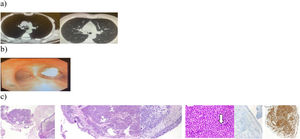
A 46-years-old male patient admitted to the clinic with the complaint of cough with as ashen-colored sputum that had been going on for six months. He was active smoker and working in a shoe manufacturing factory. He had no other medical history. A hypodense nodular soft tissue appearance with a diameter of 18mm was observed in the right main bronchus on thorax computed tomography (Fig. 1a). On bronchoscopic evaluation, an endobronchial lesion with a wide base was identified narrowing the lumen close to 80% on the posterior wall of the right main bronchus (Fig. 1b). Since the patient had a negative biopsy, rigid bronchoscopy was performed both for mechanical resection and biopsy after three weeks. It was observed that the lumen of the right main bronchus was 90% occluded with a lobulated endobronchial lesion located on the posterolateral wall with a wide base 5mm after the main bronchus entrance. This lesion was excised from the base with an electrocautery snare probe. On histopathological examination, tumor infiltration with monotonous appearance as small islands vimentin positive and for both anti-smooth muscle actin (SMA) and desmin antibodies, and caldesmon (E89) positive reported (Fig. 1c). The case was diagnosed with glomus tumor in line with these clinical, morphological and immunohistochemical findings. Due to the absence of atypical mitosis and rare mitosis, the case was thought to be compatible with benign glomus tumor. After consulting with the thoracic surgery department, it was decided to perform a right main bronchus sleeve resection on the patient because the mass lesion could be removed and local recurrence was not infrequent. After the surgery, bronchoscopic evaluation indicated no pathological finding and annual chest tomography and bronchoscopic evaluation if indicated were planned during follow up.
Thorax computerized tomography of the patient. (a) Mediastinal and lung window. (b) Bronchoscopic view of the lesion. (c) Hematoxylin eosin sections 40× and 100×, tumoral infiltration in the submucosal forehead, 200×, mitotic cell is shown in the section marked with arrow, 400×, immunohistochemically low Ki67 index, 100×, vimentin positivity 3D.
Glomus tumors are solitary and benign lesions, usually formed by glomus bodies located in the dermis and subcutis layer of the extremities.1 Although it is usually located subungally, cases have been reported rarely in the feet, ankles, knees, hips, thighs, thorax, sacrum and coccyx. However, tracheobronchial and lung parenchyma involvement was extremely rarely reported.2 There were approximately 50 cases with lung involvement reported in the literature that we have reached.3 Cases originating from the endobronchial airways are quite limited.4 The first option in treatment is the surgical resection, there were several cases treated with rigid bronchoscopy. However, local recurrences were reported and were attributed to insufficient excision.5 The World Health Organization divides glomus tumors into three categories: benign, uncertain malignant potential, and malignant. According to the histologic variants, glomus tumors are divided into subtypes of “solid glomus tumor”, “glomangioma” and “glomangiomyoma”, depending on the prominence of glomus cells, vascular structures and smooth muscle. In conclusion, despite having a low incidence, glomus tumor should be kept in mind that close follow-up is required for developing metastasis and local recurrence, especially in cases of lesions above 2cm and atypical mitotic nuclear atypia.
Conflict of InterestsThe authors state that they have no conflict of interests.