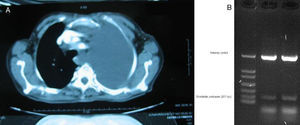
Bordetella pertussis (BP) is a small Gram-negative coccobacillus with an exclusive affinity for the mucous layers of the human respiratory tract.1 BP is an important cause of respiratory disease and it is a persistent public health problem. In 2010, a BP epidemic was detected in the city of Aydin, Turkey.2 Although pleural effusions or empyemas with BP infection are extremely rare, we present a case of non-small-cell lung carcinoma and unilateral pleural effusion with infection due to BP.A 64-year-old woman was hospitalized due to progressive dyspnea and thoracic pain. The patient had a history of non-small-cell lung cancer and she was receiving treatment. Previously, she had smoked 4–5 cigarettes per day for a period of some 10 years. Upon exploration, she showed signs of illness and emaciation, while presenting clinical anemia and signs of massive left pleural effusion on chest CT (Fig. 1). Heart rate was 85bpm, blood pressure 120/85, with no signs of heart failure. Chest radiography confirmed left unilateral effusion. Hemoglobin was 9.1g/100ml, with normochromic and normocytic blood smear. Serum levels of ferritin, vitamin B12 and folate were normal. Erythrocyte sedimentation rate was 90mm/h.Serum levels of electrolytes were normal, as were glycemia and serum calcium. The serum analyses of the liver and thyroid functions were anodyne.Pleural aspiration was performed, and 1500ml of cloudy liquid were obtained. Given the persistence of the pleural liquid collections, two days after the second aspiration a chest drain was inserted. For this pleural drainage, we used a small-caliber catheter. The protein level was 35g/l and the glucose concentration was 0.3mmol/l. No malignant cells were observed, but on PCR the presence of BP was demonstrated. The patient presented neither fever nor clinical manifestations of infection, and blood leucocyte count was normal. In addition, there were no signs of diarrhea and the stool tests, urinalysis and blood cultures were repeatedly negative. Chest computed tomography (CT) (obtained 2 weeks after drainage and treatment with erythromycin, 2mg/day) revealed enlarged mediastinal lymph nodes. The patient presents residual left pleural effusion that has not required new therapeutic drains. Several aspiration samples have remained sterile on culture.Several BP species have been associated with respiratory disease in humans. BP is more frequent and causes more diverse clinical manifestations in pediatric patients. In adolescents and adults, it is frequent for whooping cough to go unnoticed, as the only clinical manifestation may be persistent, unusual cough. Pneumonia is the most frequent complication. Cultures and polymerase chain reaction (PCR) are useful to establish the diagnosis if a sample can be obtained in an early phase of the disease.3 PCR has been widely used for whopping cough since 2001, especially in infants. The increased number of cases reported is due in large part to infection in adolescents and adults, and loss of immunity plays an important role. Although none of the patients presented immunosuppression in the conventional sense (HIV, hematologic disorders or immunosuppressive treatment), all were older patients who had underlying pulmonary problems together with other medical disorders, and all of them belonged to a population of patients that is usually vulnerable to opportunistic infections. All the patients presented signs and symptoms that were clinically compatible with respiratory syndromes caused by BP, and all responded to treatment.4In the literature, we have found no cases similar to ours, only that of a case of pleural effusion caused by B. bronchiseptica reported in a patient with AIDS.5 In the city of Aydin, in 2010 an epidemic of BP was detected,2 and we believe that our case could have originated from this epidemic. Pleural effusions or empyemas with BP infection are extremely infrequent.In our patient, there were diagnostic signs indicative of active infection. Presumably, the empyema was self-limiting. Positive PCR can be determinant in the diagnosis of limited empyema and similar latent infections. We present a very rare case of a patient with non-small-cell lung cancer and unilateral pleural effusion who presented BP infection.
Please cite this article as: Senturk E, et al. Empiema por Bordetella pertussis en un paciente adulto con cáncer de pulmón. Arch Bronconeumol. 2012;48:263–4.