Adrenocortical carcinoma is an extremely rare tumor. Around 0.5–2 cases per million inhabitants are diagnosed per year.1 Presentation varies from asymptomatic forms to manifestations of hormonal hyperfunction, especially hypercortisolism and androgenization. These tumors are very aggressive, and prognosis is poor, even after surgery. Diagnosis is obtained by imaging tests and confirmed by pathology analysis of the surgical specimen. However, surgery is not always possible, so reaching a definitive diagnosis can be complex. We report the case of an adrenocortical carcinoma with liver and lung extensions that was diagnosed by flexible bronchoscopy.
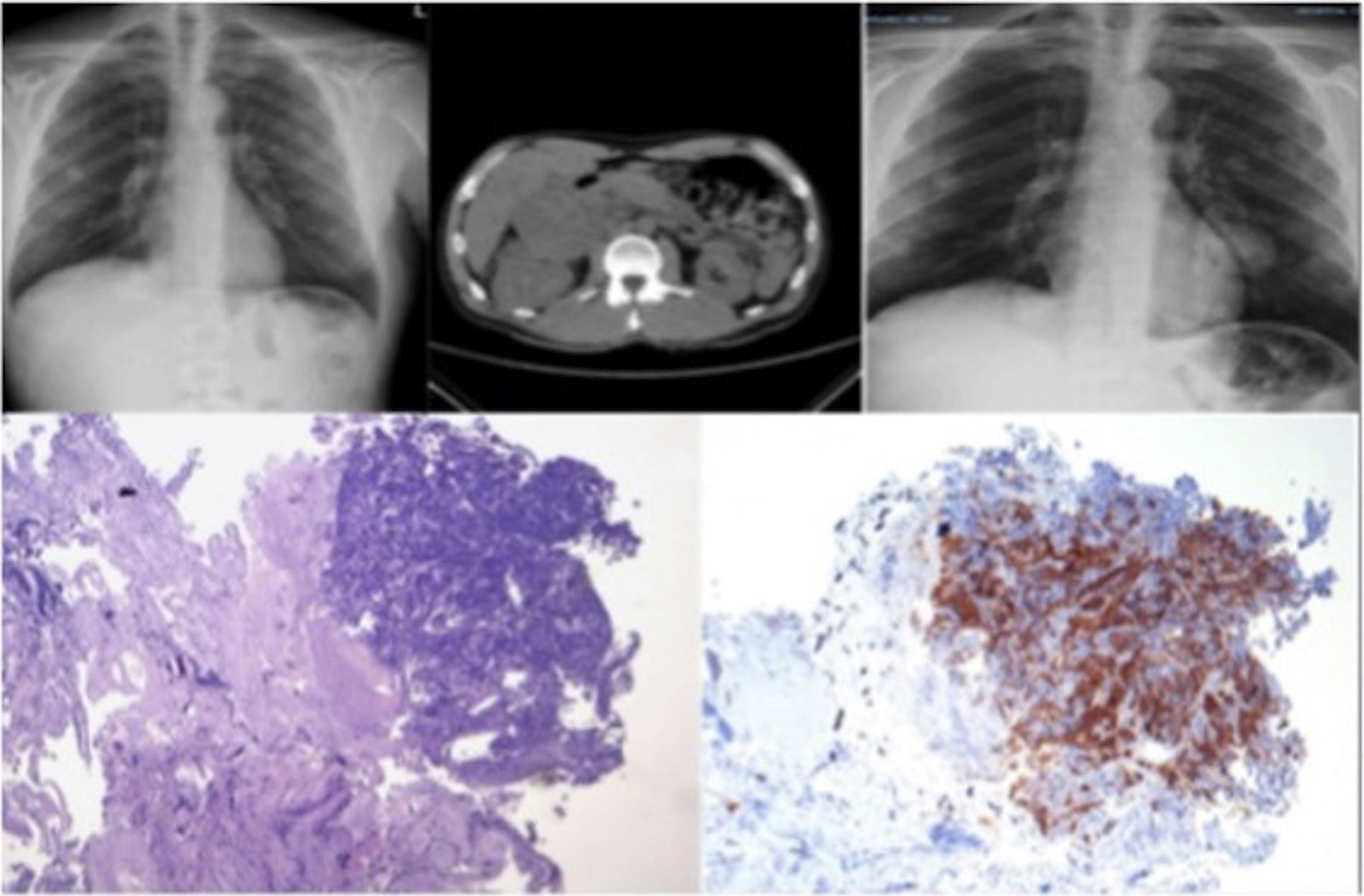
Our patient was a 54-year-old man with no significant history or toxic habits, who attended the emergency room for a 3-day history of chest pain radiating to the back, accompanied by 38.5°C fever, dyspnea on moderate exertion, cough with purulent expectoration, and hemoptysis. He had no chest pain or palpitations. He reported asthenia and anorexia in the last 6 months, with a 10kg weight loss. Physical examination was unremarkable, and vital signs were normal, with the exception of fever. Clinical laboratory test results were all normal, except for C-reactive protein, which was high. Multiple pulmonary nodules were observed on chest X-ray (Fig. 1), so the patient was admitted to the respiratory medicine ward.
During admission, a computed tomography was performed, which revealed a right peritoneal mass of heterogeneous density measuring 13cm×11cm (Fig. 1), impinging on the right kidney and the right hepatic lobe, containing punctiform calcifications. The right adrenal gland could not be visualized. Multiple disperse, rounded, dense pulmonary nodules were detected in both lung fields, consistent with metastases. No mediastinal or axillary lymphadenopathies were observed. A rounded hypodense lesion was seen in liver segment V–VI, consistent with metastases.
Given the findings consistent with adrenocortical carcinoma, an examination of the adrenal axis and meta-iodobenzylguanidine scintigraphy were requested to rule out pheochromocytoma, since biopsy of the lesion in these cases may be fatal. As this isotope is not used in our hospital, the scintigraphy would have been deferred 1 week, so to avoid delay in diagnosis, we decided to perform a fine-needle aspiration of the liver.
Pathology report results were negative for neoplastic cells, so a bronchoscopy was scheduled. In the chest X-ray conducted before this examination, the pulmonary nodules were seen to have grown significantly (Fig. 1). Bronchoscopy revealed a mass with a necrotized surface and soft consistency in the wall of the posterior segment of the left lower lobe (B10), with partial stenosis of the bronchus. Brushing was performed and a biopsy was obtained, and selected bronchial material was aspirated. The endoscopic judgment was direct signs of neoplasia in the left B10, and the pathology results from the endobronchial biopsy gave a diagnosis of primary carcinoma in the adrenal cortex, with the following immunohistochemical features: inhibin positive, and CK7, TTF-1 and napsin negative (Fig. 1).
Adrenocortical carcinoma is a rare, highly aggressive malignant neoplasm, with poor 5-year survival rates, ranging from 15% to 44% in the published series.2,3 Even after radical resection, most patients develop local recurrence or de novo metastasis.4 Although it is more often sporadic, it may be associated with familial susceptibility.5,6
Metastasis occurs via the lymphatic system and the bloodstream, and by implantation in nearby sites. It has been reported that 21%–39% of all patients have distant metastases at the time of diagnosis.7 Adrenocortical carcinoma usually metastasizes to the lung, the liver, the peritoneum and pleura, the lymph nodes, and the bones.8 Disease progression is rapid, and this entity is a challenge, in terms of both diagnosis and early treatment. The rapid progression of our patient can be observed in the series of radiological images of the chest (Fig. 1).
Radiological assessment of tumor extension is essential and helps to establish the surgical approach. Complete surgical resection is the only curative option when the disease is localized. Patients should undergo surgery in an experienced reference center.9 In our patient, the extension of the lesions ruled out resection, and palliative oncological care was administered.
Since cases of adrenocortical carcinoma are extremely rare, and surgery is not always an option for diagnostic confirmation, we consider this case exceptional, as the diagnosis was established by bronchoscopy. The possibility of rare cancers must be considered in the differential diagnosis of pulmonary lesions.
Our thanks to the Respiratory Medicine Department of the Hospital Universitario Virgen de la Victoria.
Please cite this article as: Cabrera César E, Fernández Aguirre MdC, Reina Marfil N, Velasco Garrido JL. Diagnóstico de carcinoma suprarrenal por broncoscopia flexible. Arch Bronconeumol. 2018;54:171–172.