The clinical expression of infectious diseases depends largely on microbial damage, but also on the host's immune response, and sometimes the abrupt triggering of this response can worsen the patient's clinical outcome. This situation is called immune reconstitution inflammatory syndrome (IRIS),1 known better since the HIV epidemic.
Although most of IRIS have been described in HIV-infected patients, has been also described in solid organ transplant recipients, neutropenic patients2 and after treatment with tumor necrosis factor-alpha (TNF-α).3
IRIS is a complex entity that continues to be entirely unknown nowadays, although consensus has been reached on the criteria for this diagnosis.1
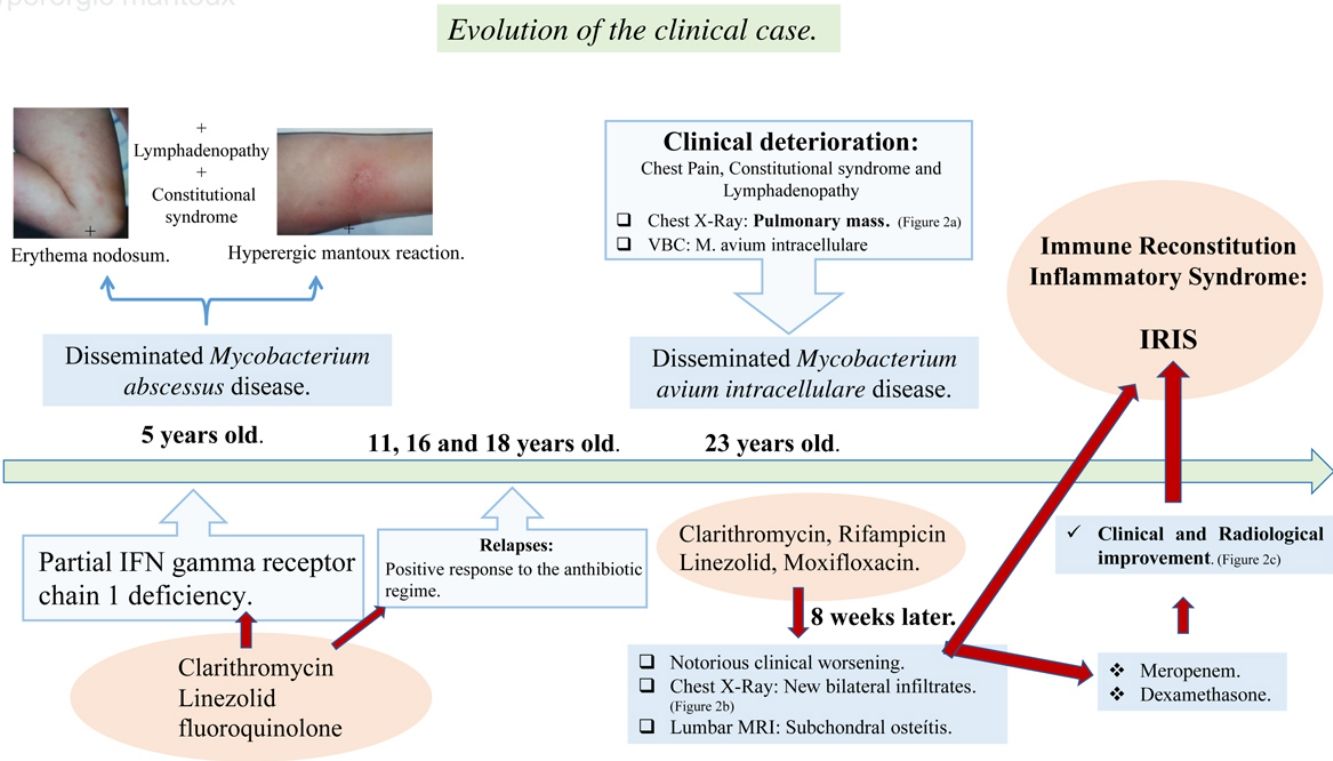
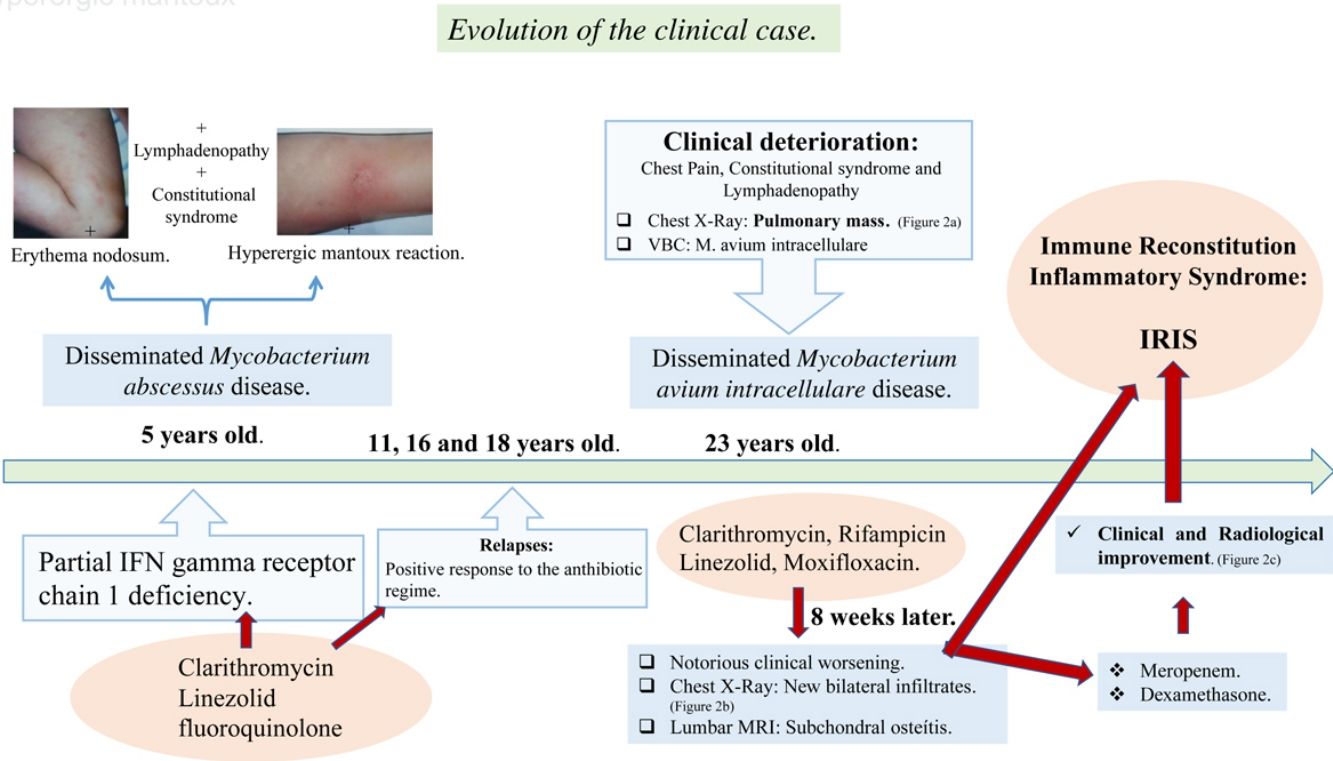
We present the case of a 24-year-old female diagnosed with a partial IFN gamma receptor chain 1 deficiency at 5 years of age, after a disseminated Mycobacterium abscessus disease. An antibiotic regime based on Clarithromycin, Linezolid and a fluoroquinolone was established, with a positive response by the patient in each of the three relapses she experienced for over 15 years.
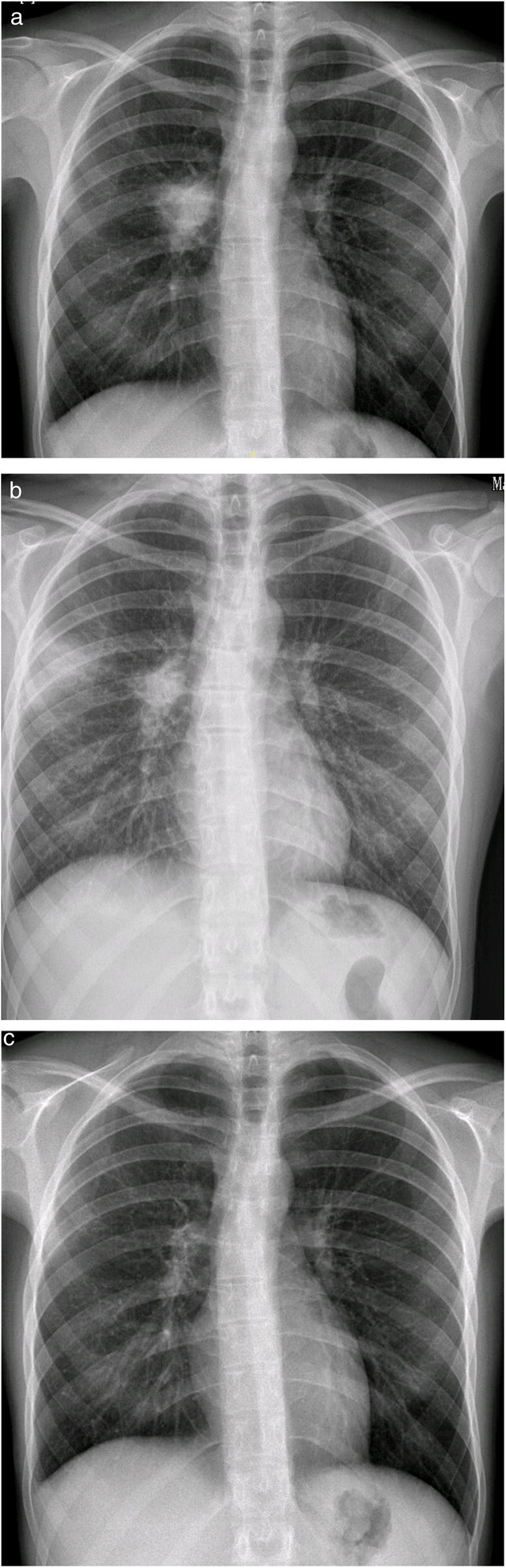
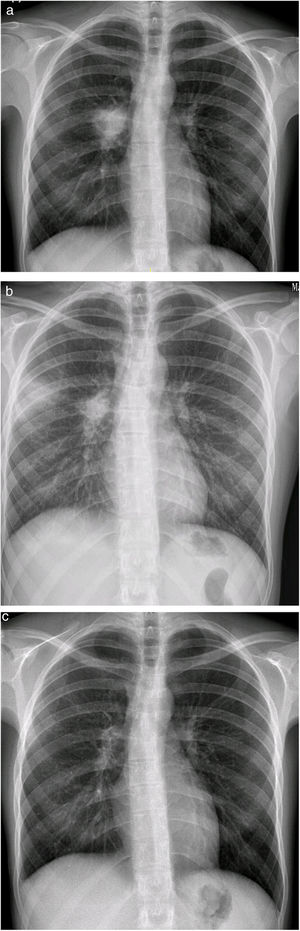
At 23 years of age, she presented a marked clinical deterioration, and the chest X-ray showed a right pulmonary mass that raised the differential diagnosis of several entities, including neoplastic diagnosis (Fig. 1a).
Samples were obtained by video-bronchoscopy and M. avium intracellulare grew in them. Due to the patient's history, it was decided to start antibiotherapy for M. avium intracellulare, but also covering M. abscessus, with clarithromycin, rifampicin, linezolid and moxifloxacin, which immediate clinical improvement.
However, after eight weeks of antibiotherapy, she suffered a notorious clinical worsening: the X-ray showed new bilateral parenchymal infiltrates (Fig. 1b) and the lumbar MRI (severe pain), identified a subchondral osteitis in the soma of L4. These findings led to a suspected diagnosis of disseminated mycobacteriosis and IRIS, like that described in other series.4
Meropenem and dexamethasone (DXM) were added to the treatment, and she experienced gradual clinical and radiological improvement (Fig. 1c) until she was completely asymptomatic after 2 months of treatment, a situation that is still in place at present.
Although IRIS in immunodeficiencies other than HIV infection is scarce, the fact that our patient suffers from a partial deficiency of IFN gamma receptor chain 1 and the worsening after eight weeks of antimycobacterial treatment supports the diagnosis of IRIS,1 especially because the new pulmonary infiltrate and focal lesions in other tissues appeared, both major criteria for IRIS according to INSHI.5 Our diagnosis is also supported by the improvement experienced after the initiation of corticotherapy and with the evolution of the pharmacological treatment.
With an effective treatment there is an immunologic shift from a state of immunosuppression (Treg and Th12) to a state of inflammatory response against the pathogen (Th17 and Th1), triggering an inflammatory storm that would justify the paradoxical worsening observed in our patient.4
IRIS generally presents with a milder course in patients with immunodeficiencies not associated with HIV, and its recovery is also gradual, as it occurred with our patient.2,3
In summary, the diagnosis of IRIS in non-HIV patients requires high clinical suspicion and is based on a series of criteria and clinical parameters that reflect the worsening of an infection or systemic inflammation secondary to the initiation of treatment. Therefore, it is a diagnosis of exclusion.1
FundingThere is no funding related to this article.
Conflict of InterestsThe authors state that they have no conflict of interests.