Computed tomography pulmonary angiography (CTPA) has become the gold standard imaging technique in the evaluation of patients with suspected pulmonary thromboembolism (PTE).1 PTE – acute or chronic – is confirmed on CTPA by filling defects in the pulmonary arteries. Several factors, whether technical or disease- or patient-related, can result in a suboptimal, low-quality CTPA, which can be misinterpreted by the radiologist.2
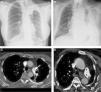
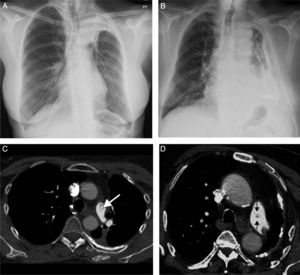
We report 2 cases of mistaken diagnosis of acute PTE in the emergency department of our hospital. Both patients complained of chest pain and dyspnea: both had elevated D-dimer levels and significant structural changes in the left hemithorax. In one of the patients, changes were due to post-radiation sequelae from lung cancer in clinical remission (Fig. 1A), and in the other they were caused by long-term pleural thickening from calcified tuberculosis (Fig. 1B). Anatomical distortion of the chest structures in general (loss of left hemithorax volume, mediastinal shift), and of the pulmonary arteries in particular (traction and kinking) caused artefacts related with turbulent flow of both blood and intravenous contrast medium in the pulmonary arteries of the left hemithorax, visualized on CTPA as apparent pulmonary artery defects (Figs. 1C and D). Filling defects were ruled out by late phase acquisitions on chest CT (obtained when the intravenous contrast medium is more diluted), thus confirming that the observations were due to artefacts. Neither patients had other pulmonary circulation filling defects or signs of right cardiac cavity overload or deep vein thrombosis.
(A) Posteroanterior chest X-ray of a 52-year-old patient (henceforth patient X) with a history of lung cancer treated with chemotherapy and radiation therapy 7 years previously, showing complete atelectasis of the left upper lobe. (B) Posteroanterior X-ray of an 85-year-old patient (henceforth patient Y), showing extensive left pleural thickening and calcification and significant loss of volume in the ipsilateral hemithorax. (C) Axial CT of patient X apparently showing a filling defect in the left main pulmonary artery (arrow), mistakenly interpreted as PTE. (D) Axial CT of patient Y apparently showing another filling defect in the left main pulmonary artery (arrows) that was also mistakenly interpreted as PTE.
Factors which may contribute to misreading a CTPA examination may be patient-related (such as artefacts caused by breathing or heart movements), technical (such as X-ray beam hardening or partial volume), or disease-related.3 Disease-related artefacts have been reported to include impacted mucus in the bronchi, perivascular edema, or pulmonary artery sarcoma. However, as far as we are aware, this is the first description of structural changes (such as presented by our 2 patient) causing anatomical distortion of the pulmonary arteries, that in turn produced intravascular turbulence of blood and intravenous contrast flow.4,5
We believe that these 2 cases underline the importance of understanding the physiopathology and intravascular hemodynamic consequences of structural changes in the chest that cause an anatomical distortion of the pulmonary arteries, in order to avoid misinterpretation during CTPA procedures.
Please cite this article as: Gorospe Sarasúa L, Ayala Carbonero AM, Fernández-Méndez MÁ. Falso tromboembolismo pulmonar en la angiografía por tomografía computarizada en dos pacientes con distorsión anatómica del tórax. Arch Bronconeumol. 2015;51:662–663.