We report the case of 72-year-old man, former smoker, with moderate chronic obstructive pulmonary disease (post-bronchodilator FEV1 69%), and previous left pneumonectomy for squamous cell lung cancer with invasion of the pulmonary artery.
He presented in the emergency department of our hospital 2 months post-surgery with progressively worsening dyspnea, even on minimal exertion, aggravated in a sitting or upright posture.
Clinical signs included tachypnea, oxygen saturation (SatO2) 88%, d-dimer 1226ng/ml, and arterial blood gases pH 7.42, pO2 65.1mmHg, pCO2 31.2mmHg and HCO3 20.1mmol/l. Post-surgical changes were seen on chest X-ray, and no signs of pulmonary embolism were found on lung scintigraphy/SPECT-CT.
In view of the patient's history of lung surgery and oxygen desaturation in an upright posture, platypnea–orthodeoxia syndrome (POS) was suspected.
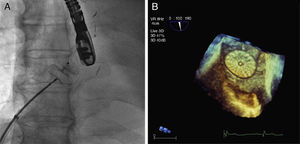
SatO2 was tested in supine and sitting positions, showing a significant fall in hypoxemia in an upright posture (from 93% to 88% with nasal cannulas at 4l/min). Transthoracic echocardiography (TTE) with bubble study revealed a right-to-left shunt due to a patent foramen ovale (PFO). These findings were confirmed by transesophageal echocardiography (TEE).
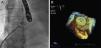
The patient underwent heart surgery for percutaneous closure of the PFO, using the Amplatzer® Cribriform occluder (Fig. 1). Successful placement of the device and absence of residual shunt was confirmed with TEE. In subsequent follow-ups, the patient's dyspnea was fully resolved and standing SatO2 was normal.
POS is an unusual phenomenon, consisting of dyspnea in an upright posture, which diminishes in recumbency (platypnea), accompanied by increased blood oxygen levels in that posture (orthodeoxia).
Causes of POS can be divided into 3 groups, depending on the pathogenesis: cardiac, pulmonary or other.1–3
Two components are required in cardiac POS, one being anatomical (common in all patients) and the other functional. The anatomical component must involve an intracardiac communication causing shunt. The most common defect in the general population and in POS patients is PFO. PFO does not generally cause disease because it causes left-to-right shunt, but this reverses in the presence of certain functional changes.
The most common functional components include ascending aorta aneurysm, pneumonectomies (most often right-sided) and lobectomies, pericardial and myocardial disease, and tricuspid valve disease. The reduction in blood flow experienced in recumbency causes the shunt to diminish, with the consequent rise in SatO2.
A high level of suspicion is needed in the diagnosis of POS, and a careful anamnesis is essential if it is to be identified.
The most simple, but no less important, examination is the determination of SatO2 in different postures. Definitive diagnosis of cardiac POS is reached with bubble-contrast TEE, which produces fewer false-positives than TTE. Both tests may be normal when the patient is supine, or if microbubble contrast medium is administered via an upper limb. This is because in PFO, the flow is received primarily by the inferior vena cava.4
Cardiac POS treatment consists of closing the PFO with Amplatzer® devices, resulting in resolution of symptoms5 and normal SatO2 in an upright posture.
Please cite this article as: Galván OP, Garcia-Olivé I, Prats MS, Sistach EF, Fernández-Nofrerias E, Manzano JR. Disnea en paciente neumonectomizado. Arch Bronconeumol. 2015;51:524–525.