Tracheobronchopathia osteochondroplastica (TO) is caused by osteocartilaginous nodules originating from the cartilaginous rings and is therefore located in the anterior part of the trachea. The aetiology of TO is still not fully understood. The disease is benign and has an indolent course. Most patients are asymptomatic or have nonspecific respiratory symptoms.1
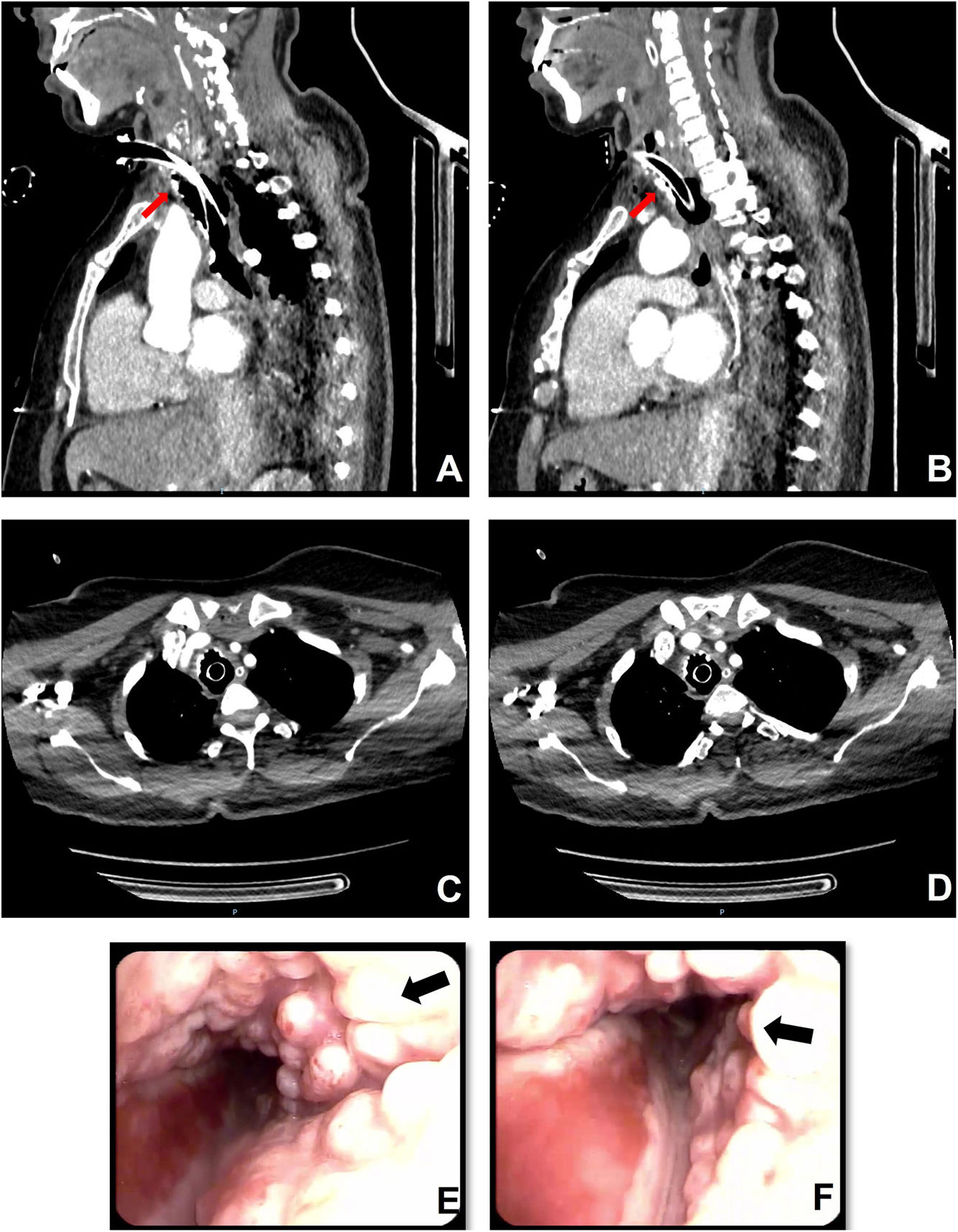
Chest X-ray is often unremarkable. Thorax computed tomography (CT) scan may show calcified nodules arranged along the antero-lateral wall of the trachea and the main bronchi. Firm and glossy nodules with intact mucosa, are typical bronchoscopic findings of TO.2
We describe a patient who underwent emergency tracheostotomy due to failed oro-tracheal intubation procedure for the anatomical conformation, during prolonged generalized non motor seizures with severe respiratory failure. CT scan shows multiple calcified nodules on the antero-lateral tracheal wall that spared the laryngeal tract (Fig. 1A–D), confirmed by bronchoscopy (Fig. 1E and F). Histological examination of a biopsy fragment sustained the diagnosis of TO.
In the antero-lateral tracheal wall, thorax CT scan shows calcified nodules, which protrude into the airway (A–D, red arrows). Large nodules, above the tracheal cannula cuff, are in contact with the cannula itself and occluding the tracheal lumen (B). Bronchoscopy reveals firm and glossy nodules with intact mucosa layer (E and F, black arrows), the posterior tracheal wall is spared.
During evaluation for removal of the tracheal cannula, with the cannula scuffed and capped and the patient in spontaneous breathing, tracheal nodular lesions resulted in air passage obstruction in the inspiratory phase only. Therefore, cannula was removed during bronchoscopic examination that confirmed the tracheal patency.
Conflict of InterestsThe authors state that they have no conflict of interests.