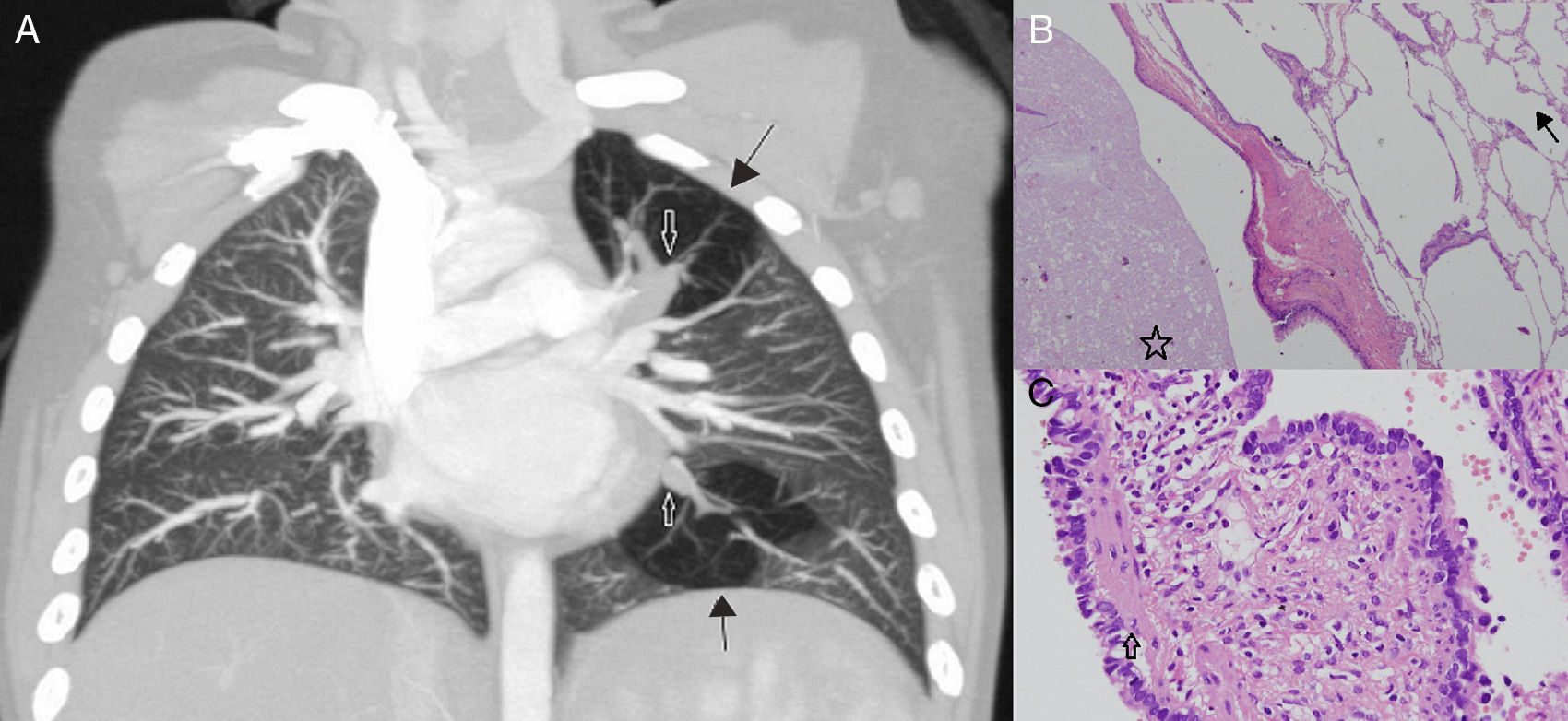
A 2 year-old girl presented with a 6-month history of recurrent airway infections. On anteroposterior chest X-ray, focal radiolucent areas were seen in both the upper zone and paracardiac region of the left lung. On contrast-enhanced chest computed tomography, central mucocele formations were observed in the left perihilar region, together with bi-segmental air trapping and oligaemia, suggestive of bi-segmental bronchial atresia (Fig. 1A). The patient underwent bi-segmentectomy. The histopathology report included mucocele formations and emphysematous changes confirming bronchial atresia, together with respiratory epithelial lined cysts and a thin fibromuscular layer in the cyst wall, suggesting areas of focal congenital pulmonary airway malformation (CPAM) (Fig. 1B).
(A) Contrast-enhanced, coronal plane, chest computed tomography. Closed arrows show mucoceles and black arrows show air-trapped segments. (B) Haematoxylin–eosin, ×100 magnification. The air trapping areas (open arrow) and mucocele (asterix), confirming bronchial atresia. (C) Haematoxylin–eosin, ×400 magnification. CPAM areas (closed arrow) showed by respiratory epithelial lined cysts and a thin fibromuscular layer in the cyst wall.
CPAM areas within bi-segmental bronchial atresia is an extremely interesting presentation.1 To the best of our knowledge, this is the first such case reported in the literature. This case is an example of type 4 CPAM that is generally part of the differential diagnosis of focal air-trapping. CPAM is associated with increased incidence of pulmonary malignancy in addition to pulmonary and extrapulmonary malformations. Pleuropulmonary blastoma, bronchioloalveolar carcinoma and rhabdomyosarcoma are the most common malignancies associated with CPAM.2 The presence of CPAM areas within bi-segmental bronchial atresia requires long-term follow-up due to the increased risk of malignancy.