Community-acquired pneumonia increases the risk of cardiovascular events (CVE). The objective of this study was to analyze host, severity, and etiology factors associated with the appearance of early and late events and their impact on mortality.
MethodProspective multicenter cohort study in patients hospitalized for pneumonia. CVE and mortality rates were collected at admission, 30-day follow-up (early events), and one-year follow-up (late events).
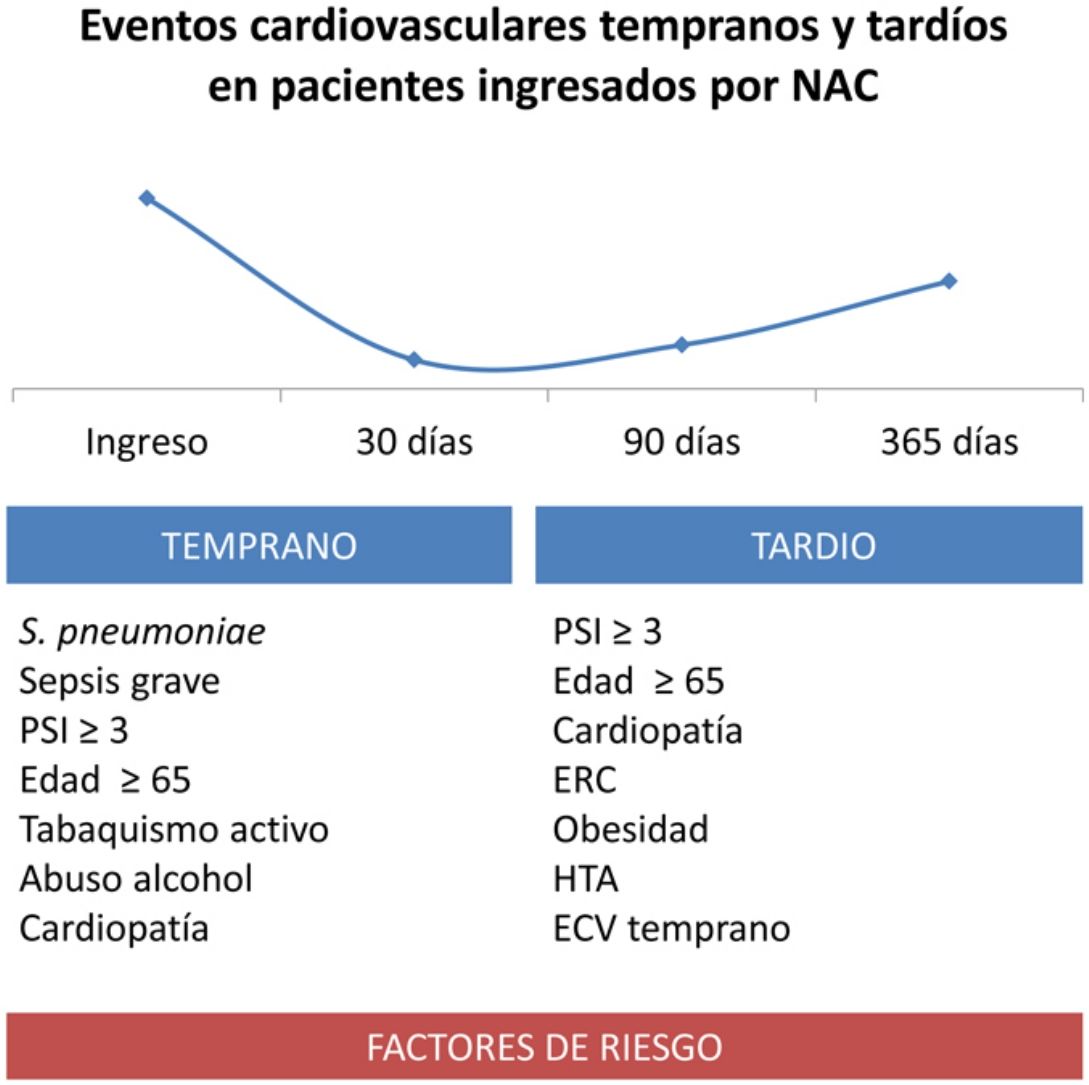
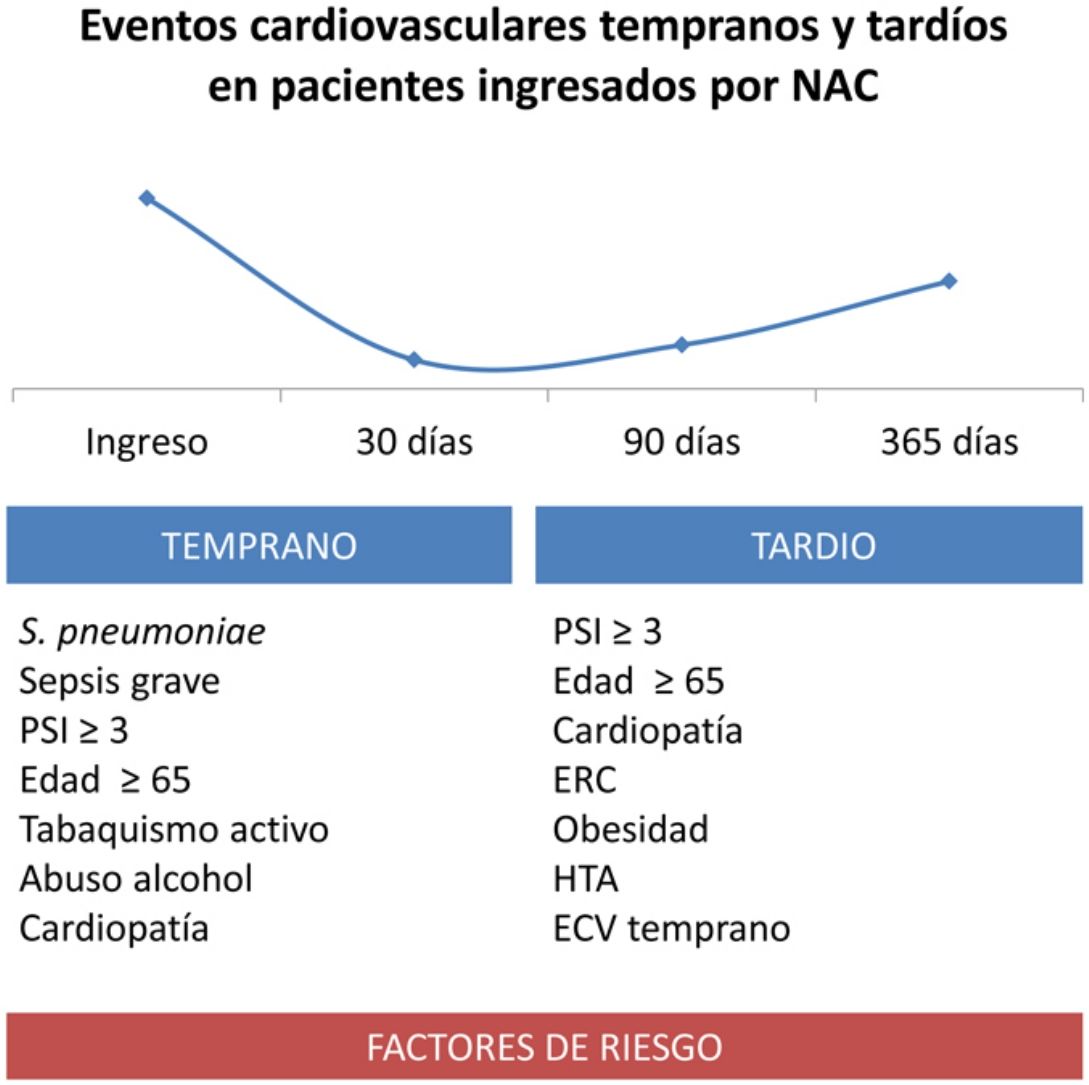
ResultsIn total, 202 of 1967 (10.42%) patients presented early CVE and 122 (6.64%) late events; 16% of 1-year mortality was attributed to cardiovascular disease. The host risk factors related to cardiovascular complications were: age ≥ 65 years, smoking, and chronic heart disease. Alcohol abuse was a risk factor for early events, whereas obesity, hypertension, and chronic renal failure were related to late events. Severe sepsis and Pneumonia Severity Index (PSI) ≥ 3 were independent risk factors for early events, and only PSI ≥ 3 for late events. Streptococcus pneumoniae was the microorganism associated with most cardiovascular complications. Developing CVE was an independent factor related to early (OR 2.37) and late mortality (OR 4.05).
ConclusionsAge, smoking, chronic heart disease, initial severity, and S. pneumoniae infection are risk factors for early and late events, complications that have been related with an increase of the mortality risk during and after the pneumonia episode. Awareness of these factors can help us make active and early diagnoses of CVE in hospitalized CAP patients and design future interventional studies to reduce cardiovascular risk.
La neumonía adquirida en la comunidad se asocia al desarrollo de eventos cardiovasculares (ECV). El objetivo del estudio fue analizar los factores relativos al huésped, la gravedad y la etiología que se asocian con la aparición de estos eventos, tempranos y tardíos, y su impacto en la mortalidad.
MétodoEstudio prospectivo de cohortes multicéntrico en pacientes ingresados por neumonía. Se recogieron ECV durante el ingreso, a los 30 días (tempranos) y al año (tardíos) y la mortalidad.
ResultadosDoscientos dos de 1.967 (10,42%) pacientes presentaron ECV tempranos y 122 (6,64%) tardíos. El 16% de la mortalidad al año se atribuyó a complicaciones cardiovasculares. Los factores del huésped relacionados con complicaciones cardiovasculares fueron: edad ≥ 65 años, abuso de alcohol, tabaquismo y cardiopatía crónica en los tempranos y obesidad, HTA e insuficiencia renal crónica en los tardíos. La presencia de sepsis grave y Pneumonia Severity Index (PSI) ≥ 3 fueron factores de riesgo independiente de eventos tempranos y, únicamente, el PSI ≥ 3 de los tardíos. Streptococcus pneumoniae fue el microorganismo con mayor riesgo de complicaciones cardiovasculares. Desarrollar un ECV fue factor independiente de mortalidad temprana (OR 2,37) y tardía (OR 4,05).
ConclusionesLa edad, el tabaquismo, la cardiopatía, la gravedad inicial y el S. pneumoniae son factores de riesgo de presentar ECV tempranos y tardíos, lo que conlleva mayor mortalidad durante y tras el episodio agudo de neumonía. Conocer estos factores puede ser de utilidad para desarrollar estrategias activas de diagnóstico precoz de eventos y/o diseñar ensayos dirigidos a reducir las complicaciones cardiovasculares.
Interest has grown in recent years in the association between infection and the development of cardiovascular events (CVE).1,2 Community-acquired pneumonia (CAP) is a very common infection that carries a mortality burden of 5%–15%,3 and causes cardiovascular (CV) complications that can occur during both the acute and late phases of the episode: the CV risk remains higher for a considerable period of time (10 years),4,5 and the death rate is as high as 30%.4,6 The reported frequency of CVE in CAP ranges between 12% and 30%,7,8 according to studies with different follow-up periods.
The main hypothesis put forward to explain this nexus is that CAP triggers the action of various mechanisms, such as inflammatory, local and systemic response, hypoxemia, vascular endothelial dysfunction, and the induction of a prothrombotic state.9–12 Direct myocardial damage caused by Streptococcus pneumoniae has also been demonstrated in animal models.13 Both prolonged inflammatory response over time and cardiovascular damage can be subclinical during the acute episode. This can lead to complications that appear subsequent to the infection, such as acute myocardial infarction, heart failure, arrhythmia, stroke, and others. Factors such as age or initial severity of the pneumonia appear to influence the development of complications and/or mortality during the acute stage and for a period of up to 30 days.8 Most studies analyze factors associated with the appearance of early CVE, but fail to analyze the potential long-term effect. Our hypothesis is that the different risk factors associated with host characteristics, initial severity of the episode, and the causative microorganism, impact differently on the appearance of early and late CVE in the Spanish population.
Our objective was to analyze whether host characteristics, initial severity of pneumonia, and etiology independently influence the development of early (up to 30 days) and late (up to one year) CVE, and the impact of CVE on mortality.
MethodsStudy design and patientsThis was a prospective, multicenter cohort study in adult patients admitted for CAP in 9 Spanish hospitals. Between June 2012 and June 2015, patients with clinical symptoms of acute respiratory infection and new infiltrate on chest X-ray who provided signed informed consent were recruited sequentially into the study. In 1 center, only patients with pneumonia caused by S. pneumoniae were included. Patients were excluded if they were immunocompromised, if their treatment was limited due to terminal disease, or if they had been hospitalized within 15 days before developing clinical symptoms. The study was approved by the Ethics Committee of the site that was coordinating the study.
Demographic data, comorbidities, previous treatment, and clinical, radiological, and laboratory data were collected during the acute episode. Comorbidity was defined according to previous published studies14 as: cardiac (coronary heart disease, congestive heart failure, arrhythmia or valvular disease), pulmonary (asthma, COPD or fibrosis), renal disease prior to the pneumonia episode, chronic liver disease, neurological disease (of any etiology), diabetes mellitus, and neoplastic disease that was active or treated in the previous year. Infection severity was quantified using the Pneumonia Severity Index (PSI) scale,15 as this is the most widely used tool both in Spain and internationally. Severe respiratory failure (PaO2 /FiO2 < 250 mmHg) and sepsis with organ dysfunction (according to the criteria established at the 2001 SCCM/ESICM/ACCP/ATS/SIS International Conference) were specifically collected.16
Microbiological studies included: pneumococcal and Legionella antigen in urine, blood culture on admission, and atypical bacteria serologies. Gram testing and culture were performed in sputum from patients with expectoration. Sampling using invasive procedures and study of pharyngeal smears for virus were performed at the discretion of the treating physician.
Follow-up was conducted during hospital admission and 30 days after discharge. Patients were then monitored by telephone contact and electronic medical record review at 90 days and at 1 year.
Cardiovascular eventsEvents were divided into early (occurring between diagnosis and 30-day follow-up) and late (between 30-day follow-up and 1 year) groups. The following CVE were targeted: cerebrovascular accident (stroke and transient ischemic attack), pulmonary embolism and/or deep vein thrombosis, acute coronary syndrome (acute myocardial infarction and unstable angina), onset or worsening of cardiac arrhythmia, and de novo heart failure or worsening of pre-existing heart failure. Infarction was diagnosed when an increase and/or fall in troponin T with at least 1 result above the 99th percentile of the upper reference limit along with one of the following criteria was detected: 1) symptoms of ischemia; 2) ischemic electrocardiographic changes: appearance of Q waves, ST segment elevation greater than 2 mm in two contiguous leads in V1, V2, V3 and 1 mm in all other leads, ST segment depression or T wave inversion, or the appearance of new left bundle branch block; 3) ultrasound imaging showing non-viable myocardium or focal alteration of new-onset myocardial contractility.
The same time periods were applied for mortality, early (up to 30 days) and late (from 30 days to 1 year), differentiating between all-cause and CVE mortality.
Statistical analysisThe statistical analysis was performed using the SPSS (version 20.0) and R statistical packages. Qualitative variables were expressed as percentages and compared using the Chi-square test. Quantitative variables were expressed as mean or median and interquartile range, and compared using parametric and non-parametric tests. The PSI value was taken as a continuous quantitative variable and as an ordinal quantitative variable (grades < 3, 3, 4, and 5). Multivariate logistic regression was used to predict the development of early and late CVE (dependent variables). Three models were constructed for the study of each dependent variable: variables associated with host characteristics (model 1), severity of the CAP episode (model 2), and causative microorganisms (model 3). Two logistic regressions were also performed to predict early and late mortality (dependent variables) using as independent variables age, PSI, PaO2/FiO2 < 250 mmHg, and the appearance of CVE at admission for early mortality, and early CVE for late mortality. Statistical significance for all analyses was established at a p value < 0.05.
ResultsOf the 2011 patients initially included in the study, 44 were excluded from the analysis because of lack of data. Of these 1967 initial patients, 1866 were assessed in an in-person visit at 30 days (100 deaths and 1 lost to follow-up). At 1 year, 1710 patients were evaluated (98 deaths and 58 lost to follow-up). Of the 1967 patients included, 60.7% were men with a mean age of 66 years. Arterial hypertension (AHT) (39.6%), followed by chronic heart disease (27.8%) and chronic lung disease (24.4%), were the most frequent comorbidities. An etiological diagnosis was achieved in 1014 patients (51.6%), with S. pneumoniae being the main causative agent in 688 patients (67.8%); 205 patients had invasive pneumococcal disease (IPD). Other etiologies were mixed (11.2%), atypical (12.3%), and viral (9.8%). Overall, 49% of patients had severe sepsis on admission and 24% had severe respiratory failure; 102 patients (10.2%) were admitted to intensive care units and 34 (1.2%) to intermediate respiratory care units.
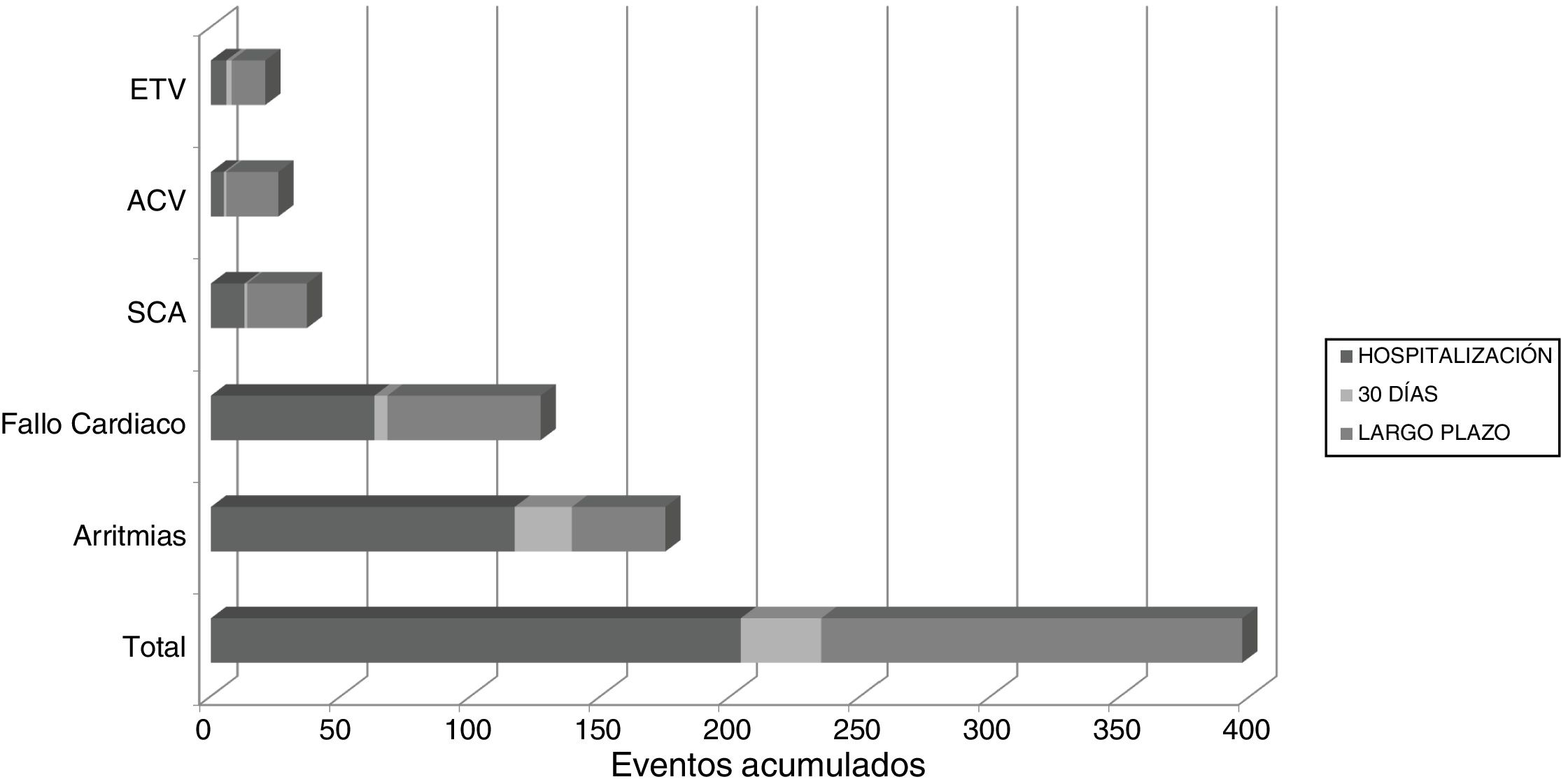
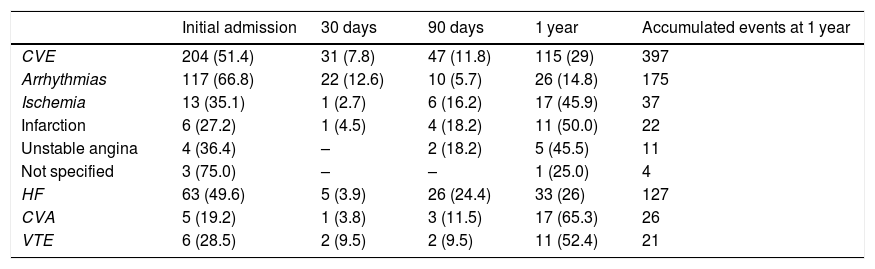
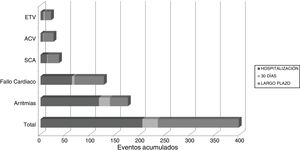
Appearance of cardiovascular eventsUnivariate study. A total of 202 (10.42%) patients had early CVEs and 122 (6.64%) had late CVEs (Table 1); 6.8% of patients with early CVE also had late CVE. Overall, 20% of patients with CVE had 2 or more complications in the same episode during follow-up. A total of 397 CVE were recorded: 235 early and 163 late (Fig. 1). Throughout the follow-up period, 11 patients developed AHT de novo (0.6%) and 7 patients were diagnosed with diabetes mellitus (0.4%).
In-hospital, 30-day, and long-term cardiovascular events.
| Initial admission | 30 days | 90 days | 1 year | Accumulated events at 1 year | |
|---|---|---|---|---|---|
| CVE | 204 (51.4) | 31 (7.8) | 47 (11.8) | 115 (29) | 397 |
| Arrhythmias | 117 (66.8) | 22 (12.6) | 10 (5.7) | 26 (14.8) | 175 |
| Ischemia | 13 (35.1) | 1 (2.7) | 6 (16.2) | 17 (45.9) | 37 |
| Infarction | 6 (27.2) | 1 (4.5) | 4 (18.2) | 11 (50.0) | 22 |
| Unstable angina | 4 (36.4) | – | 2 (18.2) | 5 (45.5) | 11 |
| Not specified | 3 (75.0) | – | – | 1 (25.0) | 4 |
| HF | 63 (49.6) | 5 (3.9) | 26 (24.4) | 33 (26) | 127 |
| CVA | 5 (19.2) | 1 (3.8) | 3 (11.5) | 17 (65.3) | 26 |
| VTE | 6 (28.5) | 2 (9.5) | 2 (9.5) | 11 (52.4) | 21 |
CVA: cerebrovascular accident; CVE: cardiovascular events recorded in each follow-up period, expressed in absolute number (percentage of total accumulated events at 1 year for each event type); HF: Heart failure; Ischemia: ischemic events broken down into subtypes; VTE: venous thromboembolic disease.
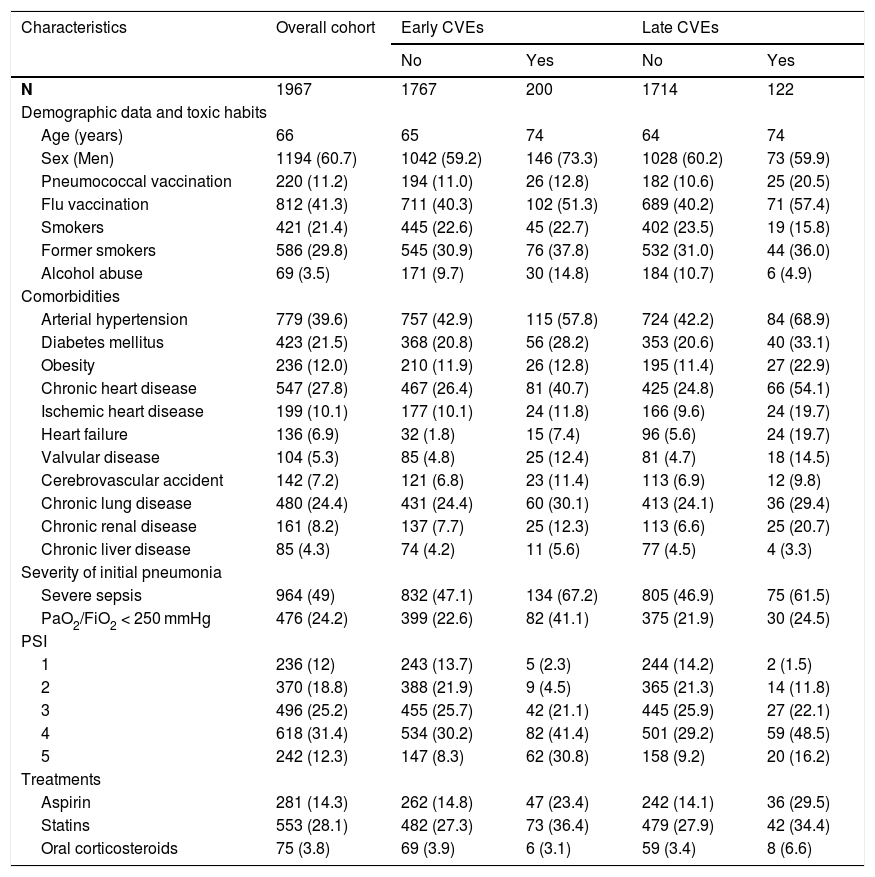
Table 2 summarizes patient characteristics. The group of patients who developed CVE was older and had more comorbidities, mainly HT, diabetes, obesity, stroke, and chronic heart disease, and a higher initial severity of pneumonia. More patients with pneumococcal pneumonia developed CVE compared to other etiologies, 12.5% vs. 7.7% (P = 0.051), and up to 17.7% in IPD vs. 9.3% in non-IPD (P = 0.006). Early CVEs occurred in 11% patients with pneumococcal CAP vs. 5.7% of those with another etiology (P = 0.014) and in 15.5% with IPD vs. 7.7% non-IPD (P = 0.003). No differences were found for late events, which occurred in 2.9% of patients with pneumococcal CAP and 4.7% in CAP with another etiology (P = 0.181).
Characteristics of the overall cohort and by development or non-development of early and late cardiovascular events.
| Characteristics | Overall cohort | Early CVEs | Late CVEs | ||
|---|---|---|---|---|---|
| No | Yes | No | Yes | ||
| N | 1967 | 1767 | 200 | 1714 | 122 |
| Demographic data and toxic habits | |||||
| Age (years) | 66 | 65 | 74 | 64 | 74 |
| Sex (Men) | 1194 (60.7) | 1042 (59.2) | 146 (73.3) | 1028 (60.2) | 73 (59.9) |
| Pneumococcal vaccination | 220 (11.2) | 194 (11.0) | 26 (12.8) | 182 (10.6) | 25 (20.5) |
| Flu vaccination | 812 (41.3) | 711 (40.3) | 102 (51.3) | 689 (40.2) | 71 (57.4) |
| Smokers | 421 (21.4) | 445 (22.6) | 45 (22.7) | 402 (23.5) | 19 (15.8) |
| Former smokers | 586 (29.8) | 545 (30.9) | 76 (37.8) | 532 (31.0) | 44 (36.0) |
| Alcohol abuse | 69 (3.5) | 171 (9.7) | 30 (14.8) | 184 (10.7) | 6 (4.9) |
| Comorbidities | |||||
| Arterial hypertension | 779 (39.6) | 757 (42.9) | 115 (57.8) | 724 (42.2) | 84 (68.9) |
| Diabetes mellitus | 423 (21.5) | 368 (20.8) | 56 (28.2) | 353 (20.6) | 40 (33.1) |
| Obesity | 236 (12.0) | 210 (11.9) | 26 (12.8) | 195 (11.4) | 27 (22.9) |
| Chronic heart disease | 547 (27.8) | 467 (26.4) | 81 (40.7) | 425 (24.8) | 66 (54.1) |
| Ischemic heart disease | 199 (10.1) | 177 (10.1) | 24 (11.8) | 166 (9.6) | 24 (19.7) |
| Heart failure | 136 (6.9) | 32 (1.8) | 15 (7.4) | 96 (5.6) | 24 (19.7) |
| Valvular disease | 104 (5.3) | 85 (4.8) | 25 (12.4) | 81 (4.7) | 18 (14.5) |
| Cerebrovascular accident | 142 (7.2) | 121 (6.8) | 23 (11.4) | 113 (6.9) | 12 (9.8) |
| Chronic lung disease | 480 (24.4) | 431 (24.4) | 60 (30.1) | 413 (24.1) | 36 (29.4) |
| Chronic renal disease | 161 (8.2) | 137 (7.7) | 25 (12.3) | 113 (6.6) | 25 (20.7) |
| Chronic liver disease | 85 (4.3) | 74 (4.2) | 11 (5.6) | 77 (4.5) | 4 (3.3) |
| Severity of initial pneumonia | |||||
| Severe sepsis | 964 (49) | 832 (47.1) | 134 (67.2) | 805 (46.9) | 75 (61.5) |
| PaO2/FiO2 < 250 mmHg | 476 (24.2) | 399 (22.6) | 82 (41.1) | 375 (21.9) | 30 (24.5) |
| PSI | |||||
| 1 | 236 (12) | 243 (13.7) | 5 (2.3) | 244 (14.2) | 2 (1.5) |
| 2 | 370 (18.8) | 388 (21.9) | 9 (4.5) | 365 (21.3) | 14 (11.8) |
| 3 | 496 (25.2) | 455 (25.7) | 42 (21.1) | 445 (25.9) | 27 (22.1) |
| 4 | 618 (31.4) | 534 (30.2) | 82 (41.4) | 501 (29.2) | 59 (48.5) |
| 5 | 242 (12.3) | 147 (8.3) | 62 (30.8) | 158 (9.2) | 20 (16.2) |
| Treatments | |||||
| Aspirin | 281 (14.3) | 262 (14.8) | 47 (23.4) | 242 (14.1) | 36 (29.5) |
| Statins | 553 (28.1) | 482 (27.3) | 73 (36.4) | 479 (27.9) | 42 (34.4) |
| Oral corticosteroids | 75 (3.8) | 69 (3.9) | 6 (3.1) | 59 (3.4) | 8 (6.6) |
CVE: cardiovascular events; N: number; PSI: Pneumonia Severity Index.
Data presented as mean, median (IQ range) or number (%).
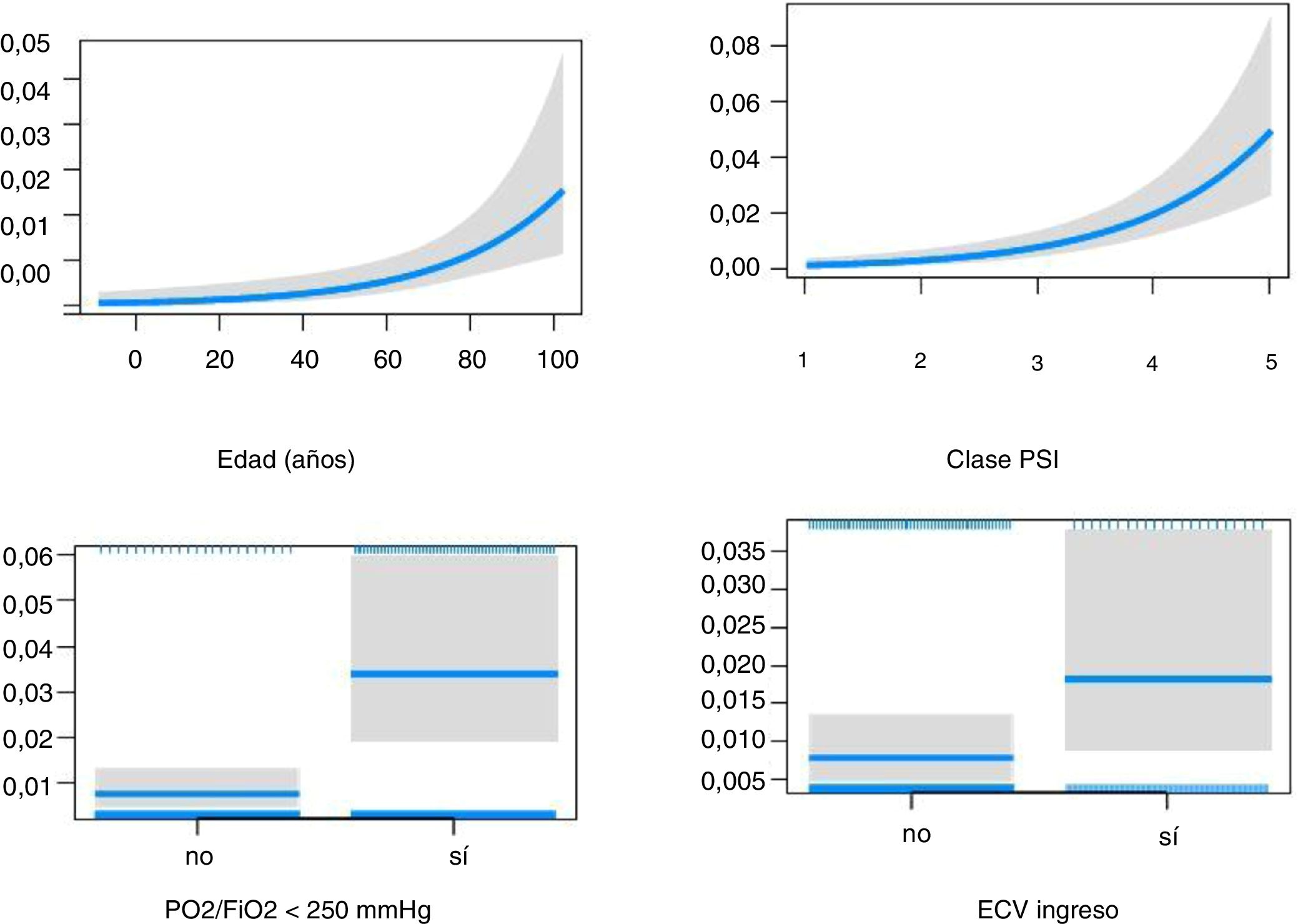
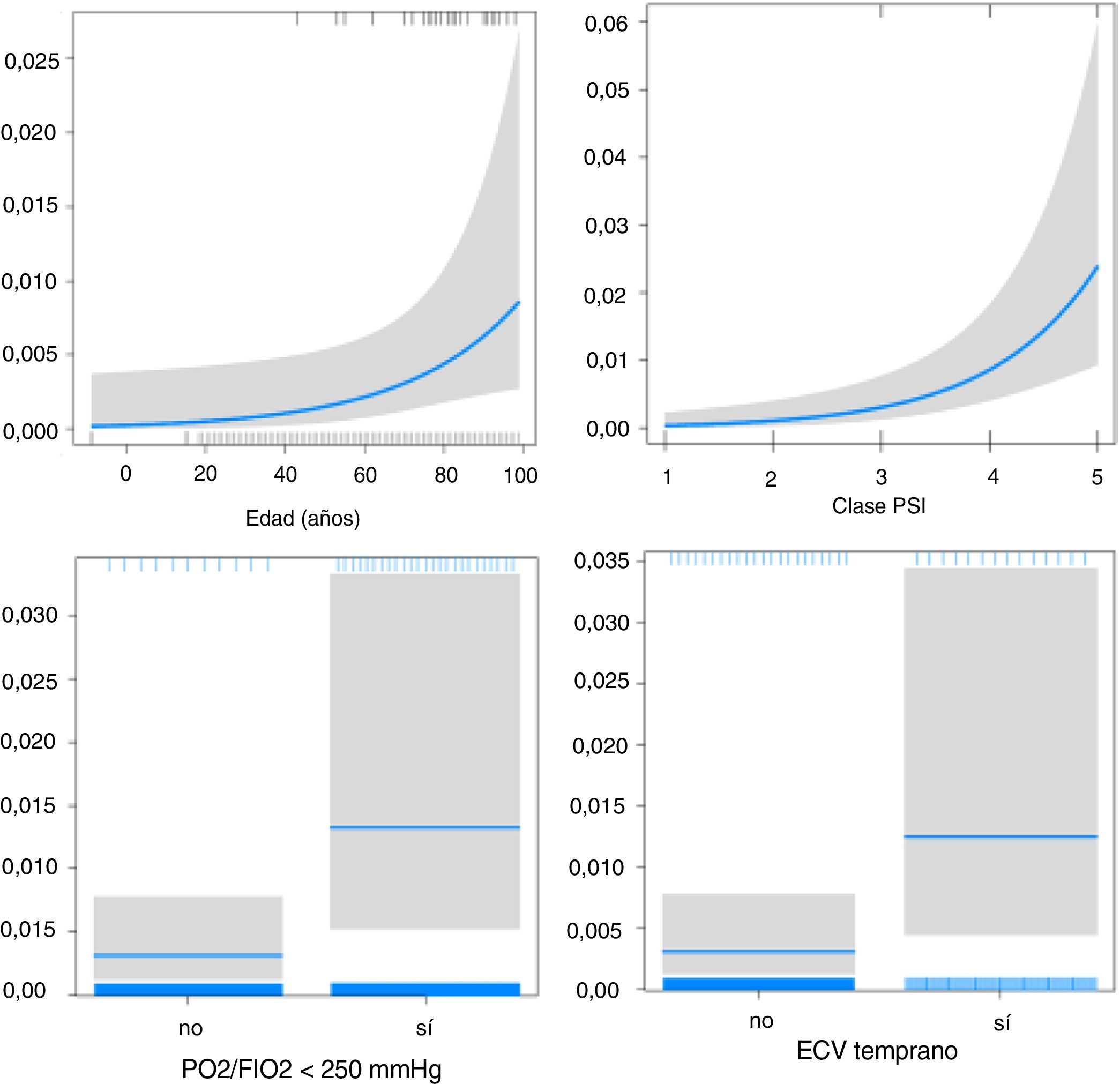
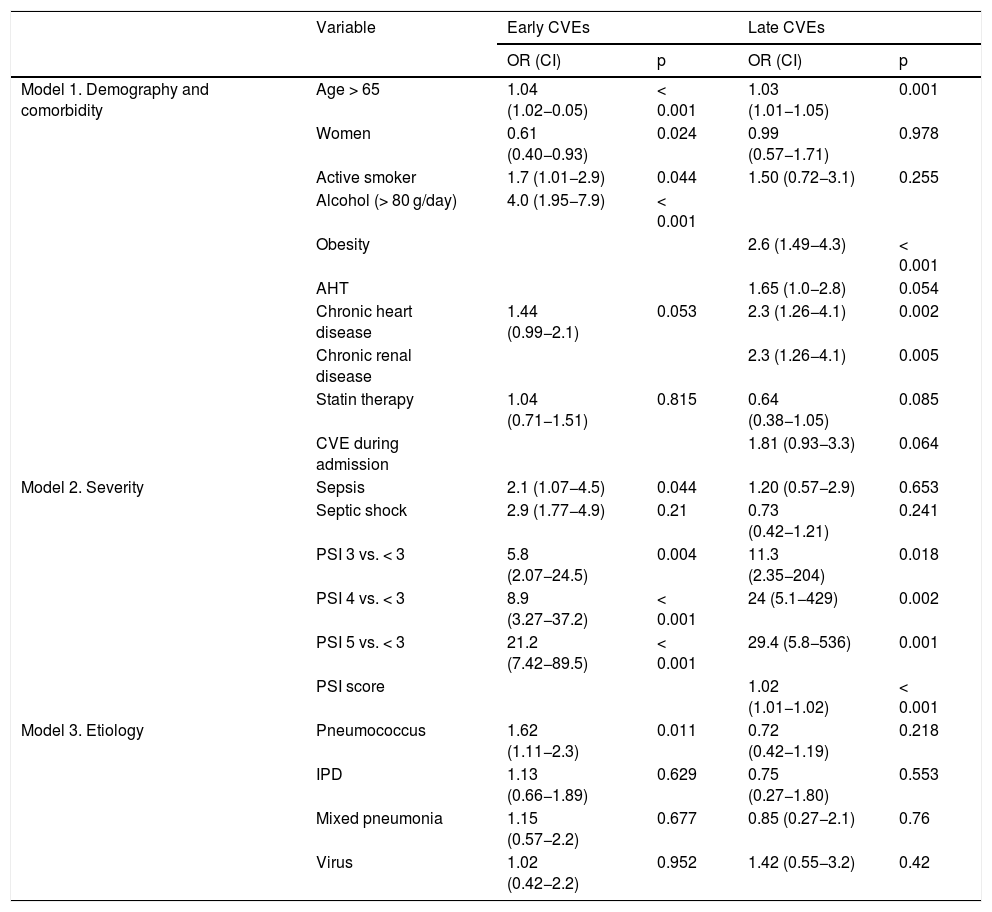
Multivariate study (Table 3). Independent factors associated with early events were: age over 65 years, active smoking, alcohol abuse, history of heart disease, severe sepsis at onset, PSI ≥ 3, and S. pneumoniae infection. Female sex was a protective factor. Factors associated with late events were age over 65 years, obesity, hypertension, history of heart disease, chronic kidney disease, and PSI ≥ 3. Developing an early event was associated with a trend of increased risk of late CVE. No etiology showed an independent effect on late CVE.
Multivariate models for selected variables and early and late cardiovascular events.
| Variable | Early CVEs | Late CVEs | |||
|---|---|---|---|---|---|
| OR (CI) | p | OR (CI) | p | ||
| Model 1. Demography and comorbidity | Age > 65 | 1.04 (1.02−0.05) | < 0.001 | 1.03 (1.01−1.05) | 0.001 |
| Women | 0.61 (0.40−0.93) | 0.024 | 0.99 (0.57−1.71) | 0.978 | |
| Active smoker | 1.7 (1.01−2.9) | 0.044 | 1.50 (0.72−3.1) | 0.255 | |
| Alcohol (> 80 g/day) | 4.0 (1.95−7.9) | < 0.001 | |||
| Obesity | 2.6 (1.49−4.3) | < 0.001 | |||
| AHT | 1.65 (1.0−2.8) | 0.054 | |||
| Chronic heart disease | 1.44 (0.99−2.1) | 0.053 | 2.3 (1.26−4.1) | 0.002 | |
| Chronic renal disease | 2.3 (1.26−4.1) | 0.005 | |||
| Statin therapy | 1.04 (0.71−1.51) | 0.815 | 0.64 (0.38−1.05) | 0.085 | |
| CVE during admission | 1.81 (0.93−3.3) | 0.064 | |||
| Model 2. Severity | Sepsis | 2.1 (1.07−4.5) | 0.044 | 1.20 (0.57−2.9) | 0.653 |
| Septic shock | 2.9 (1.77−4.9) | 0.21 | 0.73 (0.42−1.21) | 0.241 | |
| PSI 3 vs. < 3 | 5.8 (2.07−24.5) | 0.004 | 11.3 (2.35−204) | 0.018 | |
| PSI 4 vs. < 3 | 8.9 (3.27−37.2) | < 0.001 | 24 (5.1−429) | 0.002 | |
| PSI 5 vs. < 3 | 21.2 (7.42−89.5) | < 0.001 | 29.4 (5.8−536) | 0.001 | |
| PSI score | 1.02 (1.01−1.02) | < 0.001 | |||
| Model 3. Etiology | Pneumococcus | 1.62 (1.11−2.3) | 0.011 | 0.72 (0.42−1.19) | 0.218 |
| IPD | 1.13 (0.66−1.89) | 0.629 | 0.75 (0.27−1.80) | 0.553 | |
| Mixed pneumonia | 1.15 (0.57−2.2) | 0.677 | 0.85 (0.27−2.1) | 0.76 | |
| Virus | 1.02 (0.42−2.2) | 0.952 | 1.42 (0.55−3.2) | 0.42 | |
AHT: arterial hypertension; CAP: community-acquired pneumonia; CI: confidence interval; CVA: cerebrovascular accident; CVE: cardiovascular events; IPD: invasive pneumococcal disease; OR: odds ratio; PSI: Pneumonia Severity Index.
Independent variables included. Model 1: age > 65 years, female sex, active smoker, former smoker, alcohol consumption (> 80 g/day), systemic AHT, obesity, diabetes, chronic heart disease, CVA, chronic kidney disease, aspirin treatment, statin therapy, CVE during admission for CAP. Model 2: Sepsis, septic shock, PaO2/FiO2 < 250 mmHg, PSI analyzed as an ordinal quantitative variable (grades 3, 4, and 5 vs < 3) and in addition as a continuous quantitative variable (score) in the late CVE model. Model 3: pneumococcus, IPD, viral etiology and mixed etiology.
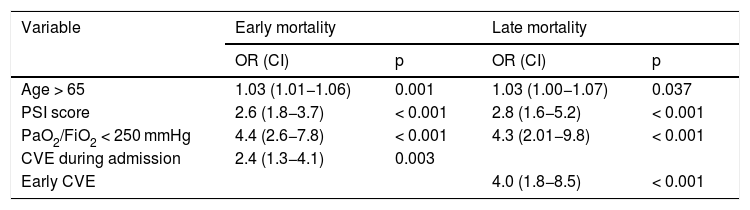
During the study, 198 patients died: 89 during admission, 11 before day 30, and 98 more before 1 year. Thirty-two of the 198 deaths were attributable to CVE, 30% during the initial admission, and 70% in the long-term follow-up. Decompensated heart failure accounted for 50% of mortality due to CVE (16 patients), followed by ischemic stroke (16%, 5 patients), cardiac arrhythmias (16%, 5 patients), acute coronary syndrome (12%, 4 patients), and venous thromboembolic disease (6%, 2 patients).
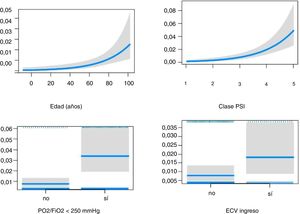
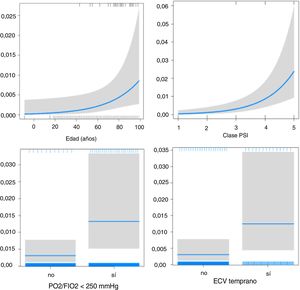
The effect of CVE on early (Fig. 2) and late mortality (Fig. 3) adjusted for age, PaO2/FiO2 < 250 mmHg, and PSI score is shown in Table 4.
Multivariate models for selected variables and early and late mortality.
| Variable | Early mortality | Late mortality | ||
|---|---|---|---|---|
| OR (CI) | p | OR (CI) | p | |
| Age > 65 | 1.03 (1.01−1.06) | 0.001 | 1.03 (1.00−1.07) | 0.037 |
| PSI score | 2.6 (1.8−3.7) | < 0.001 | 2.8 (1.6−5.2) | < 0.001 |
| PaO2/FiO2 < 250 mmHg | 4.4 (2.6−7.8) | < 0.001 | 4.3 (2.01−9.8) | < 0.001 |
| CVE during admission | 2.4 (1.3−4.1) | 0.003 | ||
| Early CVE | 4.0 (1.8−8.5) | < 0.001 | ||
CI: confidence interval; CVE: cardiovascular events; OR: odds ratio; PSI: Pneumonia Severity Index.
Independent variables: age over 65 years, PSI score, PaO2/FiO2 < 250 mmHg, CVE during initial admission for early mortality, and early CVE for late mortality.
The main findings of the study were: 1) early CVE occurred in 10.4% patients, and late CVE in 6.6%; 2) independent factors associated with early events were age over 65 years, active smoking, alcohol abuse, history of heart disease, severe sepsis at onset, PSI ≥ 3, and S. pneumoniae infection. Female sex was associated with a lower risk; 3) factors associated with late events were age over 65 years, obesity, AHT, history of heart disease, chronic kidney disease, PSI ≥ 3, and CVE during admission for pneumonia; 4) early CVE had a negative impact on survival at 30 days and 1 year after the pneumonia episode.
In our study, we found that the risk of developing CVE associated with CAP is high. Some patients with early complications also developed late complications (6.8%), and patients often presented more than 1 complication per episode (20%). Cardiac complications (88% of the total), particularly arrhythmias and heart failure, in the short and long term, such as stroke and/or venous thromboembolic disease, were more common than non-cardiological vascular events. These findings are similar to those obtained by Corrales-Medina et al.,6 although the rates of ischemic heart disease (0.6%) are lower than in the Violi et al. cohort (7.5%)8 in which an active search for silent ischemia was performed.
Preliminary studies in our group have shown that elevated levels of cardiac biomarkers at the time of CAP diagnosis, ventricular stress reflex, myocardial damage, and heart failure17 correlate with the development of short- and long-term CVEs.18 In this study, we have identified factors related with host characteristics, initial severity of pneumonia, and causative microorganism, which independently influence the appearance of CVE. During the acute phase of CAP, advanced age, alcohol abuse, and smoking, widely recognized risk factors for cardiovascular disease, can increase the risk of acute CVE by up to 4-fold. Chronic heart disease was, unsurprisingly, an independent risk factor for the development of CVE, unlike AHT and obesity, which only showed an independent effect on late CVE and chronic kidney disease. Previous treatment with statins, which, due to their immunomodulatory and lipid-lowering effects, have been associated with lower mortality in CAP,19,20 did not protect against the appearance of CVE.
These results show the potential deleterious impact of CAP on patient comorbidity during and after the acute episode. In patients who already have cardiovascular risk factors, an increase in endothelial damage and destabilization of a pre-existing atheroma plaque, persistence of systemic inflammation,21 and hypoxemia could lead to progression of concomitant disease.22,23 Although our findings confirm that comorbidity increases the risk of CVE, it is important to note that 60% of patients who developed early CVE and 45% late CVE had no known history of heart disease. These patients might already have presented subclinical disease and CAP could have played a critical role in its deterioration and aggravation,23 for which reason some authors consider it a cardiovascular risk factor per se.6,24
Severity of CAP presentation is also associated with increased CVE risk, with an odds ratio (OR) that increases progressively with the PSI score.6 During sepsis, which occurs in 40% of hospitalized patients25 and in severe CAP, increased production of inflammatory cytokines and damage10,11,26,27 persist for an unknown period of time. The persistence of a certain degree of inflammation and/or prothrombotic state observed after discharge21,28 may influence the development of late CVE. In our study, the effect of severity measured by PSI achieved a higher OR than severe sepsis on admission for late CVEs. This can be explained because PSI quantifies not only severity, but also age and comorbidity variables of the patient—heart failure and chronic kidney disease—that also increase the likelihood of developing CVE in the long term.
S. pneumoniae was the most frequent etiological agent in the cohort (66%), and in up to 75% of the CVE subgroup. In the 688 patients with pneumococcal CAP, the incidence of CVE was 12.5%, almost twice that of other etiologies, and even higher (17.7%) in patients with IPD. The multivariate study showed that this microorganism has an independent effect when compared with other etiologies. In fact, animal models have shown that S pneumoniae can directly damage the myocardium, causing necrosis and subsequent fibrosis.13 It also has the ability to replicate within macrophages generating a reservoir,29 which if not eradicated can contribute to maintaining a proinflammatory and prothrombotic state, favoring long-term CVE.30
Total mortality during follow-up of the overall cohort was close to 10% (5% at 30 days). This is due to the profile of patients included, of which 10.2% were initially admitted to the ICU, while immunocompromised patients and those with limited therapeutic intervention or a terminal event were excluded. In contrast, total mortality in the CVE subgroup was 22%. This subgroup had twice the early mortality rate and nearly 4 times the late mortality rate compared to patients who did not develop CVE, after adjusting for age and severity. Up to 16% of 1-year mortality was due to a CVE, with the majority occurring between 30 days and 1 year (11%), which corroborates its impact on mortality after discharge.6,26,31
A limitation of the study that should be pointed out is the possible underestimation of CVE after day 30, after which no in-person monitoring was conducted. However, double telephone follow-up and checking of the electronic medical record (both hospital and primary care) were performed. Due to the absence of any systematic virology studies, the possible association of CVE with viral pneumonia, an etiology associated with cardiovascular risk and myocardial damage,32,33 could not be demonstrated.
ConclusionsOur study shows that cardiovascular complications are common among the population hospitalized with CAP, occurring most frequently in the first 30 days. It is also interesting to note the increase in cases of not only ischemic vascular events, but also arrhythmias and heart failure, the main cause of CVE death in our study. Knowing the host-related factors (age, smoking and chronic heart disease) associated with the development of cardiovascular complications, the initial severity of the pneumonia and the causative microorganism (S. pneumoniae), could help in the active screening and early diagnosis of these events. Finally, it is crucial that cardiovascular prevention strategies are implemented during and after the pneumonia episode, and that future intervention studies with treatments to reduce CVE are designed, in order to reduce morbidity and mortality associated with CAP.
FundingThis work has been funded by the Instituto de Salud Carlos III ProjectPI13/00583 (co-funded by European Regional Development Fund/European Social Fund. “Investing in your future”) [PI13/00583] and by the Spanish Society of Pulmonology and Thoracic Surgery [Respiratory Infections PII 166/2013].
Conflict of interestThe authors state that they have no conflict of interests.
The authors would like to thank the NEUMONAC group, Luz Mimbiela, Alexandra Gimeno, Alba Piró and the statistician Antonio José Cañada for their support and dedication to the project.
Pedro Pablo España, Ane Uranga Echeverria (Hospital de Galdakao, Galdakao); Luis Borderías, Elena Briz Muñoz (Hospital San Jorge, Huesca); Olga Rajas (Hospital La Princesa, Madrid); Jordi Almirall, Mari Carmen de la Torre Terron, Ramon Boixeda Viu (Hospital de Mataró, Mataró); Rafael Zalacaín (Hospital de Cruces, Bilbao); Montserrat Vendrell, Montserrat Motjé (Hospital Josep Trueta, Girona); Salvador Bello (Hospital Miguel Servet, Zaragoza); Isabel Mir, Antonio Payeras Cifre (Hospital Son Llàtzer, Palma de Mallorca); Concepción Morales (Hospital Virgen de las Nieves, Granada); Luis Molinos (Hospital Universitario Central de Asturias, Oviedo); Ricard Ferrer (Hospital Mutua Terrasa, Terrasa); M. Luisa Briones (Hospital Clínico Universitario, Valencia); Rosa Malo (Hospital Puerta de Hierro, Majadahonda) Raúl Méndez, Rosario Menéndez, Irene Aldás (Hospital La Fe), Antoni Torres, Rosanel Amaro (Hospital Clínic, Barcelona).
Members of the NEUMONAC Group are listed in Appendix A.
Please cite this article as: Aldás I, Menéndez R, Méndez R, España PP, Almirall J, Boderías L, et al. Eventos cardiovasculares tempranos y tardíos en pacientes ingresados por neumonía adquirida en la comunidad. Arch Bronconeumol. 2020;56:551–558.