Tuberculosis (TB) remains a highly prevalent and potentially severe disease. However, since 2002 the annual incidence has been decreasing both worldwide and in Spain, where the incidence varies widely between regions. The main objective of this study is to describe the experience of a monographic TB unit in a second level hospital.
Patients and methodsA descriptive study was carried out which included all cases of TB diagnosed in a monographic unit of a secondary hospital between 2003 and 2011. Demographic, clinical, epidemiological and microbiological data were recorded.
ResultsWe analyzed 500 TB cases and found an increasing annual incidence in all subgroups, including native and immigrant populations. Most cases (63.8%) were male, with a median age of 36 years (range 8 months–90 years). In total, 39.8% of patients were foreign born. Coinfection with human immunodeficiency virus (HIV) was found in 11.0% of cases. The pulmonary form was most frequently diagnosed (63.8%). Overall mortality was 5.8% with no significant differences between groups (including foreign born and HIV positive patients).
ConclusionsAlthough TB incidence is globally decreasing, in our study we found an increasing number of cases in recent years in all subgroups, which can be explained by this being a monographic unit with an intensive contact tracing program.
La tuberculosis (TB) continua siendo una enfermedad muy prevalente aunque desde el año 2002 el número de casos anuales muestra una tendencia decreciente en el mundo y también en nuestro país, donde la incidencia es muy variable entre comunidades autónomas. El objetivo principal de este estudio es describir la experiencia de una unidad monográfica de TB de un centro hospitalario de segundo nivel.
Pacientes y métodosEstudio descriptivo de los casos de TB diagnosticados en una unidad monográfica de un hospital secundario entre 2003 y 2011. Se recogieron datos demográficos, clínicos, epidemiológicos y microbiológicos para su análisis.
ResultadosSe analizaron 500 casos de TB encontrando una incidencia anual creciente en todos los subgrupos, incluyendo población autóctona e inmigrante. La mayoría (63,8%) eran varones, con una mediana de edad de 36 años (rango 8 meses-90 años). Un 39,8% de los pacientes era inmigrante. En 11,0% de los casos existía coninfección con el virus de la inmunodeficiencia humana (VIH). La localización fue pulmonar en el 63,8% de los casos. La letalidad global fue del 5,8% sin encontrar diferencias significativas entre subgrupos (incluyendo población inmigrante y VIH).
ConclusionesA pesar de la tendencia descendente global en cuanto al número de casos de TB declarados, en nuestra serie ésta es creciente en todos los subgrupos. La existencia de una unidad monográfica de TB junto con un exhaustivo programa de estudio de contactos podría explicar este hallazgo.
Tuberculosis (TB) remains a major health problem throughout the world. According to World Health Organization (WHO) data, although the number of annual cases has been falling since 2002, in 2010 there were 8.8 million incidental cases of TB, causing 1.4 million deaths worldwide.1
This decrease in annual cases has also been observed in Europe and Spain. According to data from the Spanish National Epidemiological Surveillance Network (RENAVE), the incidence rate for TB in Spain in 2010 was 15.5 cases per 100000 population, 8.4% lower than 2009 and 8% lower than 2008.2 This decrease occurred at the expense of pulmonary TB in particular, with the incidence rates of tuberculous meningitis and other TBs remaining stable. The TB rates declared to RENAVE are highly variable in each region, ranging between 8 and 29 cases per 100000 population, with the regions of Galicia, Melilla, and Cantabria having the highest overall rates. However, the information collected by RENAVE is incomplete with respect to certain important data, such as the presence of coinfection with human immunodeficiency virus (HIV) or treatment completion, and there is no information on other comorbidities in patients, different diagnostic microbiology tests or drug-resistance. Series published in recent years in Spain provide insight into important data with respect to treatment adherence and death rate.3,4 The percentage of those born outside Spain remains stable, around 30% of cases, and there appear to be differences between the native and immigrant populations with respect to age, adherence and anti-tuberculosis drug resistance.5–7 In the Balearic Islands, the TB incidence rate declared in 2010 was 13.3 cases per 100000 population, following the same downward trend described in the rest of the country.
The aim of this study was to describe the experience of a multidisciplinary single-specialty TB unit in Hospital Son Llàtzer (HSLL) (Palma de Mallorca, Spain), with emphasis on the time trend and 2 special populations – HIV-infected patients and immigrant patients.
Materials and MethodsDesignDescriptive study conducted in HSLL, a 350-bed hospital serving some 250000 residents of an urban-rural area of Mallorca, of whom around 43000 (17.2%) are immigrants. The study was approved by the center's research committee.
PatientsAll TB cases diagnosed in the HSLL during the period January 2003–December 2011 were included.
MethodsIn 2003, the HSLL opened a multidisciplinary (Internal Medicine, Respiratory Medicine, Pediatrics and Nursing) single-specialty TB clinic. In this one-stop clinic, suspected cases of tuberculous disease referred from health centers or the Emergency Department are studied on an outpatient basis, patients diagnosed with TB are followed-up after discharge, and household contacts are studied. At the first visit, laboratory tests, chest radiograph, sputum culture, a tuberculin test (TT)8 and Quantiferon-TB-Gold In-Tube9 (QFT-G-IT) assay are also carried out (the latter performed on most patients as of 2008), in addition to anamnesis and a physical examination. Bronchoscopy is performed when indicated. At the second visit, 48–72h after the first, the TT is read and other additional tests are interpreted, initiating treatment when indicated, both for tuberculous disease and infection.
Diagnosis of TuberculosisAs per the clinical definition, a patient was considered to have TB when she/he had signs or symptoms consistent with tuberculous disease in the absence of any other disease that could explain them, and they responded to pharmacological TB treatment. The case was confirmed bacteriologically when it met laboratory diagnostic criteria, i.e., isolation in culture of a Mycobacterium tuberculosis complex microorganism, or, if unable to perform said culture, with the demonstration of acid-fast bacilli by microscopy in a suitable clinical sample. A case was considered to be not bacteriologically confirmed when it met the criteria for clinical case definition but did not meet laboratory diagnostic criteria.10
Clinical and Epidemiological DataPatient medical records were reviewed retrospectively, and the following information was collected: sociodemographic data (age, sex, and country of origin), substance abuse (smoking, drinking considered as consumption of more than 30g of alcohol per day and intravenous drug use), comorbidities (diabetes, neoplasms, and HIV infection), diagnostic method and sample, treatment prescribed, anti-tuberculosis drug susceptibility, toxicities, treatment adherence and final outcome.
StatisticsThe descriptive statistical analysis included median and range for continuous variables, and frequencies and proportions for categorical variables. The quantitative variables were compared using the Student's t-test; the Chi-square test was used for the qualitative variables when they met the applicable criteria. The difference was considered statistically significant when P<.05. The odds ratio and 95% confidence interval were used to estimate the risk. The time course was studied by calculating the linear trend using the least squares method. Computer applications SPSS Statistics 18® and Epidat 3.1® were used for the statistical analyses.
ResultsGeneral CharacteristicsIn the time period reported, a total of 500 cases of TB were diagnosed. The patient characteristics with respect to substance abuse and comorbidities are described in Table 1. In total, 29 cases (5.8%) were diagnosed in children under 14 years old and 18 (3.6%) in children under 5. Fifty-five patients (11.0%) were HIV-positive. Of the 500 cases of TB, 199 (39.8%) occurred in immigrants. The location of the TB is described in Table 1. Most cases (380 cases; 76.0%) were located in the lungs or pleura only. Meningeal TB was diagnosed in 21 cases (4.2%). The remaining 99 cases (19.8%) were TB in other locations (including the lymph nodes, skin and genitourinary tract among others). In total, 43 cases (8.6%) were recurrent, with evidence that 21 patients had previously completed treatment (48.8%), while the remaining 32 patients had not completed or started treatment for various reasons.
Clinical and Epidemiological Characteristics of Patients Diagnosed With Tuberculosis in Hospital Son Llàtzer.
| Median age | 36 years (range 8 months-90 years) |
| Males | 319 (63.8%) |
| Substance abuse | |
| Smoking | 210 (42.0%) |
| Alcoholism | 84 (16.8%) |
| IVDU | 19 (3.8%) |
| Underlying diseases | |
| Neoplasia | 12 (2.4%) |
| Diabetes mellitus | 16 (3.2%) |
| HIV infection | 55 (11.0%) |
| Immunosuppressant treatment | 17 (3.4%) |
| Location of the tuberculosis | |
| Lungs | 331 (66.2%) |
| Lymph nodes | 36 (7.2%) |
| Pleural | 49 (9.8%) |
| Meningeal | 21 (4.2%) |
| Disseminated | 26 (5.2%) |
| Other | 37 (7.4%) |
IVDU, intravenous drug users. Alcoholism: >30g of alcohol/day. Immunosuppressant treatment: corticosteroids and other immunosuppressants (methotrexate, azathioprine).
The smear was positive in 259 of 486 cases in which it was performed (53.3%) and the culture in 358 of 473 cases (75.7%). The smear was positive with a positive culture in 5 cases and a negative culture in 22 cases, of which 6 (27.3%) were on treatment with quinolones at the time the sample was taken.
OthersOther diagnostic methods used, and which were occasionally positive at the same time as the microbiological tests, were: pathology in 60 cases (12.0%), adenosine deaminase (ADA) in cerebrospinal or pleural fluid (with consistent biochemistry) in 72 cases (14.4%) and polymerase chain reaction (PCR) in 4 cases (0.8%).
Tuberculin Test and Quantiferon-TB-Gold In-Tube AssayThe QFT-G-IT was performed prior to starting TB treatment in 167 of the cases studied: it was positive in 130 (77.8%), negative in 31 (18.6%) and indeterminate in 6 cases (3.6%). The TT was positive in 365 (87.1%) of the 419 cases in which it was performed.
Anti-Tuberculosis Drug ResistanceSusceptibility testing was available in 357 cases. Isoniazid resistance was detected in 17 cases (4.8%) and isoniazid and rifampicin resistance (multi-resistance) in 4 cases (1.1%) (streptomycin resistance was also observed in one of these cases). Among the first 17 cases, none of the patients had previously had anti-tuberculosis treatment, while among the 4 cases of multi-resistance, 2 had undergone and completed treatment. There were no cases of extensively drug-resistant TB.
Treatment and OutcomeInitial treatment was commenced with 4 drugs (rifampicin, isoniazid, pyrazinamide and ethambutol; RHZE) in 296 cases (59.2%), while treatment with 3 drugs (RHZ) was indicated in the remaining cases. During the first study period (January 2003–January 2007), the percentage of patients treated initially with the RHZE regimen was 52/169 (30.8%), while in the second period (January 2007–December 2011), it was 253/331 (76.4%), showing a statistically significant difference (P<.001). Treatment had to be modified due to toxicity (mainly liver and skin) in 36 cases (7.2%). With respect to outcome, recovery was observed in 407 patients (81.4%). Thirty patients dropped out of treatment (6.0%). Thirteen patients died in total (5.8%); in all cases the cause of death was directly related with TB. In the patient group with TB-related deaths, the mean age was 67 years (range 31–87), significantly higher than the other TB patients (P<.001). The meninges were most common location in this sub-group, presenting in 2 patients (15.4%). Most were native (76.9%; 10 patients) and males (76.9%; 10 patients), with no statistically significant differences compared to the rest of the population. There were no differences with respect to death rates when other variables such as HIV, substance abuse, previous TB or other comorbidities such as diabetes mellitus were considered.
Patients With Human Immunodeficiency Virus InfectionHIV serology was performed in 486 patients (97.2%). In our series, 55 patients (11.0%) were HIV-positive (Table 2). Most (65.5%, 36 patients) were Spanish, and the immigrants were mainly from Sub-Saharan Africa (13 cases; 23.6%), especially Nigeria. Only 13 (23.6%) of the patients with HIV infection received anti-retroviral treatment (ART) regularly, with good adherence, of whom 3 (23.1%) had an undetectable viral load at the time of TB diagnosis. Fifteen patients (27.3%) had been prescribed ART but did not take it regularly. None of the remaining 27 patients received ART: 12 (21.8%) were diagnosed with HIV and TB simultaneously and 15 (27.3%) were aware of their HIV diagnosis but for various reasons had not commenced ART. The median CD4 was 122cells/μl (range 6–663). Among TB patients coinfected with HIV, there were significantly more smokers, and intravenous drug addiction was more common in this group. The disseminated forms, including tuberculous meningitis, were more common in patients with HIV infection. The TT was negative more often in HIV patients, unlike the QFT-G-IT test.
Differences Between Patients With and Without HIV Diagnosed With Tuberculosis at Hospital Son Llàtzer.
| HIV (n=55) | Non-HIV (n=431) | P | OR (95% CI) | |
| Mean age | 40.16 (SD 9.3) | 40.33 (SD 19.3) | NS | |
| Sex, M/F | 40/15 (72.7%/27.3%) | 277/154 (64.3%/35.7%) | NS | |
| Smoker | 49 (89.1%) | 174 (40.1%) | <.001 | 12.06 (5.05–28.77) |
| Alcoholism | 12 (21.8%) | 71 (16.5%) | NS | |
| IVDU | 19 (34.5%) | 10 (2.3%) | <.001 | 22.22 (9.61–51.36) |
| Cancer | 2 (3.6%) | 9 (2.1%) | NS | |
| Diabetes | 0 (0.0%) | 16 (3.7%) | NS | |
| Immunosuppressants | 0 (0.0%) | 13 (3.0%) | NS | |
| Pulmonary TB | 27 (49.1%) | 295 (68.4%) | .004 | 0.44 (0.25–0.78) |
| Lymph node TB | 6 (10.9%) | 29 (6.7%) | NS | |
| Pleural TB | 2 (3.6%) | 46 (10.7%) | NS | |
| Disseminated TB | 11 (20.0%) | 14 (3.2%) | <.001 | 7.44 (3.18–17.39) |
| Meningeal TB | 7 (12.7%) | 14 (3.2%) | <.001 | 5.09 (1.91–13.55) |
| Other locations | 2 (3.6%) | 35 (8.1%) | NS | |
| Positive acid-fast smear | 23 of 55 (41.8%) | 231 of 417 (53.4%) | NS | |
| Positive culture | 43 of 53 (81.3%) | 306 of 407 (75.2%) | NS | |
| INH resistance | 2 of 43 (4.6%) | 15 of 307 (4.9%) | NS | |
| Multi-resistance | 0 of 43 (0.0%) | 5 of 307 (1.6%) | NS | |
| Positive TT | 26 of 47 (53.3%) | 330 of 363 (90.9%) | <.001 | 0.12 (0.06–0.24) |
| Positive QFT-G-IT | 15 of 21 (71.4%) | 115 of 147 (78.2%) | NS | |
| 4D initial treatment | 30 (60.0%) | 261 (60.5%) | NS | |
| Lost to follow-up | 4 (7.3%) | 26 (6.0%) | NS | |
| TB-related mortality | 2 (3.6%) | 10 (2.3%) | NS |
4D, 4 drugs (RHZE); SD, standard deviation; M, male; 95% CI, 95% confidence interval; INH, isoniazid; F, female; NS, no significant differences; OR, odds ratio; TT, tuberculin test; QFT-G-IT, Quantiferon-TB-Gold In-Tube; TB, tuberculosis; IVDU, intravenous drug users; HIV, human immunodeficiency virus.
Immunosuppressant treatment: Corticosteroids and other immunosuppressants (methotrexate, azathioprine).
Statistically significant results are highlighted in bold.
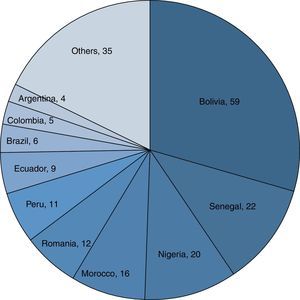
The main countries of origin of the immigrant population were Bolivia (59; 29.6%), Senegal (22; 11.1%) and Nigeria (20; 10.1%) (Fig. 1). Table 3 describes the main differences between the immigrant and native populations. In summary, it was observed that the immigrant population was significantly younger, with a higher predominance of males and less substance abuse. No differences were observed with respect to drug resistance, treatment adherence or TB-related deaths. Treatment was initiated with 4 drugs (RHZE) more often in the immigrant population.
Differences Between the Immigrant and Native Populations in Patients Diagnosed With Tuberculosis in Hospital Son Llàtzer.
| Native (n=301) | Immigrant (n=199) | P | OR (95% CI) | |
| Mean age | 45.11 (SD 20.88) | 32.78 (SD 11.81) | <.001 | 12.33 (9.13–15.53) |
| Sex, M/F | 206/95 (68.4%/31.6%) | 113/86 (56.8%/43.2%) | .01 | 1.65 (1.14–2.39) |
| Smoker | 154 (51.2%) | 56 (28.1%) | <.001 | 2.67 (1.82–3.92) |
| Alcoholism | 61 (20.3%) | 23 (11.6%) | .01 | 1.94 (1.16–3.26) |
| IVDU | 14 (4.7%) | 5 (2.5%) | NS | |
| HIV | 36 (12.0%) | 19 (9.5%) | NS | |
| Cancer | 8 (2.7%) | 4 (2.0%) | NS | |
| Diabetes | 12 (4.3%) | 4 (2.0%) | NS | |
| Immunosuppressants | 16 (5.4%) | 1 (0.5%) | .008 | 11.11 (1.46–84.50) |
| Pulmonary TB | 208 (71.1%) | 126 (63.3%) | NS | |
| Lymph node TB | 18 (6.0%) | 18 (9.0%) | NS | |
| Pleural TB | 23 (7.6%) | 26 (13.1%) | NS | |
| Disseminated TB | 16 (5.3%) | 10 (5.0%) | NS | |
| Meningeal TB | 13 (5.9%) | 8 (4.0%) | NS | |
| Other locations | 22 (7.3%) | 14 (7.0%) | NS | |
| Positive acid-fast smear | 149 of 292 (51.0%) | 110 of V194 (56.7%) | NS | |
| Positive culture | 214 of 285 (75.1%) | 144 of 188 (76.6%) | NS | |
| INH resistance | 9 of 217 (4.1%) | 8 of 142 (5.6%) | NS | |
| Multi-resistance | 1 of 217 (0.5%) | 3 of 142 (2.1%) | NS | |
| Positive TT | 207 of 242 (85.5%) | 158 of 178 (88.8%) | NS | |
| 4D initial treatment | 136 (45.2%) | 160 (80.3%) | <.001 | 0.20 (0.13–0.30) |
| Lost to follow-up | 15 (5.0%) | 15 (7.5%) | NS | |
| TB-related mortality | 10 (3.3%) | 3 (1.5%) | NS | |
| Mean annual incidence rate | 145/100000inhab.-year. | 460/100000inhab.-year. | <.001 | 0.40 (0.24–0.67) |
4D, 4 drugs; SD, standard deviation; M, male; Inhab, Inhabitants; 95% CI, 95% confidence interval; INH, isoniazid; F, female; NS, no significant differences; OR, odds ratio; TT, tuberculin test; TB, tuberculosis; IVDU, intravenous drug users; HIV, human immunodeficiency virus.
Statistically significant results are highlighted in bold.
The mean annual incidence rate for TB in the HSLL in natives was 145 per 100000 population and year, and in immigrants was 460 per 100000 population and year.
Study of ContactsA study of those living with the index cases has been carried out since January 2006. This study has enabled tuberculous disease to be diagnosed in 23 (3.1%) of the 741 contacts studied.
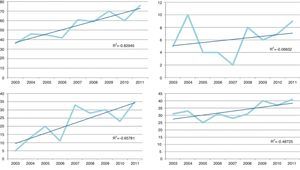
Time TrendFig. 2 shows the time trends for the number of cases of TB in the general population and in 3 sub-groups: HIV-infected patients, the native population and the immigrant population. All sub-groups showed an upward trend, mainly in the non-native population sub-group.
DiscussionTuberculous disease is increasingly prevalent in our healthcare area, and is occurring in both the native and, to a larger extent, the immigrant population. Anti-tuberculosis drug resistance was very rare, and we only had 4 cases of multi-resistance during the period studied. The rates of drop-out and TB-related deaths were low.
Our data contrast with those of RENAVE and series published in Spain,2,11 which indicate that the incidence of TB has been falling in recent years. This rise in the number of cases in our area could have various explanations. The existence of a single-specialty, multidisciplinary TB clinic in our hospital and the teaching activities carried out around it may have raised awareness in clinicians to actively search for TB; furthermore, a study of contacts of patients diagnosed with TB in our hospital has been carried out since 2006, which has allowed a further 23 cases of tuberculosis to be diagnosed, i.e., 3.1% of the 741 contacts of the cases studied. This proportion of patients among the contacts of an index case is more than twice that observed in a study conducted in Vizcaya (Spain),12 and shows the importance of performing a systematic study of contacts of each TB case. Furthermore, the HSLL healthcare area covers economically deprived areas of the city with a high immigrant population, where there is probably a higher incidence of TB cases.
The proportion of HIV-coinfected TB patients was 11% and remained stable in the study period, although it was somewhat higher than that observed in other series and in data collected in the RENAVE or the European TB surveillance network,2,13 where HIV infection is described in 6% of cases. Other Spanish studies have shown a gradual decrease in the number of HIV-infected TB patients in recent years,5,10 which we did not observe in this small series. Substance abuse, especially smoking and intravenous drug addiction were more common in this group. Lung involvement was significantly less common than in patients not infected with HIV, unlike the disseminated forms, including meningitis, which were more common in this group, in agreement with the data declared in the country as a whole in this population.2 The high percentage of patients diagnosed simultaneously with HIV and TB in our study was notable.
The increase in the number of annual cases of TB occurs especially (although not exclusively) in relation to the immigrant population, as has already been observed in other studies.14 The overall percentage of immigrants in our series was 39.8%, higher than the 33% declared to RENAVE in Spain in 2010,2 and also higher than the 29.7% observed in the Spanish multicentre ECUTTE study.3 The countries of origin of most immigrant patients with TB in our area were Bolivia, Senegal and Nigeria, although immigration from these countries, according to 2011 data from the Palma municipal observatory,15 only constitutes a small proportion of the total immigration in Palma de Mallorca (5.4%, 2%, and 3.1%, respectively). As in other studies, the immigrant population tended to be younger, with less substance abuse and fewer comorbidities than the non-immigrant population.3,6 However, unlike the ECUTTE multicentre study,3 and the study conducted in Granada (Spain) by Molina-Rueda et al.,5 we did not observe poorer treatment adherence in the group of foreign patients, a higher death rate or a higher number of resistances to first-line anti-tuberculosis drugs as found in other Spanish publications.5,6
Most patients received 4 first-line drugs (RHZE) as the initial treatment for TB; the percentage of patients receiving this therapeutic regimen was higher in the immigrant population and in the case of TB recurrence, following national recommendations.16 However, in our area, we observed a low overall rate of resistance to isoniazid or to isoniazid/rifampicin (21 of 357 cases [5.9%], of which 4 were cases of recurrence). If we exclude the cases of recurrence, the percentage of primary resistance in our area is lower (4.2%) and we could even reconsider the need for initial treatment with 4 drugs in our area in some cases, as other authors have suggested.17
The death rate was low in our series, compared with others such as that published in 2006 by Pina et al.,18 where a death rate of 6.4% was observed, without specifying the underlying causes. Among European countries that also report death rates, the overall death rates published are higher (10.2%).12 In our series, the only variable associated with a higher risk of mortality was age, as has been published in other studies18,19; the death rates in patients with HIV were also significantly lower than those found in a large series in Catalonia (Spain) which showed, in the era of highly active ART, a death rate of 43.1% in HIV patients coinfected with TB.20 However, alcoholism, multi-resistance or the coexistence of a neoplasm were not associated with an increase in TB-related deaths. The low prevalence of patients with diseases such as diabetes or neoplasms, as well as multi-resistance, may explain this finding.
Unfortunately our study has certain limitations, primarily that this is a descriptive study with a retrospective nature. Furthermore, some of the sub-groups studied, such as HIV-infected patients, have a small number of cases. Another limitation, when estimating the possible role of the single-specialty unit, is that we do not have a period before its introduction to compare results. However, given that the migratory flow to Mallorca is relatively low, according to data from the Spanish National Statistics Institute,21 it seems unlikely to have influenced our results.
ConclusionsIn our study, we observed an upward trend in the number of cases during the study period, as well as a higher percentage of immigrants than in other series and registers in Spain. Treatment adherence was similar in the immigrant and native populations, with low overall mortality. The index case contact study allowed us to diagnose a not inconsiderable number of cases. All of this reaffirms the importance of a single-specialty unit dedicated to the diagnosis and treatment of TB, and the study of contacts to optimize control of the tuberculosis endemic. We therefore consider that the financial difficulties experienced by the Spanish National Health System should not affect TB diagnosis and treatment programs, which are essential for achieving real control of the epidemic.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: González-Moreno J, et al. Experiencia de una unidad monográfica de tuberculosis: primeros 500 casos. Arch Bronconeumol. 2013;49:421–6.