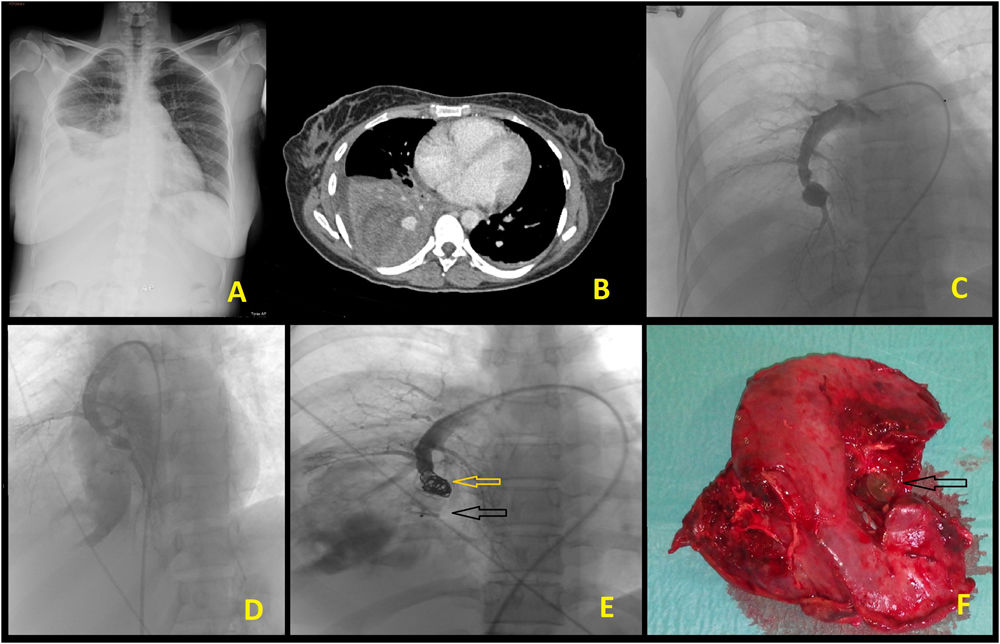
We report the case of a 29-year-old patient who attended the emergency department due to generalized deterioration, dyspnea, fever of up to 38 °C, and right rib pain. She had recently been diagnosed with type I diabetes mellitus, with onset of an episode of ketoacidosis 1 week earlier. Clinical laboratory tests were significant for severe leukocytosis and hyperglycemia1. Right lower lobe (RLL) pneumonia was identified (Fig. 1A) and the patient was hospitalized. The patient’s clinical progress was slow and she had an episode of self-limiting hemoptysis. Bronchoscopy was performed and a biopsy was obtained, identifying the presence of Mucor fungal hyphae. A contrast-enhanced chest computed tomography (CT) scan (Fig. 1B) revealed findings consistent with necrotizing pneumonia, increased pleural effusion, and a saccular lesion measuring 14 mm associated with a mucormycotic pseudoaneurysm of the lower medial segmental branch of the RLL.
A) Chest AP Rx showing alveolar infiltrate in RLL containing some radiolucent areas associated with pleural effusion. B) Contrast-enhanced chest CT (mediastinal window). Pulmonary parenchymal consolidation with enhanced thick-walled hypodense collection associated with a 6 cm abscess (necrotizing pneumonia) and pleural effusion. Saccular lesion, measuring 14 mm, associated with mucormycotic pseudoaneurysm. C) Diagnostic-therapeutic arteriography. Saccular lesion associated with pseudoaneurysm in the lower branch of the medial segment of the RLL. D) Pseudoaneurysm appearing smaller than in Figure C, showing contrast extravasation associated with the rupture. E) Embolization by Amplatzer device (black arrow) and placement of coils (yellow arrow) in the arterial branch of the lower medial segment of the RLL. F) Surgical piece after right lower lobectomy, showing necrotic cavity and Amplatzer device (arrow).
AP: anteroposterior; RLL: right lower lobe; Rx: X-ray; CT: computed tomography.
In view of these findings, therapeutic arteriography (Fig. 1C) with selective catheterization of the lesion was performed, causing it to rupture (Fig. 1D). The patient began to produce frank hemoptysis that required urgent embolization with a 14 mm Amplatzer II device and the placement of 10 mm coils and an 8 mm Amplatzer in the lower medial segmental branch of the RLL.
Following clinical stabilization with targeted treatment (amphotericin liposomal and capsofungin), a right lower lobectomy was performed in a second procedure (Fig. 1F) with no further complications.
FundingThis paper has not received any funding.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: García Gallardo MdM, Berma Gascón ML. Diagnóstico y tratamiento urgente de la ruptura de un pseudoaneurisma mucormicótico pulmonar. Arch Bronconeumol. 2022;58:85.