Continuous positive airway pressure (CPAP) is one of the most common therapies for Obstructive Sleep Apnea (OSA). We present a brief, patient-reported outcome measure used to assess patients’ levels of adherence with CPAP treatment.
MethodsA questionnaire was developed based on academic literature. We qualitatively tested a pool of 18 items. It was tested in a sample of 174 patients from the Hospital La Princesa. Next, 1021 patients from Catalonia were evaluated.
Results5 items were removed. Nominal groups referred to three areas: general knowledge about OSA and its risks; CPAP treatment information and expectations; CPAP use, monitoring, and confidence with its use. The 13 retained items maintained the same meaning as the original questionnaire (r=.986; p<.001) and the three proposed dimensions detected a significant increase in general knowledge of OSA (t[173]=8.097, p<.001); CPAP treatment information (t[173]=15.170, p<.001); and CPAP use (t[173]=14.642, p<.001). The final 12-item version was reliable (CRI=.793) and its internal structure was adequate (χ2[51]=72.073; p=.027, CFI=.967, RMSEA=.020 [.000, .030]). Women had a better general knowledge of OSA (t[1,018]=2.190, p=.029), CPAP treatment information (t[1,018]=2.920, p=.004), and higher overall OSA-CPAP scores (t[1,018]=3.093, p=.002). Scores were positively related to quality of life and motivation, adherence was positively related to CPAP use and monitoring, and the total score was negatively related to daytime sleepiness.
ConclusionsThe interview could help clinicians prevent some dropouts by targeting patients with lower adherence. It's a tool for assessing patient adherence to CPAP and to promote strategies through education and external motivational stimuli.
La presión positiva continua en la vía aérea (CPAP) es uno de los tratamientos más frecuentes para la apnea obstructiva del sueño (AOS). Presentamos una breve medida de resultados percibidos por el paciente para evaluar los niveles de adhesión de los pacientes al tratamiento con CPAP.
MétodosSe desarrolló un cuestionario basado en la literatura académica. Se ensayó cualitativamente un conjunto de 18 ítems en una muestra de 174 pacientes del Hospital La Princesa (Madrid). A continuación se evaluaron 1.021 pacientes de Cataluña.
ResultadosSe eliminaron 5 ítems. Los grupos nominales se refirieron a tres áreas: conocimiento general sobre la AOS y sus riesgos; información y expectativas de tratamiento con CPAP; uso de la CPAP, seguimiento y desenvoltura en su manejo. Los 13 ítems conservados mantuvieron el mismo significado que el cuestionario original (r=0,986; p<0,001) y las tres dimensiones propuestas detectaron un aumento significativo en el conocimiento general de la AOS (t[173]=8,097, p<0,001); información sobre el tratamiento con CPAP (t[173]=15,170, p<0,001); y uso de la CPAP (t[173]=14,642, p<0,001). La versión final de 12 ítems fue fiable (CRI=0,793) y su estructura interna fue adecuada (χ2 [51]=72,073; p=0,027, CFI=0,967, RMSEA=0,020 [0,000, 0,030]). Las mujeres mostraron mejor conocimiento general de la AOS (t[1,018]=2,190, p=0,029), de la información sobre el tratamiento con CPAP (t[1,018]=2,920, p=0,004), y obtuvieron mejores puntuaciones globales en la entrevista OSA-CPAP (t[1,018]=3,093, p=0,002). Las puntuaciones se relacionaron positivamente con la calidad de vida y la motivación, la adhesión se relacionó positivamente con el uso y el seguimiento con CPAP, y la puntuación total se relacionó negativamente con la somnolencia diurna.
ConclusionesLa entrevista podría ayudar a los médicos a prevenir algunos abandonos del tratamiento al indicar aquellos pacientes con menor adhesión. Es una herramienta para evaluar la adhesión del paciente a la CPAP y para promover estrategias a través de la educación y estímulos motivacionales externos.
Obstructive sleep apnoea-hypopnea syndrome (OSA) is a disorder characterised by repeated breathing interruptions because of upper airway obstruction. The prevalence of OSA in the general population varies significantly according to variations in diagnostic criteria,1 and it is associated with sleep fragmentation with consequent daytime drowsiness and increased cardiovascular risk, metabolic disturbances, traffic accidents, and use of healthcare resources.2 Continuous positive airway pressure (CPAP) is one of the most commonly used therapies for OSA. CPAP therapy reduces daytime drowsiness, improves cognitive performance, and decreases sympathetic activation, blood pressure, and mortality. However, these results depend on adequate adherence (hours of CPAP use per day) to the treatment.3–6 The use of CPAP for 6–8h per night is recommended and indeed, a common clinical and empirical benchmark of a mean 4h per night for 70% of the night has been defined for CPAP use.7
Nonetheless, 5–50% of patients discontinue CPAP treatment during the first week and 12–25% will have stopped its use after 3 years, and globally, approximately 45% of patients become non-adherent to CPAP treatment.8 When patients become non-adherent, the treatment has no effect9,6 and so it is very important to identify the factors that influence CPAP use.8,10,11 Understanding the factors that can predict CPAP treatment adherence could allow interventions to be adapted to help to ensure good patient follow-ups and thus, improve their quality of life. However, even though several groups have sought to define the profile of compliant patients, there is wide variation in these results and the set of factors related to adherence has not yet been clearly defined.
Many factors that might be related to greater adherence including age, sex, marital and socioeconomic status, disease severity, adverse effects, snoring, Epworth test scores, BMI, and treatment initiation method, have been assessed.12,13 However, from among all of these, patient perception of their symptoms and improvements in drowsiness and activity levels upon commencing CPAP treatment seem to be the most important factors. Similar to treatment adherence,11 health beliefs and behaviours (about the illness, treatment efficacy, and constraints), self-efficacy (confidence to engage in a treatment), and perceived competence (belief in one's ability to effectively interact with the environment),14,15 explain more than 30% of the variance in CPAP use.16
Psychological variables, including the health value, health locus of control, and self-efficacy were investigated by Wild et al.17; the former reflects the importance of physical activity to individuals; the locus of control scale measures health-related beliefs in three dimensions: internality (the patient's perception of the extent to which their health is within their own control), chance (patient's external control of their health outcomes), and powerful others (the belief that others have control)17,18; finally, self-efficacy measures the person's belief in their own ability to accomplish a task.17 This study observed a positive association between CPAP adherence and internal locus of control scores, perhaps because patients who believe they have control over their own circumstances are more likely to internalise advice provided their physician, reflected as better adherence to CPAP, despite its inconveniences.17 Some studies have been carried out to evaluate aspects of self-efficacy in relation to the use of CPAP. The Self-Efficacy Measure for Sleep Apnoea (SEMSA)19 is a 26-item self-administered questionnaire comprising three factors: the risk perception of obstructive sleep apnoea syndrome, benefit of CPAP, and self-efficacy (confidence to engage in CPAP use). It is a disease-specific measure of adult OSA patient pre-treatment expectations for CPAP and is designed to assess adherence-related cognitions. Different groups have obtained varying validation results for the SEMSA questionnaire, which may be because of cultural diversity.20–26 The explanatory capacity of self-efficacy cannot be applied to the general population because of the high disease variability and higher prevalence of OSA in women
CPAP use and adherence has also been related to motivation. Patients who are motivated to resolve their health problems tended to adhere better to CPAP treatment than those who worried less about their health.27
Perceived competence is usually understood as the general belief about being able to interact with the environment effectively (having competences or aptitudes). It is compose by both an expectation of self-efficacy and an expectation of good results in performing a certain behavior.28 When patients are enrolled in CPAP treatment, a feeling of responsibility for following therapy can lead to continuing treatment beyond of what is easily observable or rewarded, that is rather an intrinsic motivation.
Considering the available evidence for certain factors that influence CPAP treatment adherence, we aimed to present a brief, patient-reported outcome measure to assess patient perceived competence with CPAP therapy which included factors that could be used both to predict and follow-up this adherence. This instrument would allow healthcare professionals to implement strategies that increase patient adherence, thus helping to reduce the symptoms and comorbidities associated with OSA, as well as traffic accidents, mortality, and health expenditure associated with this disease.
Material and methodsThe evaluation protocol was approved by the ethics committee (CEICm) at the Hospital Universitario La Princesa (Registration No. 3450/18).
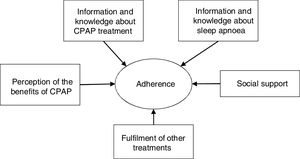
Questionnaire developmentThe OSA-CPAP Perceived Competence Evaluation Interview is an instrument for measuring the perceived competence of patients with OSA to CPAP treatment and was designed to quantify this data and make it universal. According to our bibliographic review, the construct of adherence was defined as patient number of hours use of CPAP per day and their knowledge of their disease and the benefits of follow-up,29 with social support and the patient's general ability to follow treatments being protective factors. We based the OSA-CPAP Perceived Competence Evaluation Interview on the perceived competence perspective, the Transtheoretical Model of Change30 and Motivational Interview paradigms,29 and so it included specific motivation items. The questionnaire included areas corresponding to the education module, itself derived from the work of Olsen et al.,29 including:
- •
Information and knowledge about sleep apnoea: 6 items.
- •
Information and knowledge about CPAP treatment: 9 items.
- •
Perception of the benefits of CPAP therapy: 1 item.
- •
Fulfilment of other treatments: 1 item.
- •
Social support: 1 item.
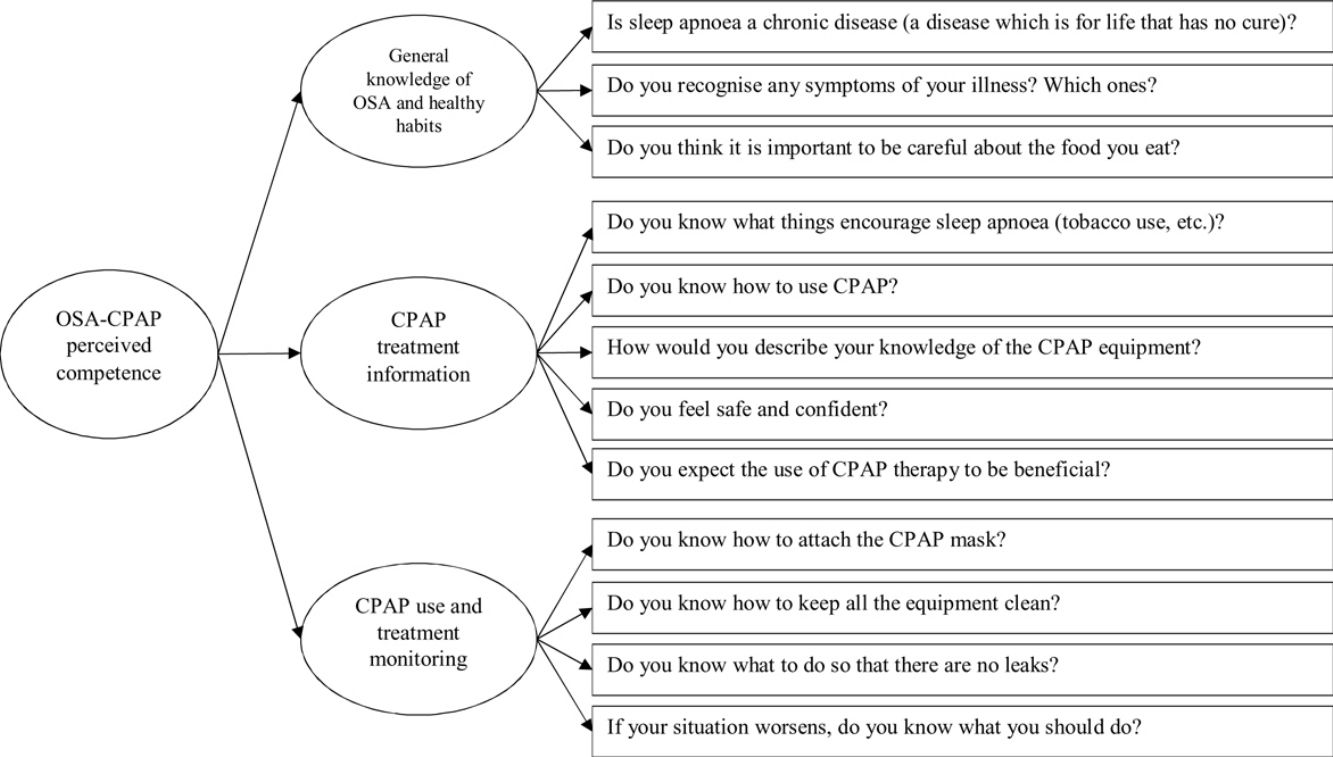
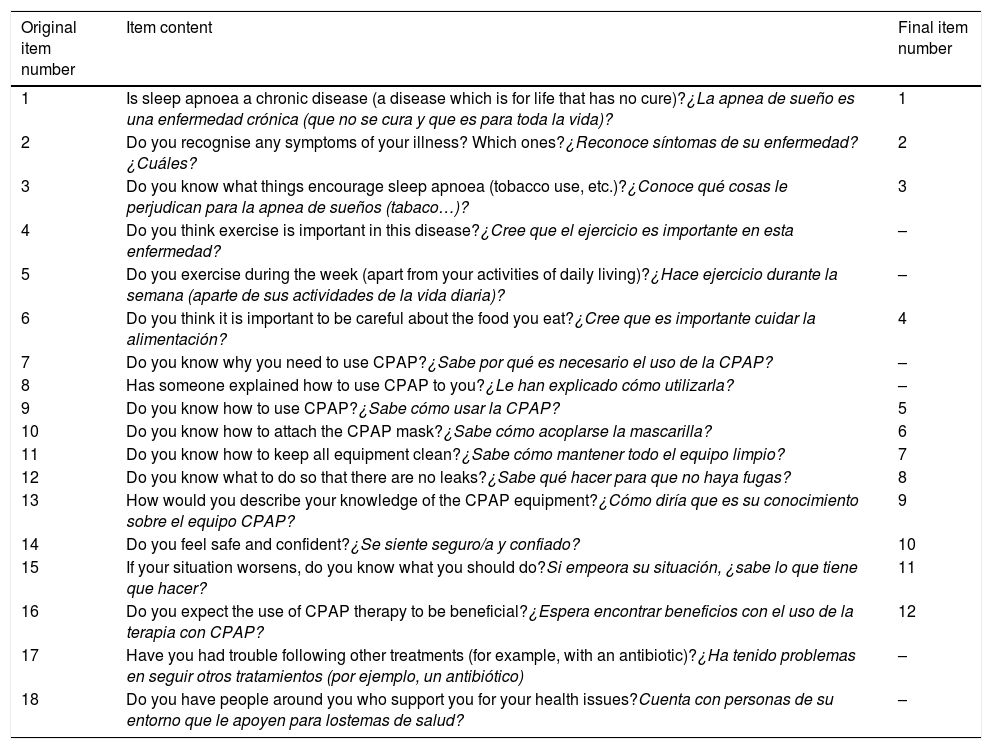
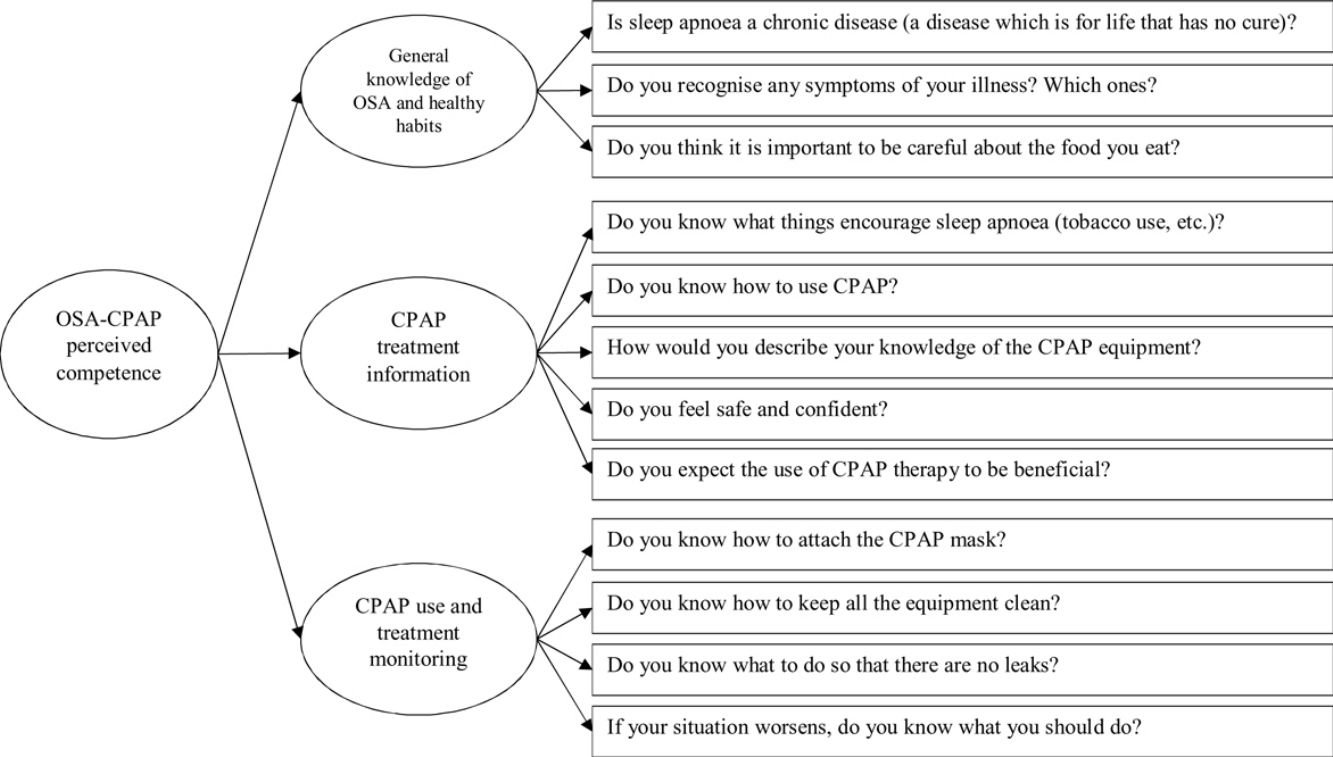
The items included in the questionnaire are shown in Table 1 and the theoretical model of the questionnaire is represented in Fig. 1.
Items used in the development of the questionnaire.
| Original item number | Item content | Final item number |
|---|---|---|
| 1 | Is sleep apnoea a chronic disease (a disease which is for life that has no cure)?¿La apnea de sueño es una enfermedad crónica (que no se cura y que es para toda la vida)? | 1 |
| 2 | Do you recognise any symptoms of your illness? Which ones?¿Reconoce síntomas de su enfermedad? ¿Cuáles? | 2 |
| 3 | Do you know what things encourage sleep apnoea (tobacco use, etc.)?¿Conoce qué cosas le perjudican para la apnea de sueños (tabaco…)? | 3 |
| 4 | Do you think exercise is important in this disease?¿Cree que el ejercicio es importante en esta enfermedad? | – |
| 5 | Do you exercise during the week (apart from your activities of daily living)?¿Hace ejercicio durante la semana (aparte de sus actividades de la vida diaria)? | – |
| 6 | Do you think it is important to be careful about the food you eat?¿Cree que es importante cuidar la alimentación? | 4 |
| 7 | Do you know why you need to use CPAP?¿Sabe por qué es necesario el uso de la CPAP? | – |
| 8 | Has someone explained how to use CPAP to you?¿Le han explicado cómo utilizarla? | – |
| 9 | Do you know how to use CPAP?¿Sabe cómo usar la CPAP? | 5 |
| 10 | Do you know how to attach the CPAP mask?¿Sabe cómo acoplarse la mascarilla? | 6 |
| 11 | Do you know how to keep all equipment clean?¿Sabe cómo mantener todo el equipo limpio? | 7 |
| 12 | Do you know what to do so that there are no leaks?¿Sabe qué hacer para que no haya fugas? | 8 |
| 13 | How would you describe your knowledge of the CPAP equipment?¿Cómo diría que es su conocimiento sobre el equipo CPAP? | 9 |
| 14 | Do you feel safe and confident?¿Se siente seguro/a y confiado? | 10 |
| 15 | If your situation worsens, do you know what you should do?Si empeora su situación, ¿sabe lo que tiene que hacer? | 11 |
| 16 | Do you expect the use of CPAP therapy to be beneficial?¿Espera encontrar beneficios con el uso de la terapia con CPAP? | 12 |
| 17 | Have you had trouble following other treatments (for example, with an antibiotic)?¿Ha tenido problemas en seguir otros tratamientos (por ejemplo, un antibiótico) | – |
| 18 | Do you have people around you who support you for your health issues?Cuenta con personas de su entorno que le apoyen para lostemas de salud? | – |
Note: Italics for the Spanish version.
The initial pool of 18 items was tested in a sample of 174 patients receiving CPAP treatment from the Spanish public health service free of charge at Hospital Universitario La Princesa (Madrid, Spain). Patients with OSA and a CPAP prescription received treatment by the Hospital Sleep Unit and were provided a CPAP device via a provider, in this case, VitalAire. Patients could go to this provider whenever necessary and were given periodic appointments to review their devices and collect replacement consumable materials. The questionnaire was administered at the beginning of the treatment, specifically after their training at the CPAP School. A follow-up was administered after a 3-month scheduled review. The nurse responsible for these CPAP Schools was trained in the motivational interview technique.
Participants were eligible for inclusion if they were at least 18 years old, had a diagnosis of OSA confirmed by clinical polysomnography or polygraphy, had a clinical recommendation for CPAP treatment, and were on CPAP treatment. Participants were excluded from the study if they were being treated with bi-level ventilation (e.g. due to evidence of Central Sleep Apnoea Syndrome), severe COPD, cognitive disorders or were unable to give informed consent.
In order to calculate the sample size, an effect size of 0.20 was taken as a reference, to be able to detect even small effects31; a power (1–β) of 0.80; and an α=.05. Taking into account the type of analysis (t-tests for comparing means for dependent groups), the calculated sample size was 156. To avoid missing data problems or experimental mortality, it was decided to increase this value in approximately 20 people. Finally, the sample consisted of 174 patients. We evaluated all the patients aged over 18 years undergoing treatment with CPAP who visited a VitalAire service point between March 20 and May 15, 2018 (n=174).
Study 2Study 2 was carried out in patients undergoing treatment with CPAP and supplied by the same treatment provider (VitalAire-Air Liquide Healthcare) via 11 care centres. The Interview was administered to patients who were already on treatment during follow-up visits. The questionnaire was used as a follow-up, in order to detect improvements or problems both in CPAP treatment and in adherence. The a priori estimated sample size was equivalent to that in Study 1, nevertheless a bigger sample including all the cases meeting the inclusion criteria during the research period was used. As the purpose was to take benefit of the possibilities of research in an inaccessible population, we surveyed as many cases as possible in order to generalize results.
The patients came from three geographical areas in Catalonia (corresponding to an approximate population of 1,403,000 inhabitants) and including the Catalunya Central, Camp de Tarragona, Terres de l’Ebre, and Barcelona-Hospital Vall d’Hebron healthcare areas. The evaluations were carried out by nurses from VitalAire during scheduled or spontaneous patient reviews at the care points, after having provided their consent to participation.
Participants were eligible for inclusion if they were at least 18 years old, had a diagnosis of OSA confirmed by clinical polysomnography or polygraphy, had a clinical recommendation for CPAP treatment, and were on CPAP treatment. Participants were excluded from the study if they were being treated with bi-level ventilation (e.g. due to evidence of Central Sleep Apnoea Syndrome), severe COPD, cognitive disorders or were unable to give informed consent.
InstrumentsSeveral socio-demographic data variables were collected alongside the OSA-CPAP Perceived Competence Evaluation Interview, including age, sex, marital status, education level, work status, quality of life, daytime sleepiness, treatment motivation, and treatment adherence. Quality of life was assessed using the Visual Analogical Well-being Scale for sleep Apnea,32 with scores ranging from 0 (‘less favourable well-being’) to 10 (‘more favourable well-being’). Daytime sleepiness was assessed using the Epworth sleepiness scale.33 Treatment motivation was defined according to the Prochaska and DiClemente transtheoretical model30: “the probability that a person begins and continues to adhere to a specific change strategy”, by posing the question, “How motivated to follow the CPAP treatment do you feel?”, with the following answers: ‘not at all motivated’ (=0), ‘not much motivated’ (=1), ‘somewhat motivated’ (=2), ‘quite motivated’ (=3), and ‘very motivated’ (=4). Finally, adherence was measured via a meter incorporated into the CPAP devices which indicated the number of hours per day the patient had used the device.
AnalysesBoth qualitative and quantitative analyses were performed. We took a two-step approach to the qualitative analyses: first, we perform a cognitive analysis (comprehension, form analysis, adaptation of the topics, etc.) of the questionnaire via 12 semi-structured patient interviews; next, we assessed the adequacy of the item content in nominal groups of patients and health professionals to try to establish which items were most valuable (a participant consensus exceeding 75%) and which dimensions were related to these items.
For the quantitative analyses we assessed the equivalence of the original versus the new questionnaire versions by performing a zero-order correlation. Paired t tests were used to check the likelihood the selected items were able to detect improvements in adherence after treatment. We then carried out confirmatory factor analyses (CFAs) to study the internal structure of the questionnaire, and assessed the model fit by using (1) chi-squared tests (where significant results cast doubt onto the model specificity); (2) the comparative fit index (CFI), with values over .95 indicating a good fit34; and (3) the root mean square error of approximation (RMSEA), with values of .05 or less indicating an adequate fit. Given the ordinal nature of the data, the corrected weighted least squares mean and variance (WLSMV) estimation method was used for the CFA.
In order to measure internal consistency, we estimated the composite reliability index (CRI) to study reliability, an index offered in the structural equation model framework because it is more robust.35 Finally, independent t-tests and zero-order correlations were used to study the relation between the OSA-CPAP Perceived Competence Evaluation Interview and sex, age, quality of life, daytime sleepiness, treatment motivation, and treatment adherence.
ResultsStudy 1: qualitative study and initial psychometric propertiesIn Study 1, both the qualitative and quantitative analyses were performed with the 18 initial items. First, we carried out 12 semi-structured interviews using the questionnaire. All the participants were patients receiving CPAP from the Pulmonology Service of the Hospital Universitario La Princesa and were residents in Madrid; they were aged between 46 and 71 years and all gave their consent to participate. Next we analysed two nominal groups: one with patients (n=20, different from the participants of the previous interviews) and the other with health professionals (2 pulmonologist specialists from Hospital Universitario La Princesa, 1 general health psychologist, and 1 nurse from the Hospital Sleep Unit). Based on the insights obtained in the interviews, we discarded 5 items (items 4, 7, 8, 17, and 18) because they corresponded to aspects that could be considered as modulating variables (social support or motivation) within the theoretical model. Thus, we worked with a total of 13 of the 18 initial items.
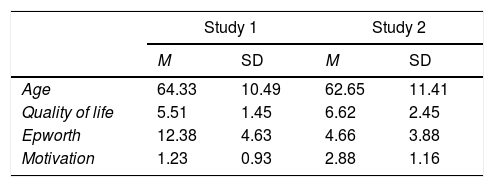
As regards the dimensions, both nominal groups agreed the questionnaire referred to three areas which could be used to evaluate changes at the three-month treatment follow-up: OSA general knowledge and associated risks (lifestyle or healthy habits); CPAP treatment information and expectations; and CPAP use and treatment monitoring and confidence in overcoming the potential obstacles associated with its use. A psychometric study was also carried out in a sample of 174 patients from the Hospital La Princesa (Madrid, Spain), as summarised in Table 2. Additionally, participants’ showed severe OSA, as measured with the Apnea Hypoapnea Index (AHI): mean=40.30 (SD=19.12); median=34.90. Patients’ mean weight was 94.10kg (SD=19.25); median=89.00kg. Finally, to evaluate patients’ CPAP pressure, the used procedure was the “titularity protocol” that consist of applying to every patient his/her values on demand, usually around 12cmH2O (Mean=11.23, SD=2.59).
The psychometric characteristics of the patients included in Studies 1 and 2.
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age | 64.33 | 10.49 | 62.65 | 11.41 |
| Quality of life | 5.51 | 1.45 | 6.62 | 2.45 |
| Epworth | 12.38 | 4.63 | 4.66 | 3.88 |
| Motivation | 1.23 | 0.93 | 2.88 | 1.16 |
| N | % | N | % | |
|---|---|---|---|---|
| Sex | ||||
| Male | 92 | 52.9 | 798 | 78.2 |
| Female | 76 | 43.7 | 223 | 21.8 |
| Missing data | 6 | 3.4 | 0 | 0.0 |
| Marital status | ||||
| Single | 48 | 27.6 | 71 | 7.0 |
| Married | 107 | 61.5 | 797 | 78.1 |
| Divorced/widowed | 19 | 10.9 | 153 | 15.0 |
| Missing data | 0 | 0.0 | 0 | 0.0 |
| Education | ||||
| Primary education | 86 | 49.4 | 422 | 41.3 |
| Secondary education | 56 | 32.2 | 435 | 42.6 |
| University education | 32 | 18.4 | 163 | 16.0 |
| Missing data | 0 | 0.0 | 1 | 0.1 |
| Work status | ||||
| Employed | 78 | 44.8 | 357 | 35.0 |
| Unemployed/not working | 8 | 4.6 | 71 | 7.0 |
| Retired | 88 | 50.6 | 592 | 58.0 |
| Missing data | 0 | 0.0 | 1 | 0.1 |
We performed a Pearson correlation between the original 18-item questionnaire and the version used in Study 1 and found that the 13 items we had retained did indeed maintain the same original meaning (r=.986; p<.001). Thus, removal of these 5 items did not affect the content of the questionnaire, only its length. Regarding the suitability of the three dimensions, paired t-tests showed that they were able to detect an increase in CPAP treatment adherence and showed significant increases in the patient general knowledge of OSA and healthy habits (t[173]=8.097, p<.001, Cohen's d=0.680); CPAP treatment information and expectations (t[173]=15.170, p<.001, Cohen's d=1.115); and CPAP use and treatment monitoring (t[173]=14.642, p<.001, Cohen's d=1.106).
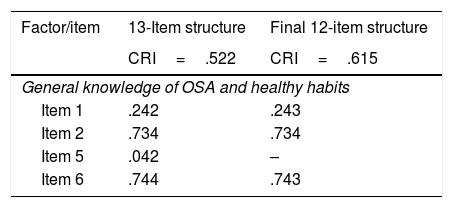
Study 2: Confirmatory factor analysisGiven the qualitative and quantitative evidence in support of the three proposed dimensions for the 13-item version of the survey, we then carried out statistical analyses to confirm this structure in a sample of 1021 patients (see Table 2). A CFA was carried out for the structure of the questionnaire used in Study 1, in which we specified, estimated, and evaluated a second-order structure for the instrument. Thus, a general OSA-CPAP perceived competence factor explained three of the first-order factors: general knowledge of OSA and healthy habits, CPAP treatment information, and CPAP use and treatment monitoring. In turn, these factors explained the 13 items we had retained in Study 1, with an excellent general model fit (χ2[62]=84.975; p=.028; CFI=.965; RMSEA=.019 [.007,.028]). The analytical fit was adequate, except for item 4, which was not statistically significant (p>.050). Therefore, a second CFA was calculated with the same structure, but without item 4. Again, the general fit was excellent (χ2[51]=72.073; p=.027; CFI=.967; RMSEA=.020 [.000,.030]), and the analytical fit was improved, as shown in Table 3.
Factor loadings and reliability estimates for the confirmatory factor analysis Models.
| Factor/item | 13-Item structure | Final 12-item structure |
|---|---|---|
| CRI=.522 | CRI=.615 | |
| General knowledge of OSA and healthy habits | ||
| Item 1 | .242 | .243 |
| Item 2 | .734 | .734 |
| Item 5 | .042 | – |
| Item 6 | .744 | .743 |
| CRI=.590 | CRI=.590 | |
|---|---|---|
| CPAP treatment information | ||
| Item 3 | .280 | .280 |
| Item 9 | .497 | .496 |
| Item 13 | .537 | .537 |
| Item 14 | .351 | .348 |
| Item 16 | .675 | .677 |
| CRI=.742 | CRI=.742 | |
|---|---|---|
| CPAP use and treatment monitoring | ||
| Item 10 | .817 | .816 |
| Item 11 | .603 | .602 |
| Item 12 | .400 | .400 |
| Item 15 | .734 | .734 |
| CRI=.870 | CRI=.793 | |
|---|---|---|
| OSA-CPAP perceived competence (second-order factor) | ||
| General knowledge of OSA and healthy habits | .770 | .553 |
| CPAP treatment information | .717 | .868 |
| CPAP use and treatment monitoring | .990 | .806 |
Notes: The numbering of the initial items are used. Abbreviations: OSA, obstructive sleep; apnoea-hypopnea syndrome; CPAP, continuous positive airway pressure; CRI, composite reliability index.
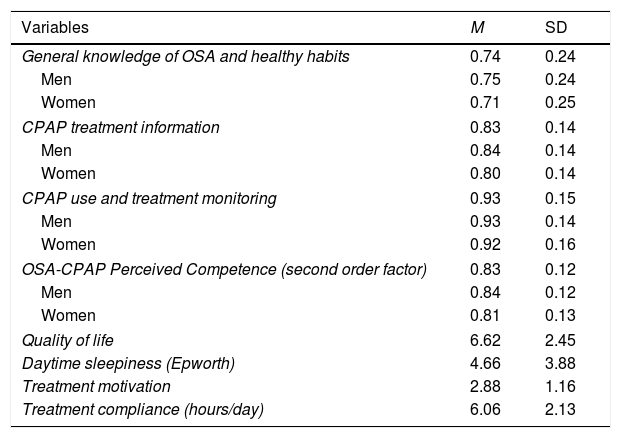
In terms of reliability, the composite reliability index for the 12-item questionnaire was .616 for general knowledge of OSA and healthy habits, .590 for CPAP treatment information, and .742 for CPAP use and treatment monitoring. The CRI for the total score was .793 and the descriptive statistics for the final 12-item questionnaire dimensions are shown in Table 4.
Descriptive statistics for the OSA-CPAP Perceived Competence Evaluation Interview dimensions and quality of life, daytime sleepiness, treatment motivation, and compliance.
| Variables | M | SD |
|---|---|---|
| General knowledge of OSA and healthy habits | 0.74 | 0.24 |
| Men | 0.75 | 0.24 |
| Women | 0.71 | 0.25 |
| CPAP treatment information | 0.83 | 0.14 |
| Men | 0.84 | 0.14 |
| Women | 0.80 | 0.14 |
| CPAP use and treatment monitoring | 0.93 | 0.15 |
| Men | 0.93 | 0.14 |
| Women | 0.92 | 0.16 |
| OSA-CPAP Perceived Competence (second order factor) | 0.83 | 0.12 |
| Men | 0.84 | 0.12 |
| Women | 0.81 | 0.13 |
| Quality of life | 6.62 | 2.45 |
| Daytime sleepiness (Epworth) | 4.66 | 3.88 |
| Treatment motivation | 2.88 | 1.16 |
| Treatment compliance (hours/day) | 6.06 | 2.13 |
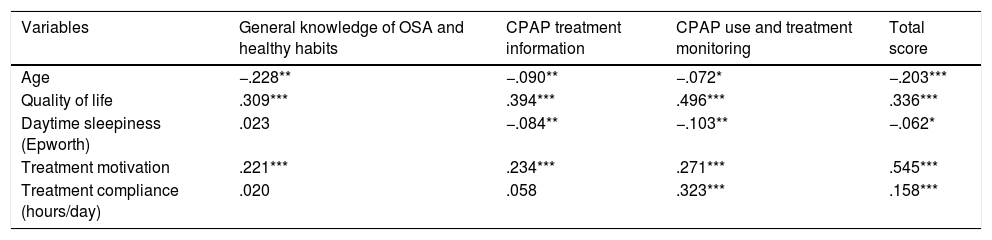
Once evidence for the factor structure and reliability was gathered, t-tests for independent samples were carried out. In all the cases, the means obtained were higher for women (Table 4), and these differences were significant for general knowledge of OSA and healthy habits (t[1,018]=2.190; p=.029), CPAP treatment information (t[1,018]=2.920, p=.004), and the overall OSA-CPAP score (t[1,018]=3.093, p=.002), but not for CPAP use and treatment monitoring (t[1,018]=1.294, p=.196). There was a weak negative relationship between the OSA-CPAP dimensions and age, with the test scores decreasing with age (Table 5). The three dimensions of the OSA-CPAP Perceived Competence Evaluation Interview and the total score were positively related to quality of life and treatment motivation, and treatment adherence was positively related to CPAP use, treatment monitoring, and the total OSA-CPAP score. Finally, the dimensions of CPAP treatment information, CPAP use and treatment monitoring, and the overall score were negatively related to daytime sleepiness, as detailed in Table 5.
Correlations between the OSA-CPAP Perceived Competence Evaluation Interview dimensions, age, quality of life, daytime sleepiness, treatment motivation, and compliance.
| Variables | General knowledge of OSA and healthy habits | CPAP treatment information | CPAP use and treatment monitoring | Total score |
|---|---|---|---|---|
| Age | −.228** | −.090** | −.072* | −.203*** |
| Quality of life | .309*** | .394*** | .496*** | .336*** |
| Daytime sleepiness (Epworth) | .023 | −.084** | −.103** | −.062* |
| Treatment motivation | .221*** | .234*** | .271*** | .545*** |
| Treatment compliance (hours/day) | .020 | .058 | .323*** | .158*** |
The main aim of this study was to present a brief patient-reported outcome measure to assess patients’ levels of adherence with CPAP treatment. Thus, we developed the OSA-CPAP Perceived Competence Evaluation Interview based on motivational interview and Olsen et al.’s results.29,30 We showed that this 13-item interview adequately encompassed the approaches of both patients and professionals to CPAP treatment and sleep apnoea, and captured the same content as the original questionnaire with near perfect correlation (Study 1). This interview was also related to CPAP treatment use, as shown by the significant improvements we found in its three dimensions (general knowledge of OSA and healthy habits, CPAP treatment information, and CPAP use and treatment monitoring) after three months of CPAP therapy (Study 1).
Moreover, CPAP use and treatment monitoring were significantly and positively related to hours of CPAP use per day, and more importantly, to the overall interview score (Study 2). Adherence is one of the most challenging aspects of CPAP treatment success, because up to 50% of patients discontinue CPAP treatment during the first week of using it.10 Our findings indicate that patients with low scores on this interview will likely have lower levels of CPAP treatment hours of CPAP use/day and so we believe this instrument can help clinicians to identify the patient subgroup likely to have low adherence levels in order to try to prevent these dropouts.
Regarding construct validity, our CFA analysis indicated an excellent fit and provided evidence for three dimensions: general knowledge of OSA and healthy habits, CPAP treatment information, and CPAP use and treatment monitoring, as well as a second-order OSA-CPAP perceived competence factor. These dimensions represent constructs that have been previously related to treatment adherence (such as healthy beliefs and behaviours20,21 and self-efficacy), which can be achieved by obtaining higher scores in CPAP treatment information and use.23,24 These dimensions can be adequately represented by a higher-order factor, which means we can both provide general information of perceived competence, and specific input on the three dimensions. Indeed, the dimensions have similar patterns of relations with the variables under study (age, quality of life, daytime sleepiness, treatment motivation, and adherence), but relations differ on their size, being CPAP use and treatment monitoring the most important in terms of adherence, quality of life, and treatment motivation.
When we examined the reliability of the dimensions we found that the estimate for CPAP use and treatment monitoring was adequate, but the reliability of general knowledge of the OSA and healthy habits and CPAP treatment information dimensions were not as good as expected. Nonetheless, the overall OSA-CPAP dimension reliability was adequate. Although this may be a limitation of the questionnaire, in our opinion, the adequate representativeness of the construct items prevails and thus, we believe the usefulness principle should be applied. Moreover, we welcome future studies designed to test this instrument using other reliability estimates such as test-retest consistency measures or information functions.
Finally, in agreement with previously published literature,19,36 we found relationships between the OSA-CPAP Perceived Competence Evaluation Interview dimensions and socio-demographic characteristics such as sex, age, quality of life, daytime sleepiness, and treatment motivation. Our data suggest that older men who report higher levels of daytime sleep and a lower quality of life and motivation levels, have a higher risk of poor adherence. Thus, these results provide important information about the profiles that should be targeted when trying to detect patients that may have potential CPAP perceived competence. Although the total score in the Interview was positive and statistically significant related to treatment compliance (hours/day), the relation was small. This relation was bigger in the case of the dimension of CPAP use and treatment monitoring. Therefore, our resources should be focused on improving patients’ knowledge on the usage of the CPAP, when our aim is to improve their treatment compliance.
Contrary to what happens with the SEMSA questionnaire (whose items attend more to the set of beliefs around the treatment, considering its risks and benefits), current questionnaire is based on the perceived competence. It assesses how the patient believes is involved in CPAP therapy from a treatment control perspective (her/his aptitudes, management, etc.) and knowledge (awareness of disease, benefits, risks, etc.).
One constraint of the OSA-CPAP Perceived Competence Evaluation Interview was that our results were limited to the Spanish context. Therefore, we encourage other academics and clinicians to use this new instrument in other contexts and report their results. Another limitation of current research are the differences between the participants in Study 1 and 2. As participants in Study 1 were evaluated before CPAP treatment, they showed higher levels of sleepiness and lower levels of quality of life, when compared to participants of Study 2, already in treatment. However, these results could be understood as a strength, as the questionnaire has shown an adequate performance in patients with different characteristics, at the same time, we should be cautious in the conclusions drawn from these two studies. Additionally, in Study 2, with patients already following treatment with CPAP, no information on pressure, mask leaks or AHI was registered. This is, therefore, a third limitation of the study.
ConclusionBased on the results we present in this current manuscript, this interview seems to be a very useful tool for assessing levels of patient adherence which we believe could be used to promote strategies to improve adherence through education about CPAP as well as patient motivational stimuli.