The National COPD Strategy in Spain was first approved in 2009.1 We are now in 2020, and the ten points we present in Table 1 go beyond the clinical guidelines and complexity of the process itself and its current status, and seek to identify issues and possible solutions to the problem of COPD in Spain, focusing on policy and the health authorities.
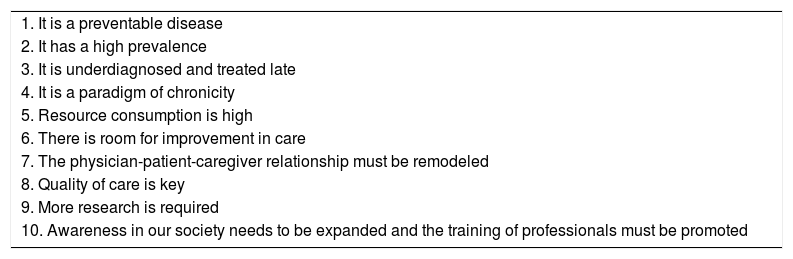
Decalogue of COPD.
| 1. It is a preventable disease |
| 2. It has a high prevalence |
| 3. It is underdiagnosed and treated late |
| 4. It is a paradigm of chronicity |
| 5. Resource consumption is high |
| 6. There is room for improvement in care |
| 7. The physician-patient-caregiver relationship must be remodeled |
| 8. Quality of care is key |
| 9. More research is required |
| 10. Awareness in our society needs to be expanded and the training of professionals must be promoted |
COPD is a preventable and treatable disease,2,3 the main cause of which in Spain is smoking. Recent trends in smoking among women and children, along with the new vaping and “heat-not-burn” devices, are creating new challenges. In Spain, smoking leads to the loss of 1 million life years annually, and 28,766 people die of COPD every year.4 COPD is still highly prevalent, and the EPISCAN II study concludes that 11.8% of Spain's citizens aged 40 or older (14.6% men and 9.4% women) have this disease,5 and that prevalence among younger patients and women is increasing.6 Unfortunately, COPD is still underdiagnosed and treated late: despite the efforts and resources devoted to performing spirometry in primary care, underdiagnosis is as high as 74.7%.6 EPISCAN II also confirms the so-called "Spanish paradox", in which underdiagnosis is greater in women.7 COPD is the paradigm of a chronic, progressive, incapacitating disease with frequent extrapulmonary manifestations and comorbidities, and a prevalence that increases with age. A comprehensive, multidisciplinary approach which incorporates a gender perspective is needed.
Use of resources associated with COPD is high, up to 3 bn Euros a year (0.2% of GDP): most expenditure goes on hospitalization, and 15% of patients consume 80% of all resources.8 There is clearly room for improvement in the care of COPD, the main issues being the low number of quality spirometries being performed,9 and the urgent need for advanced nursing skills, comprehensive process management, and prioritization using health indicators.10 Alternatives to conventional hospitalization such as home care and new technologies should be promoted11 with collaborative intervention by the public and private sectors and coordination among the different agencies involved.
We believe that the physician-patient-caregiver relationship must become a true "therapeutic alliance". The new key words in COPD are self-care, adherence, appropriate use of resources, and empowerment of patient associations, all underpinned by quality of care. Quality scientific and technical policies must be implemented, and quality standards ensuring personalized treatment must be established in regularly updated guidelines.
Sponsorship of translational research in both prevention and comprehensive care is essential. Finally, all stakeholders must collaborate in disseminating knowledge to both society and professionals. COPD is changing, and there are still a great many unknowns,12 but awareness must increase,13,14 so we propose writing the copd acronym in lower case to emphasize that this is a disease of capital importance.
In short, the copd patient is a VIP - a very important patient - to whom we must offer a longer and better quality of life. This problem and its causes must be tackled more efficiently in the coming decade, and if we all work together perhaps we can put an end to copd.15
There was no funding associated with this manuscript.
Please cite this article as: Ancochea J, Soriano JB. La EPOC en España al inicio de una nueva década. Arch Bronconeumol. 2020;57:1–2.