In recent years, the optimal location for noninvasive mechanical ventilation (NIMV) has been a matter of debate. Our aim was to detect the effectiveness of NIMV in acute hypercapnic respiratory failure (AHRF) in respiratory ward and factors associated with failure.
Methods69 patients treated with NIMV in respiratory ward were prospectively evaluated. The success of NIMV was defined as absence of need for intensive care unit (ICU) transfer with patient's dishcarge from hospital (group 1), failure of NIMV was defined as need for ICU transfer (group 2).
ResultsThe mean age was significantly higher in group 2. The cause of respiratory failure was COPD in 51 patients, obesity-hypoventilation syndrome in 14 and kyphoscoliosis in 4 patients. NIMV was successful in 55 patients and unsuccessful in 14. There was no significant difference between the two groups for pretreatment pH, PaCO2 and PaO2/FiO2 After 1h and 3h of NIMV there was significant improvement in group 1. After 3h of NIMV, in group 1 respiratory rate was significantly decreased. The pretreatment APACHE II score, respiratory rate, frequency of pneumoniae, associated complication and comorbid disease was significantly higher in group 2. The success rate was higher in patients with good compliance to NIMV.
ConclusionNIMV can be succesfully applied in patients with AHRF in respiratory ward. The associated factors with NIMV failure are absence of early improvement in blood gases and respiratory rate, bad compliance to NIMV, older age, presence of associated complication, comorbid disease, pneumonia and high baseline respiratory rate.
En los últimos años, la localización óptima de los pacientes sometidos a ventilación mecánica no invasiva (VMNI) ha sido motivo de debate. El objetivo del presente estudio fue determinar la eficacia de esta técnica en pacientes con insuficiencia respiratoria hipercápnica aguda (IRHA), ingresados en una sala de neumología y los factores asociados a su fracaso.
MétodosSe evaluaron prospectivamente 69 pacientes, tratados con VMNI, ingresados en una sala de neumología. Su eficacia se definió como la ausencia de necesidad de traslado a la unidad de cuidados intensivos (UCI) con el alta hospitalaria del paciente (grupo 1), definiéndose su fracaso como la necesidad de traslado a la UCI (grupo 2).
ResultadosLa edad media fue significativamente mayor en el grupo 2. La causa de insuficiencia respiratoria fue una enfermedad pulmonar obstructiva crónica (EPOC) en 51 pacientes, síndrome de obesidad-hipoventilación en 14 y cifoescoliosis en 4. La VMNl fue satisfactoria en 55 pacientes e ineficaz en 14. No se identificaron diferencias significativas entre ambos grupos para los valores pretratamiento de pH, PaCO2 y PaO2/FiO2. Después de 1 y 3 h de VMNl, hubo una mejora significativa en el grupo 1. Después de 3 h de VMNI, en el grupo 1, la frecuencia respiratoria disminuyó significativamente. La puntuación pretratamiento obtenida en la APACHE II, la frecuencia respiratoria, frecuencia de neumonía, complicaciones asociadas y enfermedades comórbidas fueron significativamente más altas en el grupo 2. La tasa de eficacia fue mayor en pacientes con una adhesión adecuada a la VMNL
ConclusiónLa VMNl puede aplicarse eficazmente a pacientes con IRHA ingresados en una sala de neumolo-gía. Los factores asociados a su fracaso son la ausencia de una mejora inicial de los parámetros de la gasometría y de la frecuencia respiratoria, la falta de adhesión a la VMNl, una edad más avanzada, la presencia de complicaciones asociadas, enfermedades comórbidas, neumonía y una mayor frecuencia respiratoria basal.
In recent years noninvasive mechanical ventilation (NIMV), delivered through a facial or nasal mask, has been successfully used in selected populations as an effective treatment for acute hypercapnic respiratory failure (AHRF). In the last decade, randomized controlled trials have shown that the addition of NIMV to standard medical treatment of patients with AHRF improves vital signs and gas exchange, prevents the need for intubation, reduces complications and mortality.1–7 However, the optimal location for NIMV has been a matter of debate. The use of NIMV in the intensive care unit (ICU) has been studied extensively and several reports have recommended that NIMV should be used in the ICU for patients with AHRF.8–9 Although ICU offers the most intensive monitoring and therapeutic capabilities in the hospital for patients with AHRF, this may be impractical, because in most countries the number of ICU beds are limited. Also, since some patients with AHRF are not seriously ill and do not need a close monitoring, it may cause the inconvenient use of resources. Hence, in recent years concern has focused on the use of NIMV outside the ICU (eg. emergency department, regular hospital ward, respiratory ward). Although there are limited studies about this issue, several studies have shown that patients with AHRF can be successfully treated with NIMV outside the ICU. It has also been reported that the use of NIMV in general respiratory wards could theoretically allow the earlier use of NIMV during acute respiratory failure leads to rapid improvement of physiologic variables, reduction in the need for invasive mechanical ventilation and reduction in inhospital mortality.1 However, less monitoring might increase the risk that deterorientation won't be promptly recognized and treated, hence, determining of patients who can be safely treated outside ICU is still unclear. In this prospective observational study, our aim was to evaluate the effectiveness and safety of NIMV in patients with AHRF in a respiratory ward and factors associated with failure.
Material and MethodsThe study was performed in a respiratory ward of tertiary-care university teaching hospital between February 2008 and September 2009. The study protocol is the usual medical therapeutic approach of the hospital for patients with acute respiratory failure and was not implemented for this study. The study protocol was approved by the local ethics committee. Informed consent was obtained from the patients or the first-degree relative. Patients were eligible for the study if they were admitted with AHRF. To be included in the study protocol, patients needed to fulfil the diagnose of AHRF. We defined the AHRF as severe dyspnea, hypercapnia (PaC02>45 mmHg) and a pH ranging between 7.35 and 7.26. Exclusion criteria were: a pH below 7.25, a Glasgow coma scale below 8, pneumothorax, unable to spontaneously clear secretions from the airway, unable to cooperate to NIMV, airway or facial deformity and severe organ disfunction. The diagnosis of chronic obstructive pulmonary disease (COPD) was made on the basis of clinical history, physical examination, chest radiography and spirometry. Acute exacerbation of COPD was characterized by an increase in dyspnea, cough and sputum production. The diagnosis of obesity-hypoventilation syndrome (OHS) was made by obesity (body mass index≥30 kg/m2) and chronic alveolar hypoventilation leading to daytime hypercapnia (PaCO2>45 mmHg), after exclusion of all other causes of alveolar hypoventilation and respiratory failure due to kyphoscoliosis was on the basis of physical examination and radiography with exclusion of all other causes of alveolar hypoventilation. The evaluation of the strength of the cough (0=very weak to 10=very strong) and patient's comfort on NIMV (0=very uncomfortable to 10=very comfortable) was assessed by Licert scale by a physician. All patients received standard medical treatment with oxygen by nasal cannula to maintain arterial saturation at approximately 90%, mucolytics and antibiotics if needed. Chronic obstructive pulmonary diseases patients also received inhaled steroids, bronchodilators and oral steroids (for one week) and teophylline. Patients were ventilated with NIMV using a full face mask. NIMV was initiated by an experienced physician in all patients. The mask best fitting the patient's face was chosen and the tolerance of mask by patient was controlled closely and changed if necessary. The inspiratory positive airway pressure (IPAP) was initially set at 10–12 cmH2O and adjusted according to patient's tolerance to obtain a tidal volume of 7–10 ml/kg with an expiratory positive airway pressure (EPAP) lower than 7 cmH2O. The EPAP was set initially at 5 cmH2O and increased in increments of 1 cmH2O until fractional inspired oxygen (FiO2) requirement was less than 0.5. The humidification was not used during NIMV. Oxygen was added to achieve a SaO2 of>90%. Initially the patients were encouraged to continue NIMV as much as he/she could. Intervals were permitted for eating, drinking or expectoration. When clinical findings and blood gases improved, the duration of NIMV was decreased. For associated complications, factors reported by Jimenez et al were used.10 A post-hoc analysis allowed to differentiate two group of patients, those improving at the pulmonary ward and those requiring ICU admission. While success of NIMV was defined as absence of need for ICU transfer with patient's dishcarge from hospital (group 1), failure of NIMV was defined as need for ICU transfer (group 2). Patients who were deemed unstable (haemodynamic instability, altered state of consciousness), in need of intubation or of closer monitoring were transferred to ICU. For the need of intubation, the criteria used by Brochard et al. were used.2 Endotracheal intubation was considered if any of the following criteria were met: (1) pH below 7.20, (2) pH: 7.20–7.25 on two occasions 1 h apart, (3) hypercapnic coma (GCS<8 and PaCO2>8kPa), (4) PaO2 below 6 kPa despite maximum tolerated FiO2 and (5) cardiorespiratory arrest.
Statistical AnalysisAll statistical analyses were performed using the SPSS version 10.0. For the comparison of groups, T-test, Chi-Square test and Mann-Whitney test were used. For variables that were not normally distributed, nonparametric test were used. For both groups, comparison of baseline pH, PaCO2 and PaO2/FiO2 with those recorded after NIMV was performed using multiple comparison test and Friedman test with Bonferroni correction. A p value of less than 0.05 was considered as statistically significant.
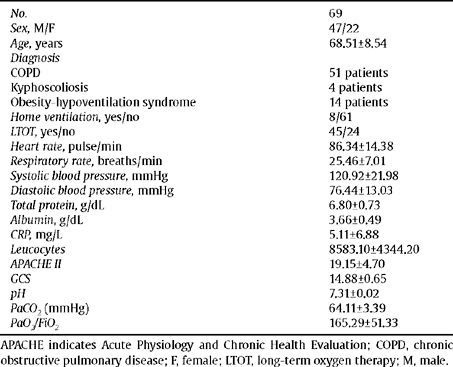
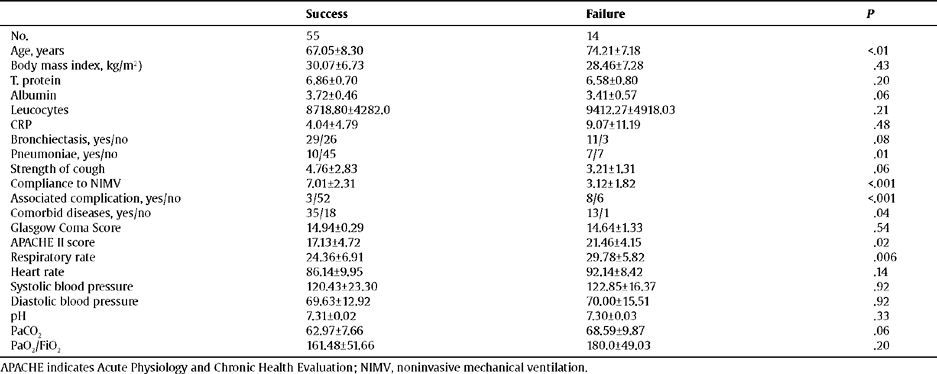
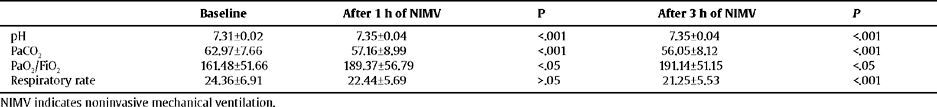
Results69 patients with AHRF treated with NIMV were enrolled in the study. Baseline characteristics of study group were shown in table 1. Eight patients in the study group were on domiciliary ventilation and 45 patients were on long-term oxygen therapy (LTOT). The cause of respiratory failure was COPD exacerbation in 51 patients, obesity-hypoventilation syndrome (OHS) in 14 and kyphoscoliosis in 4 patients. NIMV was successful in 55 patients (79.7%) (group 1) and failed in remainder 14 patients (group 2). NIMV was successful in 41 of 51 patients with COPD, 3 of 4 patients with kyphoscoliosis, and 11 of 14 patients with OHS. Table 2 shows the comparison of the success and failure groups. At entry, total protein, albumin, CRP, leucocyte count, heart rate, systolic, diastolic blood pressure, GCS and strength of cough did not preclude the patients' response to NIMV. There was no significant difference between two groups for pretreatment pH, PaCO2 and PaO2/FiO2 however, after 1h and 3h of NIMV there was a significant improvement in group 1, while there was no improvement in group 2 (Table 3 and 4). In success group, after 3h of NIMV the respiratory rate was significantly decreased (Table 3). The mean age was significantly higher in group 2. The pretreatment APACHE II score, respiratory rate, frequency of pneumoniae, associated complication and concomitant disease was significantly higher in group 2. The success rate was significantly higher in patients with good compliance to NIMV. In success group, there was associated complication in 3 of 55 patients (5.5%) while 8 of 14 (57.1%) in failure group.
Characteristics of the study group: parameters recorded at admission
| No. | 69 |
| Sex, M/F | 47/22 |
| Age, years | 68.51±8.54 |
| Diagnosis | |
| COPD | 51 patients |
| Kyphoscoliosis | 4 patients |
| Obesity-hypoventilation syndrome | 14 patients |
| Home ventilation, yes/no | 8/61 |
| HOT, yes/no | 45/24 |
| Heart rate, pulse/min | 86.34±14.38 |
| Respiratory rate, breaths/min | 25.46±7.01 |
| Systolic blood pressure, mmHg | 120.92±21.98 |
| Diastolic blood pressure, mmHg | 76.44±13.03 |
| Total protein, g/dL | 6.80±0.73 |
| Albumin, g/dL | 3.66±0.49 |
| CRP, mg/L | 5.11±6.88 |
| Leucocytes | 8583.10±4344.20 |
| APACHE II | 19.15±4.70 |
| GCS | 14.88±0.65 |
| pH | 7.31±0.02 |
| PaC02 (mmHg) | 64.11±3.39 |
| PaO2/Fi02 | 165.29±51.33 |
APACHE indicates Acute Physiology and Chronic Health Evaluation; COPD, chronic obstructive pulmonary disease; F, female; LTOT, long-term oxygen therapy; M, male.
Comparison of failure and success groups regarding baseline features
| Success | Failure | P | |
| No. | 55 | 14 | |
| Age, years | 67.05±8.30 | 74.21±7.18 | <.01 |
| Body mass index, kg/m2) | 30.07±6.73 | 28.46±7.28 | .43 |
| T. protein | 6.86±0.70 | 6.58±0.80 | .20 |
| Albumin | 3.72±0.46 | 3.41±0.57 | .06 |
| Leucocytes | 8718.80±4282.0 | 9412.27±4918.03 | .21 |
| CRP | 4.04±4.79 | 9.07± 11.19 | .48 |
| Bronchiectasis, yes/no | 29/26 | 11/3 | .08 |
| Pneumoniae, yes/no | 10/45 | 7/7 | .01 |
| Strength of cough | 4.76±2.83 | 3.21±1.31 | .06 |
| Compliance to NIMV | 7.01±2.31 | 3.12±1.82 | <.001 |
| Associated complication, yes/no | 3/52 | 8/6 | <.001 |
| Comorbid diseases, yes/no | 35/18 | 13/1 | .04 |
| Glasgow Coma Score | 14.94±0.29 | 14.64±1.33 | .54 |
| APACHE II score | 17.13±4.72 | 21.46±4.15 | .02 |
| Respiratory rate | 24.36±6.91 | 29.78±5.82 | .006 |
| Heart rate | 86.14±9.95 | 92.14±8.42 | .14 |
| Systolic blood pressure | 120.43±23.30 | 122.85±16.37 | .92 |
| Diastolic blood pressure | 69.63±12.92 | 70.00±15.51 | .92 |
| pH | 7.31±0.02 | 7.30±0.03 | .33 |
| PaCO2 | 62.97±7.66 | 68.59±9.87 | .06 |
| PaO2/FiO2 | 161.48±51.66 | 180.0±49.03 | .20 |
APACHE indicates Acute Physiology and Chronic Health Evaluation; NIMV, noninvasive mechanical ventilation.
Comparison of baseline and after NIMV blood gases and respiratory rate in success group
| Baseline | After lh of NIMV | P | After 3 h of NIMV | P | |
| pH | 7.31+0.02 | 7.35+0.04 | <.001 | 7.35+0.04 | <.001 |
| PaCO2 | 62.97±7.66 | 57.16±8.99 | <.001 | 56.05±8.12 | <.001 |
| PaO2/FiO2 | 161.48±51.66 | 189.37±56.79 | <.05 | 191.14±51.15 | <.05 |
| Respiratory rate | 24.36±6.91 | 22.44±5.69 | >.05 | 21.25±5.53 | <.001 |
NIMV indicates noninvasive mechanical ventilation.
Comparison of baseline and after NIMV blood gases and respiratory rate in failure group
| Baseline | After lh of NIMV | P | After 3 h of NIMV | P | |
| pH | 7.30±0.03 | 7.29±0.04 | >.05 | 7.28±0.04 | >.05 |
| PaCO2 | 68.59+9.87 | 69.46+8.43 | >.05 | 68.72+8.92 | >.05 |
| PaO2/FiO2 | 180.0+49.03 | 169.71+30.68 | >.05 | 176.0+29.53 | >.05 |
| Respiratory rate | 29.78±5.82 | 27.02±5.12 | >.05 | 27.16±4.87 | >.05 |
NIMV indicates noninvasive mechanical ventilation.
The duration of hospitalization was significantly lower in success group (13.75±8.52 vs 22.55±15.42 days). The total duration of NIMV therapy was 70.28±56.06 hours in success group and 18.64±14.02 in failure group before being admitted to ICU.
Of the 14 patients transferred to ICU, 7 patients were immediately intubated and invasive mechanical ventilation (IMV) was performed. In the remainder 7 patients, NIMV was continued in ICU, however 3 patients required intubation in the first day of ICU. Overall, 5 of 14 patients transferred to ICU died and 9 patients were dishcarged from hospital.
Chronic obstructive pulmonary disease was the leading cause of AHRF in the study group and this subgroup was separately evaluated. In COPD patients, there was no significant difference between patients managed successfully versus unsuccessfully with regard to baseline total protein, albumin, CRP, leucocyte count, heart rate, systolic, diastolic blood pressure, GCS, strength of cough, concomitant disease and blood gases. However, pretreatment APACHE II score, respiratory rate, frequency of pneumoniae and associated complication was significantly higher in failure group. In contrast with all study group, the presence of bronchiectasis (53.7% vs. 90%) was significantly higher in failure group. After 1h and 3h, a significant improvement in pH, PaCO2 and PaO2/FiO2 and respiratory rate was observed in success group. The success rate was also significantly higher in patients with good compliance to NIMV.
DiscussionNoninvasive positive pressure ventilation has been shown as an effective treatment of AHFR caused by various diseases preventing endotracheal intubation in 60–90% of patients.11 Most of studies regarding use of NIMV have been performed in ICU and some guidelines recommended initiating NIMV for acute respiratory failure in the ICU setting, however, since there is a general shortage of beds in ICUs and this approach may lead an inconvenient use of resources, in recent years the optimal location for NIMV has been a matter of debate.
In several studies, the safety and effectiveness of NIMV in ARF outside of ICU has been evaluated. In one randomised trial, Wood et al. found that the use of NIMV in emergency department (ED) delayed intubation and a strong trend toward higher mortality, however in this study, the groups were not well matched.12 In a subsequent study, Poponick et al. performed bilevel pressure ventilation trials on 58 patients in ED and found that, in 43 patients (74.1%) NIMV was successful.13 In another study in which 50 patients were treated with NIMV in ED, the success of NIMV was 86% and authors concluded that the use of NIMV in the ED is feasable and has potential utility.14 In a recent study by Miguel-Yanes et al. it has been reported that NIMV is a relatively safe and effective treatment in the ED.15
NIMV may also be performed in respiratory ward during ARF. However, only a few series have described NIMV use for ARF in this setting. In an early study made by Corbetta et al. in a respiratory ward, 40 patients recieved NIMV were compared with 30 patients recieved conventional treatment.11 Compared to conventional treatment, NIMV was associated with a reduction in intubation and mortaility rate. Scala et al. tried NIMV in 207 patients with AHRF in a respiratory ward and reported that arterial blood gases significantly improved after two hours of NIMV and NIMV succeeded in avoiding intubation in 169/207 patients (81.6%).16 Castillo et al. included 41 patients with acute exacerbation of COPD and randomised to NIMV and standard therapy, they found that the use of NIMV significantly reduced the respiratory rate and improved conscious level within the first 2 h.17 There were also significant differences in PaCO2 and pH levels. The need for intubation was 5% in the NIMV group and 14% in the control group. In a prospective mulitcentre randomised controlled study, 236 patients with acute exacerbation of COPD with mild to moderate acidosis were randomised to standard therapy and NIMV on respiratory ward.1 In this study, the failure criteria was the need for intubation, and the authors found that the use of NIMV significantly reduced the need for intubation and in-hospital mortality. The success rate was 85% in NIMV group. In another prospective multicentre randomised controlled study, 342 acute exacerbation of COPD patients with pH≥7.25 and PaCO2>45 mmHg were recruited on general ward and randomly assigned to standard medical treatment or early administration of additional NIMV and the authors concluded that early use of NIMV on general ward improves arterial blood gases and respiratory pattern, decreases the rate of need for intubation (8/171 in NIMV group vs 26/171 in control group).18
In the presented study, the success of NIMV was defined as absence of need for ICU transfer with patient's dishcarge from hospital and we found the success rate as 79.7% similar with these previous reports and also similar to that reported in series in which NIMV was used in the ICU. In majority of studies, NIMV was performed in patients with acute exacerbation of COPD. In contrast, our study group was heterogenous regarding the diagnosis. NIMV was successful in 41 of 51 (80.39%) patients with COPD, 11 of 14 (78.57%) patients with OHS and 3 of 4 (75%) patients with kyphoscoliosis. We couldn't compare NIMV success between each disease due to small number of patients with non COPD diseases. However, we evaluated COPD patients separately, and found that the associated factors with NIMV failure was similar with all study group, except the presence of bronchiectasis predicted failure in COPD patients.
Selection of appropriate patient is crucial for the optimization of NIMV success rates and predictors of success or failure may be helpful in selecting patients. Although predictors or associated factors of success have been well described in ICU setting,19 in respiratory ward applications, only in a few studies it has been evaluated.16,20 In the study performed by Scala et al. NIMV failure was independently predicted by Activity of Daily Living Score, pneumonia as cause of ARF and APACHE score.16 Farha et al. studied NIMV in 76 patients with ARF in general hospital ward.20 In their study, variables associated with NIMV failure were amount of secretions, etiology of respiratory failure (pneumonia was associated with the highest failure rate) and infiltrates on the chest radiograph. In our study, patients were divided into two groups according to outcome of NIMV and we investigated the associated factors with NIMV failure. Our findings were consistent with previous reports in which NIMV was used in the ICU and best predictor of success was reported as favorable response to NIMV in first 2h.19,21,22 The most commonly used indexes of severity of illness are APACHE II and Simplified Acute Physiology Score (SAPS II) and in studies performed in ICU, it has been reported that high APACHE II score is a predictor of NIMV failure.21,23 Similar with these reports, we found a significantly higher APAPCHE II score in failure group. We investigated whether the presence of associated complication on admission, modified by Jimenez et al, can predict NIMV success/failure. The rate of presence of associated complication was significantly higher in failure group. The pretreatment respiratory rate, the presence of comorbid disease (35/55 in success vs 13/14 in failure group) and pneumonia (10/55 in success vs 7/14 in failure group) were significantly higher in failure group. We used Licert scale to assess whether compliance to NIMV can predict success and found that the success rate was significantly higher in patients with good compliance to NIMV.
In conclusion, in presented study the success rate of NIMV in respiratory ward was comparable to that series in which NIMV was used in ICU. NIMV succeeded in avoiding ICU transfer in 79.7% of patients, hence we suggested that NIMV can be successfully applied in respiratory ward in majority of patients. However, associated factors with NIMV failure are absence of early improvement in blood gases and respiratory rate, bad compliance to NIMV, older age, presence of complication, comorbid disease, pneumoniae (50% of failures were patients with pneumonia), pretreatment high respiratory rate and finally, different from all study group, the presence of bronchiectasis in COPD patients. These patients should be considered for initiating NIMV in ICU or for an early transfer to ICU.