In recent years, there has been a progressive increase in the use of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), and it is currently the technique of choice for cytological analysis of mediastinal and hilar nodes in lung cancer and other diseases affecting this anatomical region. It is a very safe, minimally invasive technique.1,2 We report an unusual complication of EBUS-TBNA not described in the literature, involving pulmonary arterial thrombosis associated with intrapulmonary adenitis.
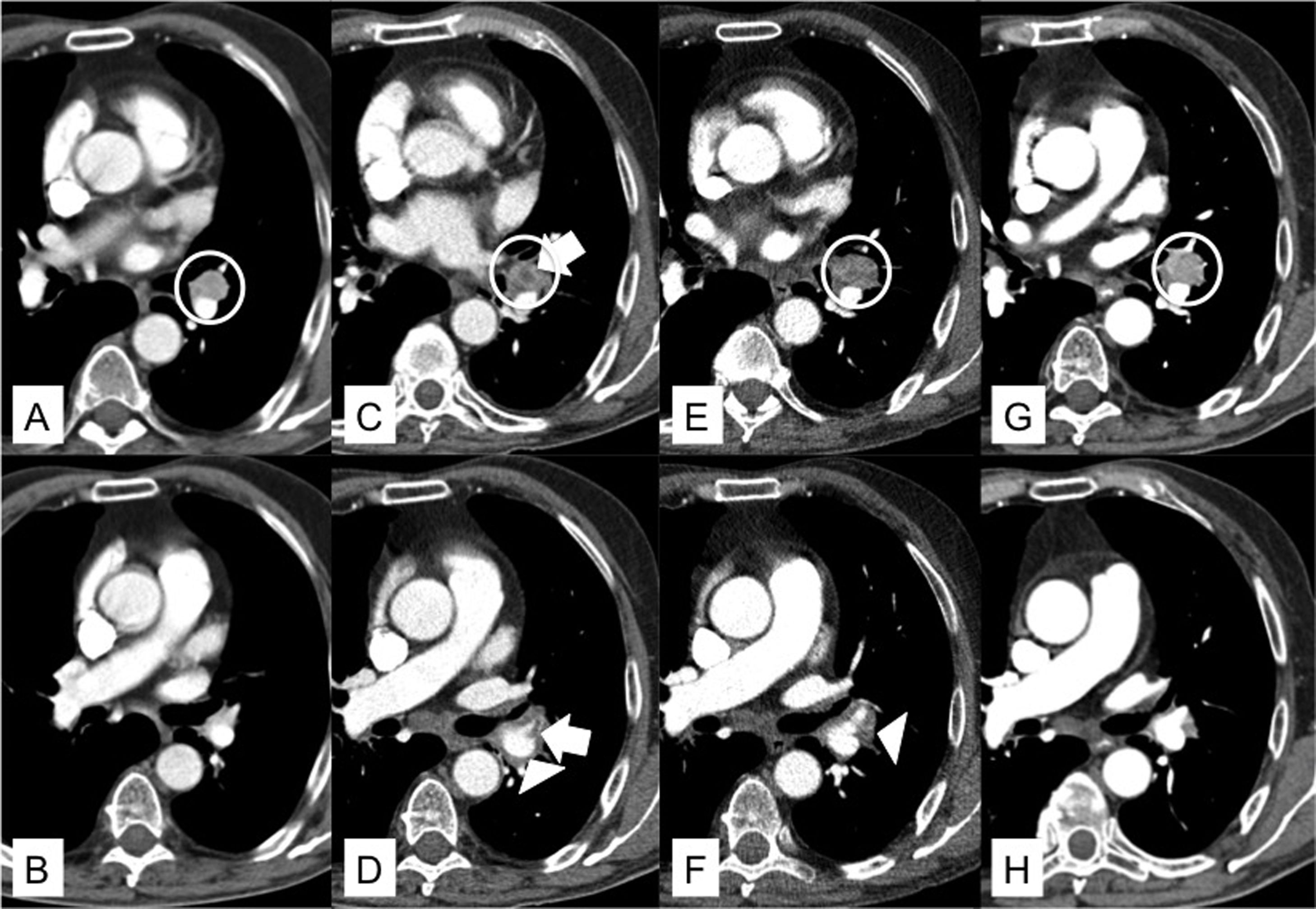
Our patient was a 71-year-old man, diagnosed 7 years previously with stage I clear cell renal carcinoma who required left radical nephrectomy and, 3 years later, atypical segmentectomy in the right upper lobe for single lung metastases. During follow-up, a chest computed tomography (CT) was performed, showing a left interlobar lymphadenopathy measuring 12 mm in its smallest diameter, with central necrosis. EBUS-TBNA identified and aspirated a left interlobar lymphadenopathy (nodal station 11) measuring 15 mm in its smallest diameter, determined on cytological analysis to be clear cell renal carcinoma metastasis. Six days after EBUS-TBNA, the patient presented in the emergency room for general malaise, 38−40 °C fever, dyspnea, and non-specific chest pain. Blood tests showed C-reactive protein 16 mg/dl, leukocytosis 14.96 × 10^9/l, with neutrophilia 13.6 × 10^9/l. Chest X-ray was normal. Empirical antibiotic treatment began with ceftriaxone and azithromycin, but the patient remained febrile, so we requested a chest computed tomography (CT) that confirmed the persistence of left interlobar lymphadenopathy surrounded by an image of soft tissue density adjacent to the enlarged lymph node, particularly in its upper margin, possibly corresponding to the needle path, that also included the left lower lobar artery. An image of acute thrombus was also observed at the point where the lingular branch of the pulmonary artery emerges (Fig. 1). A diagnosis of intrapulmonary adenitis with associated arterial thrombosis was given, and antibiotic coverage was changed to piperacillin/tazobactam and linezolid. Anticoagulant treatment started with enoxaparin 1 mg/kg every 12 h. The patient’s progress was favorable, with resolution of fever and normalization of inflammatory parameters. A chest CT scan 1 month after discharge showed resolution of the intrapulmonary adenitis and thrombosis of the lingular artery.
A: Chest CT scan in mediastinum window at the level of the bronchial bifurcation. Pathological lymphadenopathy with enhanced uptake is identified in the left hilum (white circumference). B: Chest CT scan in mediastinum window at the level of the right pulmonary artery. Patent lingular artery. C: Chest CT scan in mediastinal window at the level of the bronchial bifurcation, 34 days after A. The appearance of a hypodense focus (white arrow) in the center of the left hilar lymphadenopathy (white circumference) was observed. D: Chest CT scan in mediastinum window at level of the right pulmonary artery, 34 days after B. Appearance of a centrally located acute thrombus in the lingular artery (white arrow) and band of inflammation that encompasses the vascular structures of the left hilum (white arrowhead). E: Chest CT scan in mediastinal window at the level of the bronchial bifurcation, 44 days after A. Persistent left hilar lymphadenopathy and increased volume (white circumference) are observed. F: Chest CT scan in mediastinum window at level of the right pulmonary artery, 44 days after B. Resolution of acute thrombus located in the lingular artery but persistent band of inflammation surrounding the left hilar vessels (tip of white arrow). G: Chest CT scan in mediastinum window at the level of the bronchial bifurcation. Recovery of initial characteristics of left hilar lymphadenopathy, 69 days after A. H: Chest CT scan in mediastinum window at the level of the right pulmonary artery, 69 days after B. Resolution of band of inflammation that surrounded the left hilar vessels.
This is the first reported case of arterial thrombosis caused by EBUS-TBNA. Since its introduction in 2000, EBUS-TBNA has become an essential tool for investigating hilar and mediastinal lymphadenopathies in lung cancer, extrathoracic carcinomas, and various granulomatous conditions such as sarcoidosis or tuberculosis.3
Complications of EBUS-TBNA are rare but can be serious. In a national Japanese survey evaluating a total of 7345 procedures, the percentage of complications was 1%, the most frequent being hemorrhage (0.6%), followed by infectious complications (0.1%), such as mediastinitis, pneumonia, pericarditis, or cystic lesion infection.4
Similarly, a meta-analysis involving a total of 16,181 cases reported a frequency of serious adverse events of 0.1%, more than half of which were of infectious origin.5 It is speculated that mediastinitis is one of the most common infectious complications. It is potentially serious, with a mortality of 12%–50%,2,6 and is possibly caused by contamination of the working channel of the bronchoscope by oropharyngeal cavity secretions and consequent contamination of the needle and direct bacterial inoculation during the transbronchial mediastinal puncture.7 With regard to adenitis, 1 case of localized infection of subcarinal lymphadenopathy after EBUS-TBNA has been reported.6 No cases of arterial thrombosis associated with the procedure have been published in the literature. Several factors may have been involved in thrombus formation, including the proinflammatory status associated with focal mediastinitis and the capacity of tumor cells to induce the generation of thrombin, an enzyme involved in the pathogenesis of the hypercoagulable state accompanying cancer.8,9 In our case, it seems most likely that lymph node infection occurred with secondary infectious thromboarteritis due to contiguity, as suggested by the inflammatory reaction.
ConclusionEBUS-TBNA is a very safe test, but occasionally potentially serious complications can occur. If chest symptoms or fever develop after the procedure, these events must be ruled out with a comprehensive evaluation of the patient.
Please cite this article as: Palomeque A, Vollmer I, Fontana A, Lucena CM, Agustí C. Mediastinitis focal con trombosis arterial pulmonar asociada tras EBUS-TBNA. Arch Bronconeumol. 2020;57:74–75.