An 83-year-old non-smoking woman with a medical history of essential hypertension, type 2 diabetes mellitus, and IgA Lambda monoclonal gammopathy presented with chronic cough, fatigue, and progressive weight loss over 2 years. A chest CT scan revealed a patchy bilateral infiltrate, diffuse bronchiectasis, and cavitated lesion over right lower lobe (RLL). Subsequent diagnostic bronchoscopy was performed, with positive result for Mycobacterium tuberculosis (positive bacilloscopy, PCR and culture, with necrotic biopsy).
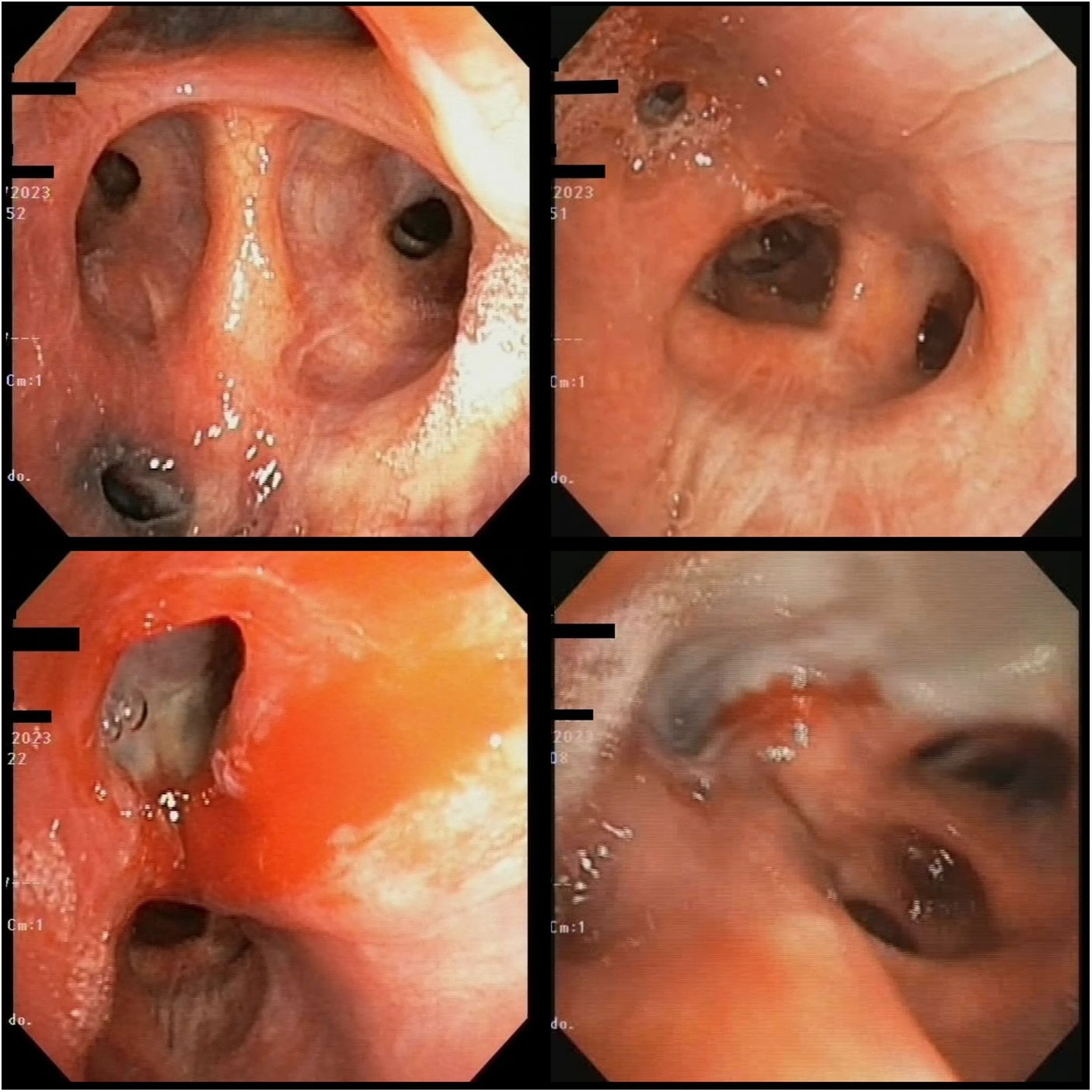
During the respiratory endoscopic study (Video 1, Figure 1) different evolutionary types were observed (type F, C, A) of endobronchial tuberculosis (EBTB) in the same patient.1,2
EBTB is classified according to Chung and Lee2: A, active caseation; B, edematous-hyperemic; C, fibrostenotic; D, tumour; E, granular; F, ulcerative; and G, nonspecific bronchitis. The pathogenesis may include direct implantation, infiltration, erosion and protrusion of tuberculous lymph node into the bronchus and hematogenous spread or lymphatic.1,2 It has a variable incidence, underdiagnosed because routine bronchoscopy is not performed. Different types may appear in the same patient,1 with a worse prognosis, types A, B, C, D, because they are associated with residual tracheobronchial stenosis.2 Therefore, not only anti-tuberculosis treatment is very important for prevent stenosis, but also diagnosis and endoscopic follow-up.
Informed ConsentWritten informed consent was obtained from the guardian for the publication of the article.
FundingThere was no funding source in this study.
Conflict of InterestThe authors declare that they have no conflict of interest.
The authors thank Félix Del Campo Matía and Tomás Ruiz Albi for their advice during the preparation of this paper.
The following are the supplementary data to this article:
We observed anthracotic mucosa. Ulcerative-cavitated lesion (type F) with anthracotic mucosa underlying the anterior segment of the right upper lobe. Middle lobe fibrostenosis (type C). Active caseating lesion (type A) at the level of the medial segment of the RLL and ulcerative-cavitated lesion or fistula (type F) with hyperemic mucosa at the level of the intermediary bronchus.