Linear endobronchial ultrasound (EBUS) allows samples of lesions close to the airways to be obtained, as it enables aspiration to be performed under visual control in real time, opening new possibilities for minimally invasive examination of the mediastinum. While there are many publications on its usefulness in the study of mediastinal or hilar lymphadenopathies, there are few that analyse the role of EBUS-guided transbronchial needle aspiration for the diagnosis of other lesions adjacent to the airways or digestive tract. We describe the characteristics and results obtained in a series of 26 cases of non-nodal lesions of different aetiologies studied by EBUS-guided transbronchial needle aspiration through the airways or oesophagus, demonstrating the usefulness and safety of this technique in the diagnosis of these types of lesions.
La ultrasonografía endobronquial lineal (USEB) facilita la obtención de muestras de lesiones próximas a la vía aérea, ya que permite realizar la punción bajo control visual en tiempo real, abriendo nuevas posibilidades de exploración mínimamente invasiva del mediastino. Mientras que existen multitud de publicaciones acerca de su utilidad en el estudio de adenopatías mediastínicas o hiliares, son escasas aquellas que analizan el papel de la punción guiada por USEB para el diagnóstico de otras lesiones adyacentes a la vía área o digestiva. Describimos las características y los resultados obtenidos en una serie de 26 casos de lesiones no adenopáticas de diferentes etiologías estudiadas mediante punción guiada por USEB a través de la vía aérea o esofágica, demostrando la utilidad y seguridad de esta técnica en el diagnóstico de este tipo de lesiones.
Linear endobronchial ultrasound (EBUS) allows the non-invasive and safe sampling of any type of lesion close to the airways and digestive tract, as it enables needle aspiration to be performed under visual control in real time (EBUS-TBNA).1 The most widely-accepted indications for EBUS-TBNA are the diagnosis, staging and restaging of lung carcinoma from mediastinal lymph node samples, although its application in the study of other diseases such as lymphomas, and granulomatous diseases like sarcoidosis and tuberculosis, has also been described.1 However, little evidence is available on the usefulness and safety of EBUS-TBNA in the diagnosis of other types of lung and mediastinal lesions adjacent to the airways or oesophagus.2,3
Clinical Observation (Case Series)Forty-three (43) lesions of possible non-nodal origin were selected from a database of 730 different lesions aspirated by EBUS-TBNA in 450 patients. After a comprehensive review of the imaging studies and cytopathological findings, 26 cases in which the authors were completely sure that the aspirated lesion was non-nodal were included in this analysis. The other 17 lesions were hilar or paratracheal masses from which, although suitable material was obtained for the diagnosis of malignancy in all cases, with no histological data to suggest that a lymph gland had been aspirated, there was some possibility, due their location, that they could have initially originated from metastatic hilar or paratracheal lymph node involvement.
The procedures were performed by four bronchoscopists in an outpatient setting, with conscious sedation with midozalam and fentanyl. The samples were examined immediately by a pathologist. An Olympus UC180F endobronchial ultrasound scope and an Aloka Alpha 5 ultrasound system were used. All patients signed an informed consent form.
The mean age of the 26 patients was 62 (SD, 12) years and 18 (69%) were male. None had endobronchial lesions. In 8 (30.8%) of the cases, the lesion was exclusively intrapulmonary, in 16 (65.4%) the lesions were pulmonary with mediastinal contact or infiltration and another 2 (7.6%) cases were paraesophageal lesions. All were less than 10mm from the airways or oesophagus; the mean diameter was 31 (SD, 16) mm, the most common location was the right upper lobe (61.5%), the mean SUV on PET-CT was 11.9 (SD, 4.2) and 2 (SD, 0.9) passes were made each time. In 3 cases, access was via the oesophagus and samples were obtained satisfactorily in all 3 cases.
Suitable material was obtained from 25 (96.1%) lesions. Of these, 16 (61.5%) were pulmonary adenocarcinomas and 6 (23.7%) other subtypes, 2 (7.6%) were extrapulmonary carcinomas, 1 (3.8%) a tubercular lesion and 1 (3.8%) a pneumonic process. In the case of one patient with pulmonary adenocarcinoma, insufficient material was obtained for a specific diagnosis and it was confirmed by surgery.
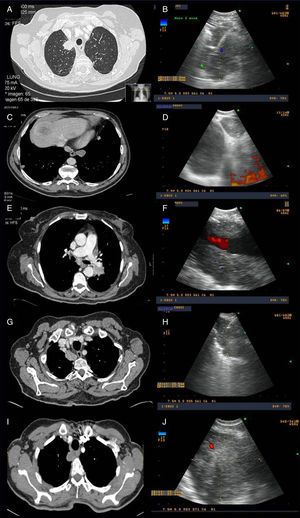
Fig. 1 shows some examples of the computed tomography (CT) and endoscopic ultrasound images obtained.
Examples of radiological and ultrasound images from four of the cases from the series. (A and B) Computed tomography (CT) and endoscopic ultrasound images of a mass located in the right upper lobe, aspirated using endobronchial ultrasound, the result of which was adenocarcinoma of pulmonary origin. (C and D) CT and endoscopic ultrasound images of a patient with a pulmonary lesion in the left lower lobe and lymphadenopathy in right mediastinal station 9. Both were aspirated using endobronchial ultrasound via the oesophagus; the result in both was colon cancer metastasis. (E and F) CT and endoscopic ultrasound images of a left hilar mass surrounding the pulmonary artery, with EBUS-guided needle aspiration diagnostic of adenocarcinoma of pulmonary origin. (G and H) CT and endoscopic ultrasound images of a right paratracheoesophageal mass possibly originating in the right upper lobe, with needle aspiration carried out via the oesophagus, resulting in a diagnosis of adenocarcinoma of pulmonary origin. (I and J) CT and endoscopic ultrasound images of a mass located in the right upper lobe infiltrating the mediastinum. EBUS-guided fine needle aspiration was performed with a result of adenocarcinoma of pulmonary origin.
No complications related with the procedures were described.
DiscussionThe diagnosis of paramediastinal or central pulmonary lesions with no endobronchial lesion is a clinical problem, since conventional diagnostic techniques are not very effective for obtaining a cytohistological diagnosis, and the results depend in large part on the size of the lesions, presence or absence of the bronchus sign and the availability of new technologies.4 For lesions closer to the central airways or the digestive tract, one possible option is the use of EBUS, a technique that has been widely validated in the study of mediastinal lymphadenopathies, although there is little published evidence in these types of lesions and few series address this indication exclusively.2,3,5 In the study by Tournoy et al.,2 all the lesions were intrapulmonary and of malignant aetiology, while in the report published by Yang et al.,3 as in ours, lesions adjacent to the airways, whether intrapulmonary or mediastinal, and of benign aetiology (such as tuberculosis and mediastinal cysts) were also included. We found only one series published in Spain in the form of an abstract.5
The review of these cases confirms the value and safety of EBUS-TBNA in both the respiratory tract and the oesophagus in the diagnosis of non-endobronchial central lesions of different aetiologies. One possible limitation of this study is that we could not clearly define if a central or paratracheal lesion was of nodal origin or if it was a lung lesion that had extended beyond the bronchi or towards the mediastinum. This was the situation encountered in 17 of the 43 cases initially selected, and the reason for excluding them from the analysis, even though a diagnosis of malignancy could be made by EBUS-TBNA in all cases. This serves to further reinforce the usefulness of this technique in these types of lesions.
Please cite this article as: Lourido T, et al. Diagnóstico de lesiones paratraqueobronquiales no adenopáticas mediante ecobronquial lineal. Actas Dermosifiliogr. 2013;49:337–9