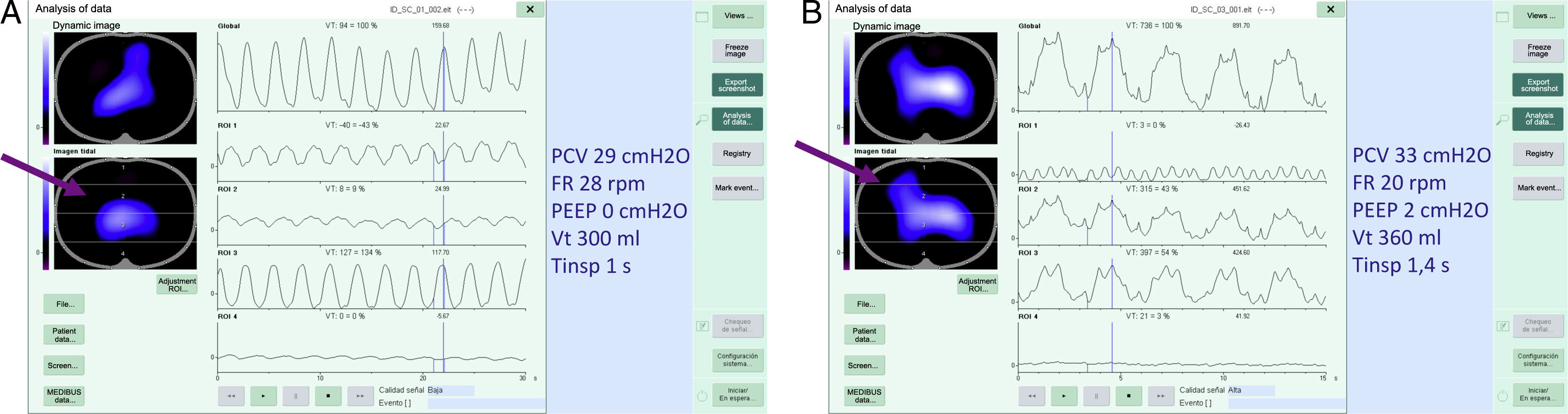
We report the case of a 69-year-old man with a diagnosis of diffuse interstitial lung disease, with a pattern of non-specific interstitial pneumonia. He was admitted to the ICU due to hypoxemic respiratory failure, and began treatment with corticosteroids and cyclophosphamide, and finally required intubation and mechanical ventilation. Static compliance was 10ml/cmH2O, and tidal volume had to be set at around 300ml and PEEP at 2cmH2O to avoid exceeding plateau pressures of 35cmH2O. No optimal PEEP setting could be found that would achieve recruitment. The patient was monitored using the PulmoVista® system (impedance tomography) to evaluate real lack of pulmonary compliance, and to assess ventilatory changes after modifying the respiratory parameters.
The figure shows how only the central part is ventilated on inspiration (Fig. 1A). By increasing the inspiratory time from 1.1s to 1.4s (as well as the other changes indicated in the image), increased ventilation and functional residual capacity could be achieved in the following 24h (Fig. 1B). Impedance tomography is a useful technique for the evaluation of situations of complex ventilatory support.1,2
Please cite this article as: Abella A, Homez M, Conejo I. Tomografía de impedancia eléctrica en un paciente con neumonía intersticial no específica. Arch Bronconeumol. 2017;53:160.