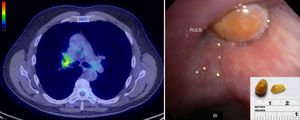
A 59-year-old man with an extensive smoking history presented with a 6-month history of nonproductive cough. Computed tomography (CT) scan of the chest revealed a dense endobronchial lesion in the right upper lobe bronchus (mean 220 Hounsfield units) along with a separate area of pulmonary infiltrate in the peripheral right upper lobe. Positron emission tomography (PET) confirmed increased uptake in the right upper lobe infiltrate and the endobronchial lesion (Fig. 1, left panel; SUVmax 4.3). A bronchoscopy was performed, which revealed a yellowish, smooth, non-vascular mass obstructing the right upper lobe bronchus (Fig. 1, right panel). Diagnostic considerations included foreign body, lipoma and endobronchial carcinoid.
Left panel shows a PET-CT image with an endobronchial lesion in the right upper lobe bronchus with FDG-avidity (SUVmax 4.3). Right panel shows a bronchoscopic image of the right upper lobe endobronchial lesion, and an image of the corn kernel after removal (inset). RULB, right upper lobe bronchus; BI, bronchus intermedius.
We successfully removed a kernel of corn masquerading as an endobronchial tumor (Fig. 1). Increased PET-avidity seen at the site of the endobronchial lesion (SUVmax 4.3) was probably due to the intense granulation tissue that had formed around the foreign body,1 with resultant post-obstructive pneumonia in the right upper lobe. The dense appearance of the kernel on CT may have been caused by a combination of the mineral content (magnesium, phosphorus and iron, amongst others) and desiccated organic matter. At follow-up, 1 week later, the patient reported a significant improvement in cough and recalled aspirating an unpopped microwave popcorn kernel 6 months before the bronchoscopy. Xing et al. have reported a similar case of an aspirated fishbone leading to chronic cough and an endobronchial lesion with surrounding FDG-avidity.2 This report, in addition to our report, highlights the importance of considering inflammation surrounding an aspirated foreign body as a potential mimic of endobronchial malignancy.
The authors would like to acknowledge Drs. Diana Kelm and Sanjay Kalra (Pulmonary and Critical Care Medicine) and Dr. Nathan Marks (Radiology), who were also involved in the clinical management of this patient.
Please cite this article as: Hoskote SS, Saeed AI, Edell ES. Cuerpo extraño endobronquial que imitaba una neoplasia maligna pulmonar con PET positivo. Arch Bronconeumol. 2016;52:484–485.