A 53-year-old man, active smoker with a cumulative dose of 40 pack-years, COPD GOLD 4C (FEV1/FVC 45%, FEV1 28%, FVC 38%), was admitted to the ICU for septic shock and severe acute hepatitis requiring vasoactive support, intubation, and invasive mechanical ventilation. Progress in the ICU continued to be poor with multiple complications, and percutaneous tracheostomy was required due to prolonged weaning. He subsequently improved, and could be decannulated with satisfactory tracheostomy closure.1
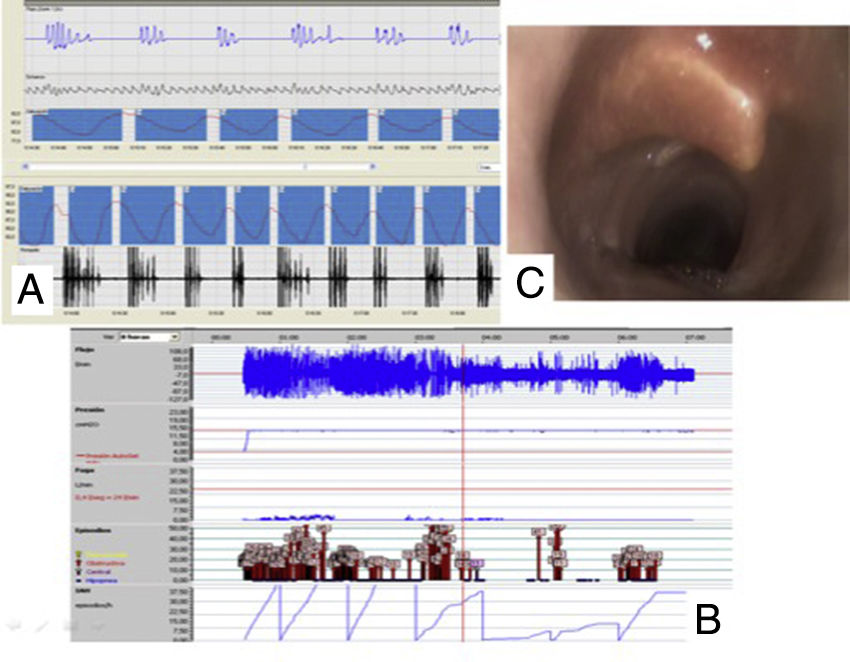
During admission, the patient presented nocturnal apneas without laryngeal stridor, so a sleep study with respiratory polygraphy was performed, which recorded a high number of obstructive respiratory events (AHI 108, CT90 99% and Oxygen Desaturation Index (ODI) 92) that were not corrected with CPAP at 14cmH2O, demonstrated by persistent respiratory events on the pressure recording of the AutoCPAP readout (Fig. 1).
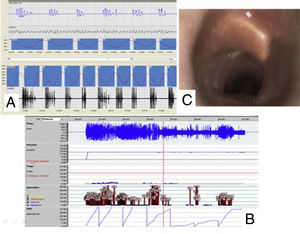
In view of the patient's recent tracheostomy, the evaluation was completed with fiberoptic bronchoscopy under sedation, revealing of note the image of a dislocation/rupture of one of the tracheal cartilages immediately below the glottis that could be the cause of the upper airway obstruction that failed to respond to CPAP, but showed partial response to NIV support in ST mode IPAP 17/EPAP 12, BR 16/min (Breathing Rate), that could subsequently be maintained.
We thank the multidisciplinary team of Sleep Unit and Non-Invasive Ventilation of the Hospital Clinic y Provincial de Barcelona.
Please cite this article as: Matute Villacís MC, Albácar Ingla N, Embid López C. Obstrucción de la vía aérea superior sin respuesta a CPAP. Arch Bronconeumol. 2018;54:578.