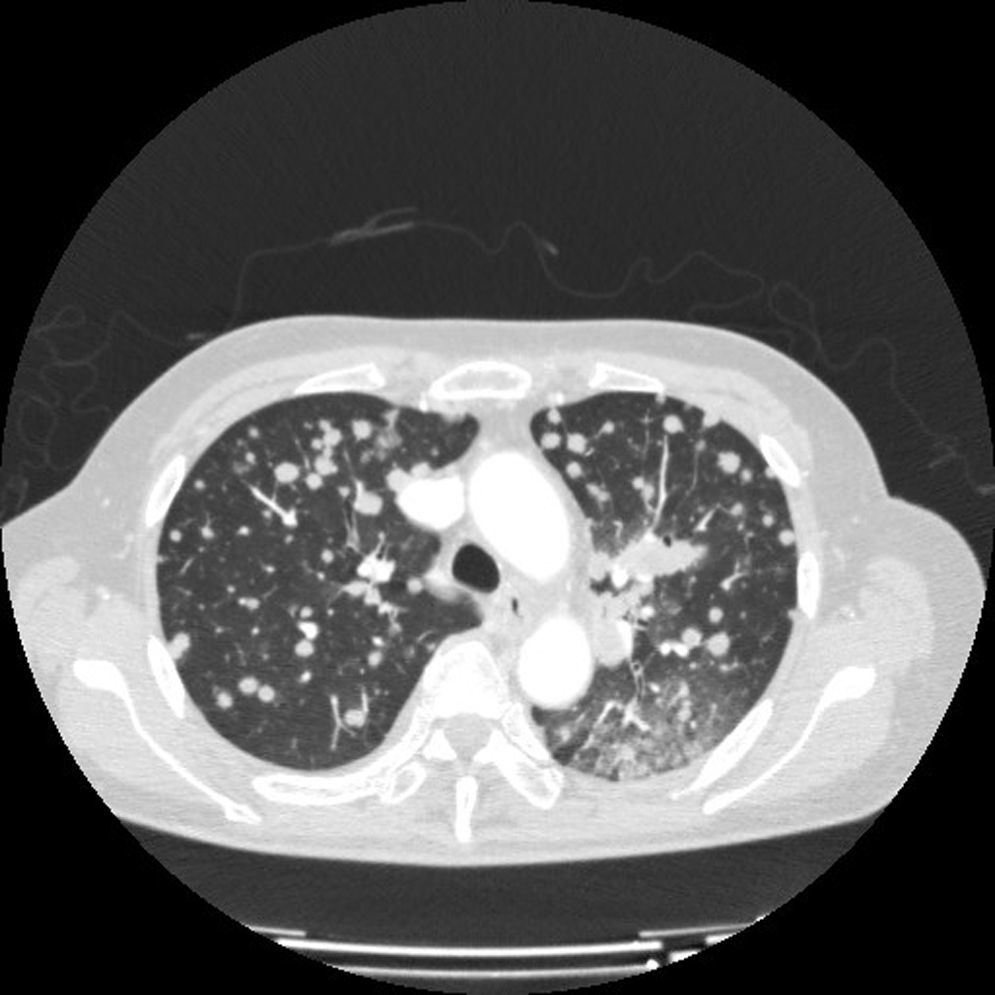
We report the clinical case of 63-year-old woman, non-smoker, of Japanese origin, who presented with dry cough of several months duration. Computed tomography (CT), positron emission tomography (PET) and fiberoptic bronchoscopy results were consistent with disseminated TTF1-positive lung adenocarcinoma (pulmonary mass in the left lower lobe with multiple bilateral nodules and bone lesions). In view of the patient's characteristics, epidermal growth factor receptor (EGFR) mutational status was requested. Exon 19 deletion was confirmed, so first line treatment with anti-EGFR was started. Tolerance was excellent, and the patient showed significant clinical improvement. The follow-up CT showed clear improvement in lesions that met RECIST criteria for partial response. Nevertheless, 2 months later, the patient developed severe left chest pain and a sensation of dyspnea. The control CT was brought forward, and revealed significant progression of the lung and bone lesions, with substantial increases in size and number of pulmonary nodules and a new rib lesion involving contiguous soft tissue (Fig. 1). In view of this rapid disease progression in a patient with EGFR-mutation lung cancer, a repeat biopsy was obtained to reevaluate the tumor genotype. The result was consistent with EGFR-mutation lung cancer, but 2 different mutations were identified: the previously determined exon 19 mutation and the T790M mutation in exon 20 that confers resistance to anti-EGFR agents. These results led us to discontinue the EGFR inhibitor and to start chemotherapy. However, the patient's general condition declined within a few days, and she died shortly afterwards.
This case illustrates 2 basic points: firstly, the need to determine the patient's EGFR mutation status, and to define the mutation subtype, since it is now established that not all mutations confer the same sensitivity to anti-EGFR agents. In our case, an exon 19 mutation was identified; this, together with the exon 21 mutation, are the most common genotypes, and both are highly sensitive to inhibitors. Progression-free survival of around 9–10 months has been reported for these subtypes in various trials.1,2 However, up to 50% of patients treated with an EGFR inhibitor can develop acquired resistance, when the T790 mutation appears in exon 20, as occurred in our case.3,4 This is of great importance, since the benefit of EGFR inhibition is lost and new strategies must be sought to block this pathway. Possible approaches include c-MET inhibitors or latest generation anti-EGFR agents. Currently, these patients are not routinely re-biopsied, but our case indicates that this is essential, since de novo mutations can have significant therapeutic and prognostic implications requiring modifications in routine clinical practice.
Please cite this article as: Cruz Castellanos P, D’errico G, de Castro Carpeño J. Hallazgo de mutación de resistencia al gen del receptor del factor de crecimiento epidérmico: a propósito de un caso. Arch Bronconeumol. 2015;51:477–478.