Endobronchial metastases (EBM) secondary to extrapulmonary primary tumors are rare. The most common solid malignant tumors associated with EBM are breast, renal and colorectal carcinomas.
This case report describes the first documented case of EBM from anal canal carcinoma. This neoplasm constitutes less than 1% of colorectal tumors.
The clinical presentation of this entity is variable, being asymptomatic in more than 50% of cases. Generally, EBM are diagnosed in advanced stages and the survival after the diagnosis is poor.
It is therefore an exceptional clinical manifestation in which bronchoscopy has an important role in the diagnosis and the treatment.
Las metástasis endobronquiales (MEB) de tumores primarios extratorácicos son infrecuentes. Los tumores de órganos sólidos que con más frecuencia se han asociado a MEB son el carcinoma de mama, el renal y el colorrectal.
En esta nota clínica se describe el primer caso documentado de MEB de carcinoma del canal anal, neoplasia que constituye menos del 1% del total de tumores colorrectales.
La presentación clínica de esta entidad es variable y es asintomática en más del 50% de los casos. Generalmente las MEB suelen diagnosticarse en fases avanzadas, por lo que la supervivencia es baja. Se trata pues de una manifestación clínica excepcional en que la broncoscopia tiene un importante papel tanto en el diagnóstico como en el tratamiento.
Endobronchial metastases (EBM) of extrathoracic primary tumors are rare. It is estimated that the incidence of EBM in patients who die due to metastatic disease is 2%. The solid organ tumors that have most frequently been associated with EBM are breast, renal and colorectal cancer. We report the first case of EBM of an anal canal squamous-cell carcinoma, a variety that represents 1% of colorectal tumors.
Clinical NotesThe patient is a 46-year-old woman with no known allergies to medication, who was an ex-smoker with an accumulated use of 40 pack-years and former parenteral drug addict. The patient's pathological history included HCV and stage 3 HIV infection since 1990, with the presentation of multiple opportunistic infections. In 2001, she underwent cervical conization due to cervical intraepithelial neoplasia (CIN III) secondary to human papillomavirus (HPV) infection, serotypes 16 and 18.
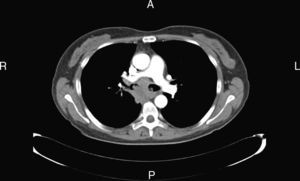
In October 2008, the patient was diagnosed with squamous-cell carcinoma of the anal canal (T4N1M0), and therefore underwent treatment with radiotherapy and chemotherapy (cisplatin and 5-fluorouracil). One year later, thoracic computed tomography (CT) revealed two nodules measuring less than a centimeter in the upper and lower right lobes, which were considered probable lung metastasis of the primary neoplasm, and 7 more cycles were administered. Three months after finishing the treatment, chest CT demonstrated an increase in the size of the lung nodules and the appearance of lymphadenopathy in the right paratracheal, subcarinal and right hilar regions (Fig. 1). Bronchoscopy revealed thickening of the main carina and three large polylobulated and hypervascular lesions, in the main carina and in the main right and left bronchi, causing the obstruction of 80% of the bronchial lumen. Given these findings, the endobronchial lesions were removed by laser photoresection. The results of the anatomopathologic study were compatible with metastasis of squamous-cell carcinoma of the digestive tract, with areas of necrosis.
Initially, the patient showed a positive clinical evolution, but died 2 months later due to hospital-acquired pneumonia.
DiscussionColorectal cancer represents 15% of all neoplasms and it is the second most frequent neoplasm in both sexes. Anal canal neoplasm represents less than 1% of all colorectal tumors. Classically, it has been associated with chronic anorectal pathologies (hemorrhoids, fistulas) or with sexually transmitted diseases, particularly with HPV (serotype 16) infections, such as in the case reported.
The diagnosis of anal canal carcinoma is usually made in advanced phases of the disease. The most frequent histologic type is squamous-cell, which frequently causes local growth in neighboring structures with lymph node affectation of the mesorectal or inguinal nodes and even, in some cases, hematogenous dissemination. Unlike colon cancer and carcinoma of the upper half of the rectum, which mainly metastasize in the liver, in the case of anal canal tumors lung metastases are more common. The presence of EBM of an anal canal carcinoma has not been previously reported in the literature.
Different extrathoracic tumors can cause EBM, but those that do so more frequently are breast cancer, hypernephroma and colorectal cancer, the latter being responsible for 12%–26% of EBM.1
The clinical and radiological presentation of EBM is undistinguishable from that of a primary endobronchial tumor. The most frequent symptoms are cough, dyspnea or hemoptysis, but up to 52%–62% of patients can be asymptomatic at the time of diagnosis,2 as in the present clinical case report. This fact justifies the frequent delay in the diagnosis, which according to different series oscillates between 44 and 63 months.3–6 In the present clinical case, the diagnostic delay was less evident, probably due to the fast growth of the lesions secondary to the severe immune deficiency of the patient.
Chest radiography can demonstrate indirect signs of endobronchial affectation, such as mediastinal thickening or atelectasis. Despite the fact that in our case the EBM were visible on thoracic CT, it generally is not an ideal diagnostic test due to its low sensitivity, which does not surpass 55%. Bronchoscopy is considered the best exploration for diagnosing EBM,7 and it usually shows evidence of hypervascular polypoid lesions (as shown in Fig. 2) and samples for the definitive diagnosis can be obtained. This is especially important because the management and prognosis of EBM can be very different from those of a primary bronchogenic carcinoma.8 Furthermore, endoscopic treatment with laser or cryotherapy can be very useful in preventing complete bronchial obstruction and improving the quality of life of these patients.5
According to their development, EBM have been classified as primary lesions (type I: direct metastasis in the bronchus) and secondary lesions (type II: bronchial invasion from a parenchymatous lesion; type III: hilar and mediastinal lymphadenopathies, or type IV: peripheral lesions that extend through proximal bronchi). In some series, secondary lesions represent up to 69% of cases.3 In the clinical case presented, the EBM would be type III.
Survival after EBM diagnosis is generally poor as it is considered a manifestation that appears in advanced stages of the disease.9 According to published studies, the survival of patients after the diagnosis of EBM ranges between 12 and 15 months.3,10 Ettensohn et al.11 report longer survival times in patients with EBM from breast neoplasms. In the study by Kiryu et al.,3 in which survival was assessed according to the type of EBM, survival ranged between 2 months for type III and 31 months for type II.
The fast, unfavorable evolution in this present case could be justified by the immune disorder secondary to the baseline disease. Our case is the presentation of an exceptional clinical manifestation of EBM of an anal canal tumor with torpid evolution, probably in the context of severe comorbidity.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Dalmases M, et al. Metástasis endobronquiales de carcinoma del canal anal. Arch Bronconeumol. 2012;48:258–60.