To analyse the clinical utility and economic impact of conventional transbronchial needle aspiration (TBNA) in patients with diagnosis of bronchogenic carcinoma (BC) and mediastinal lymphadenopathies in thoracic computed tomography (CT). To assess the predictive factors of valid aspirations.
Patients and methodsRetrospective observational study between 2006 and 2011 of all TBNA performed in patients with final diagnosis of BC and accessible hilar or mediastinal lymphadenopathies on thoracic CT.
ResultsWe performed TBNA on 267 lymphadenopathies of 192 patients. In 34.9% of patients, two or more lymph nodes were biopsied. Valid aspirations were obtained in 153 patients (79.7%) that were diagnostic in 124 patients (64.6%). Multivariate analysis showed that factors associated with valid or diagnostic results are the diameter of the lymph node and the number of lymph nodes explored. TBNA was the only endoscopic technique that provided the diagnosis of BC in 54 patients (28.1%). Staging mediastinoscopy was avoided in 67.6% of patients. The prevalence of mediastinal lymph node involvement was 74.4%, sensitivity of TBNA was 86.2% and negative predictive value was 63.6%. Including mediastinoscopy and other avoided diagnostic techniques, TBNA saved 451.57€ per patient.
ConclusionsTBNA is a clinically useful, cost-effective technique in patients with BC and mediastinal or hilar lymphadenopathies. It should therefore be performed on a regular basis during diagnostic bronchoscopy of these patients.
Analizar la utilidad clínica y el impacto económico de la punción transbronquial convencional (PTBC) en los pacientes con carcinoma broncogénico (CB) y adenopatías mediastínicas en la tomografía computarizada (TC) torácica. Analizar los factores predictores de punción válida.
Pacientes y métodosEstudio observacional retrospectivo entre 2006 y 2011 de todas las PTBC realizadas a pacientes con CB y adenopatías mediastínicas o hiliares accesibles a la técnica en la TC torácica.
ResultadosSe realizó PTBC sobre 267 adenopatías de 192 pacientes. En el 34,9% de los pacientes se pinchó más de una adenopatía. Se obtuvo punción válida en 153 pacientes (79,7%) y diagnóstica en 124 (64,6%). El análisis multivariante mostró que los factores que se asocian a la obtención de punción válida y diagnóstica son el diámetro de la adenopatía y el número de adenopatías pinchadas. La PTBC fue la única técnica endoscópica que permitió el diagnóstico de CB en 54 pacientes (28,1%). La PTBC evitó el 67,6% de las mediastinoscopias de estadificación. La prevalencia de afectación tumoral mediastínica fue del 74,4%, la sensibilidad de la PTBC del 86,2% y el valor predictivo negativo del 63,6%. Entre mediastinoscopias y otras técnicas diagnósticas evitadas, la PTBC ha supuesto un ahorro de 451,57 € por paciente estudiado.
ConclusionesLa PTBC es una técnica clínicamente útil y económicamente rentable en los pacientes con CB y adenopatías patológicas mediastínicas o hiliares, por lo que debería ser realizada como una técnica endoscópica más, de forma habitual, en estos pacientes.
Transbronchial needle aspiration of mediastinal structures was described by Schiepatti1 in 1949, but its use with flexible bronchoscopy was described and systematised by Wang2 in 1978 Currently the usefulness of conventional trans-bronchial aspiration (TBNA) lies mainly in its effectiveness as a diagnostic tool and in the mediastinal staging of bronchial carcinoma (BC).3–7 It is a simple technique to learn, with a short learning curve,8 and has proven to be cost-effective,9,10 despite which it has always been underused.11,12 Although there are as yet no studies dealing with it, we have good reason to believe that its use has decreased since endobronchial ultrasound-guided fine-needle aspiration (EBUS-FNA), or endoscopic ultra-sound guided transoesophagal fine-needle aspiration (EUS-TOFNA), were introduced. Indeed, the SEPAR guidelines on Lung Cancer13 staging identifies EBUS/EUS-FNA as the first choice for mediastinal staging, and refers to TBNA as a strategy which “would be acceptable in centres not equipped with PET, EBUS or EUS, despite the fact that other guidelines14 and modifications of the SEPA guidelines15 exist in which experts recommend that TBNA should always be carried out during bronchoscopic diagnosis whenever the thoracic CT scan reveals the presence of mediastinal or hilar pathology”.
The main aim of this study is use of the thoracic CT scan to examine the clinical and economic utility of TBNA in patients with BC and mediastinal pathologies, and the secondary aim is to examine the factors which might influence the result of such needle aspiration.
Patients and MethodsA retrospective observational study of all patients on whom TBNA of mediastinal and hilar adenopathies was performed at the University Hospital of Guadalajara, and who were consequently diagnosed with BC, between June 2006 and June 2011. TBNA was performed on all patients for whom it was considered appropriate following a bronchoscopy, and in whom the thoracic CT scan revealed the presence of adenopathies. Our diagnostic protocol for BC includes the performance of a thoracoabdominal CT scan prior to the use of diagnostic bronchoscopy.
The University Hospital, which is the only public general hospital in the Guadalajara area, caters for a population of 238000 and has 410 beds. An average of 500 bronchoscopies were carried out every year.
These bronchoscopies, all of which were on an out-patient basis, except when the patient had been hospitalised for some other reason, were performed using several different Olympus videobronchoscopies. Local anaesthetic, in the form of lidocaine at 2% and propofol sedation, was administered by the staff who carried out the bronchoscope. During bronchoscopy continuous ECG, blood pressure and pulse oximetry, oxygen saturation monitoring was carried out, with oxygen being administered at 4l/min by means of a nasopharyngeal cannula. Aspiration location was chosen on the basis of a careful examination of the thoracic CT scan, in which the diameter of each adenopathy was measured at their minor axis. For TBNA, 21 gauge eXcelon needles were used (Boston Scientific, Natick, MA, USA). The TBNA was always the first endoscopic technique to be applied, following the transnasal insertion of the bronchoscope, care being taken to avoid, as far as possible, aspiration of any secretions which might contaminate the working channel As no cytologist was present in the bronchoscopy room, in order to achieve the best possible diagnostic performance, the TBNA was carried out on the largest possible number of adenopathies, always beginning with the lymph node station, where the No. value was higher. Between 2 and 4 aspirations were performed for each adenopathy, and the samples obtained were sent to Anatomical Pathologies for analysis on microscope slides and fixed in 96 alcohol (until November 2009), or suspended in liquid methanol (CytoLyt, Cytyc Corporation, Boxborough, MA, USA) (from November 2009 onwards). Those cases in which the bronchial mucous at location of the aspiration did not present a normal macroscopic appearance were excluded from the study. 98% of the bronchoscopies were carried out by the same endoscopist (JCN).
An aspiration was considered valid when a BC diagnostic sample was obtained, or when there was a sufficient number of lymphocytes were obtained to ensure that they came from the lymphatic gland, and invalid when only bronchial cells, blood, necrotic material or samples suspected of being malignant were obtained, but which could not provide a clear basis for confident diagnosis. The protocol was approved by the Ethical Committee of Clinical Research at the Centre.
For the analysis of the economic impact the following cost parameters were used, obtained from the Hospital's Economic Management Service, and from the literature from our research field10,15–18: aspiration needle: 80EUR; anatomopathological study: 38EUR; bronchoscopy: 120EUR; CT guided transthoracic PAAF: 767EUR; bronchoscopy: 3000EUR.
Statistical AnalysisThe results of the qualitative variable are expressed as percentages and absolute frequencies. For the qualitative variable the media and standard deviation are expressed. The comparison of discrete variables was carried out by means of the chi-square test, and that of independent means of quantitative variables using Student's t-test. P<.05 was considered statistically significant. For multivariate analysis a model of binary logistical regression with the Hosmer–Lemeshow goodness of fit test. In the multivariate analysis all those factors were included which produced a P<.1 result in the bivariate analysis. For the statistical analysis the software used was SPSS version 15.0 for Windows. The prevalence, sensitivity and specificity, predictive positive value and predictive negative value were determined using standard definitions.
ResultsDuring the period of the study TBNA was performed on mediastinal adenopathies in 320 patients, who constituted the study population, with a final BC diagnosis in 192 cases. (Of the remaining 128, 25 presented malignant tumours, and 103 a range of non-tumoural conditions.) The average age was 67.2±11 years. 79.2% were men.
Diagnostic distribution was as follows: adenocarcinoma (63 cases, 32.8%), epidermoid (46 cases, 24%), microcytic (45 cases 23.4%), no small cells (34 cases, 17.1%), neuroendocrine (2 cases, 1%), low grade neuroendocrine (1 case, 0.5%), mucoepidermoid (1 case, 0.5%).
In 59 patients (30.7%) TBNA was carried out on 2 adenopathies, and in 8 patients (4.2%) on 3 adenopathies. In 160 patients (83.3%) a further endoscopic technique, in addition to TBNA, was carried out: bronchial brushing in 59 cases (30.7%), bronchoalveolar lavage in 8 cases (4.2%) and transbronchial biopsy in 68 cases (35.5%).
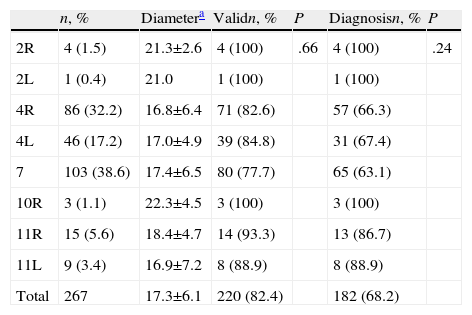
In 153 patients (79.7%) a valid aspiration was obtained, and in 124 cases (64.6%), this aspiration was diagnostic. TBNA was applied to 267 adenopathies (an average of 1.4 per patient), the distribution of which, by lymph gland stations, is shown in Table 1. Aspiration was valid in 220 patients (82.4%) and resulted in diagnosis in 182 cases (68.2%). With the exception of some instances of slight bleeding at the aspiration point, no serious complications attributable to the technique could be observed. In 4 patients clearly haematic material was obtained, indicating a vascular structure aspiration, and in all four cases the location was subcarinal.
Distribution, by Lymph Notes, of the Biopsied Adenopathies.
| n, % | Diametera | Validn, % | P | Diagnosisn, % | P | |
| 2R | 4 (1.5) | 21.3±2.6 | 4 (100) | .66 | 4 (100) | .24 |
| 2L | 1 (0.4) | 21.0 | 1 (100) | 1 (100) | ||
| 4R | 86 (32.2) | 16.8±6.4 | 71 (82.6) | 57 (66.3) | ||
| 4L | 46 (17.2) | 17.0±4.9 | 39 (84.8) | 31 (67.4) | ||
| 7 | 103 (38.6) | 17.4±6.5 | 80 (77.7) | 65 (63.1) | ||
| 10R | 3 (1.1) | 22.3±4.5 | 3 (100) | 3 (100) | ||
| 11R | 15 (5.6) | 18.4±4.7 | 14 (93.3) | 13 (86.7) | ||
| 11L | 9 (3.4) | 16.9±7.2 | 8 (88.9) | 8 (88.9) | ||
| Total | 267 | 17.3±6.1 | 220 (82.4) | 182 (68.2) |
The average diameter of the adenopathies was carried out was 17.3±6.1mm (range: 7–38mm).
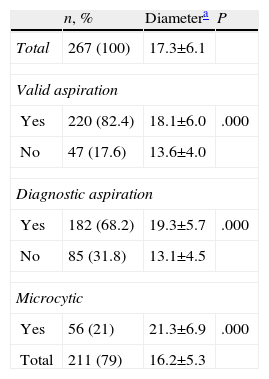
Table 2 shows the diameter comparisons in the valid samples, the diagnostic samples and the instances of microcytic carcinoma as opposed to other histological types.
Size of the Adenopathies. Comparison Between Valid Samples, Diagnostic Samples, and Instances of Microcytic (See Text).
| n, % | Diametera | P | |
| Total | 267 (100) | 17.3±6.1 | |
| Valid aspiration | |||
| Yes | 220 (82.4) | 18.1±6.0 | .000 |
| No | 47 (17.6) | 13.6±4.0 | |
| Diagnostic aspiration | |||
| Yes | 182 (68.2) | 19.3±5.7 | .000 |
| No | 85 (31.8) | 13.1±4.5 | |
| Microcytic | |||
| Yes | 56 (21) | 21.3±6.9 | .000 |
| Total | 211 (79) | 16.2±5.3 | |
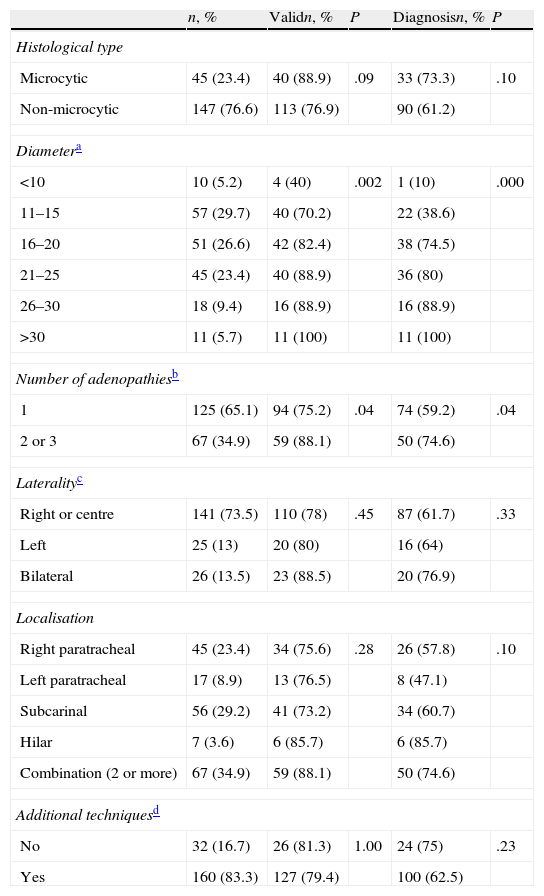
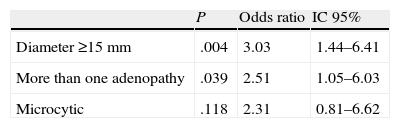
Table 3 shows the bivariate analysis of the factors in which an association with the obtaining of valid and diagnostic aspiration was considered. In both cases, the diameter of the adenopathy and the number of adenopathies biopsied during the procedure achieve statistical significance, and, although it is not statistically significant, there is a tendency in these cases towards microcytic carcinoma.
Bivariate Analysis for the Obtaining of a Valid and Diagnostic Aspiration.
| n, % | Validn, % | P | Diagnosisn, % | P | |
| Histological type | |||||
| Microcytic | 45 (23.4) | 40 (88.9) | .09 | 33 (73.3) | .10 |
| Non-microcytic | 147 (76.6) | 113 (76.9) | 90 (61.2) | ||
| Diametera | |||||
| <10 | 10 (5.2) | 4 (40) | .002 | 1 (10) | .000 |
| 11–15 | 57 (29.7) | 40 (70.2) | 22 (38.6) | ||
| 16–20 | 51 (26.6) | 42 (82.4) | 38 (74.5) | ||
| 21–25 | 45 (23.4) | 40 (88.9) | 36 (80) | ||
| 26–30 | 18 (9.4) | 16 (88.9) | 16 (88.9) | ||
| >30 | 11 (5.7) | 11 (100) | 11 (100) | ||
| Number of adenopathiesb | |||||
| 1 | 125 (65.1) | 94 (75.2) | .04 | 74 (59.2) | .04 |
| 2 or 3 | 67 (34.9) | 59 (88.1) | 50 (74.6) | ||
| Lateralityc | |||||
| Right or centre | 141 (73.5) | 110 (78) | .45 | 87 (61.7) | .33 |
| Left | 25 (13) | 20 (80) | 16 (64) | ||
| Bilateral | 26 (13.5) | 23 (88.5) | 20 (76.9) | ||
| Localisation | |||||
| Right paratracheal | 45 (23.4) | 34 (75.6) | .28 | 26 (57.8) | .10 |
| Left paratracheal | 17 (8.9) | 13 (76.5) | 8 (47.1) | ||
| Subcarinal | 56 (29.2) | 41 (73.2) | 34 (60.7) | ||
| Hilar | 7 (3.6) | 6 (85.7) | 6 (85.7) | ||
| Combination (2 or more) | 67 (34.9) | 59 (88.1) | 50 (74.6) | ||
| Additional techniquesd | |||||
| No | 32 (16.7) | 26 (81.3) | 1.00 | 24 (75) | .23 |
| Yes | 160 (83.3) | 127 (79.4) | 100 (62.5) | ||
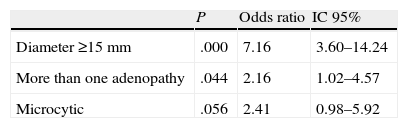
Tables 4 and 5 show the results of the multivariate analysis aimed at obtaining valid and diagnostic samples. Once again, the size of the adenopathy and the number of adenopathies biopsied during the procedure are shown to achieve statistical significance, and there is a non-significant tendency towards microcyte in the case of the diagnostic sample.
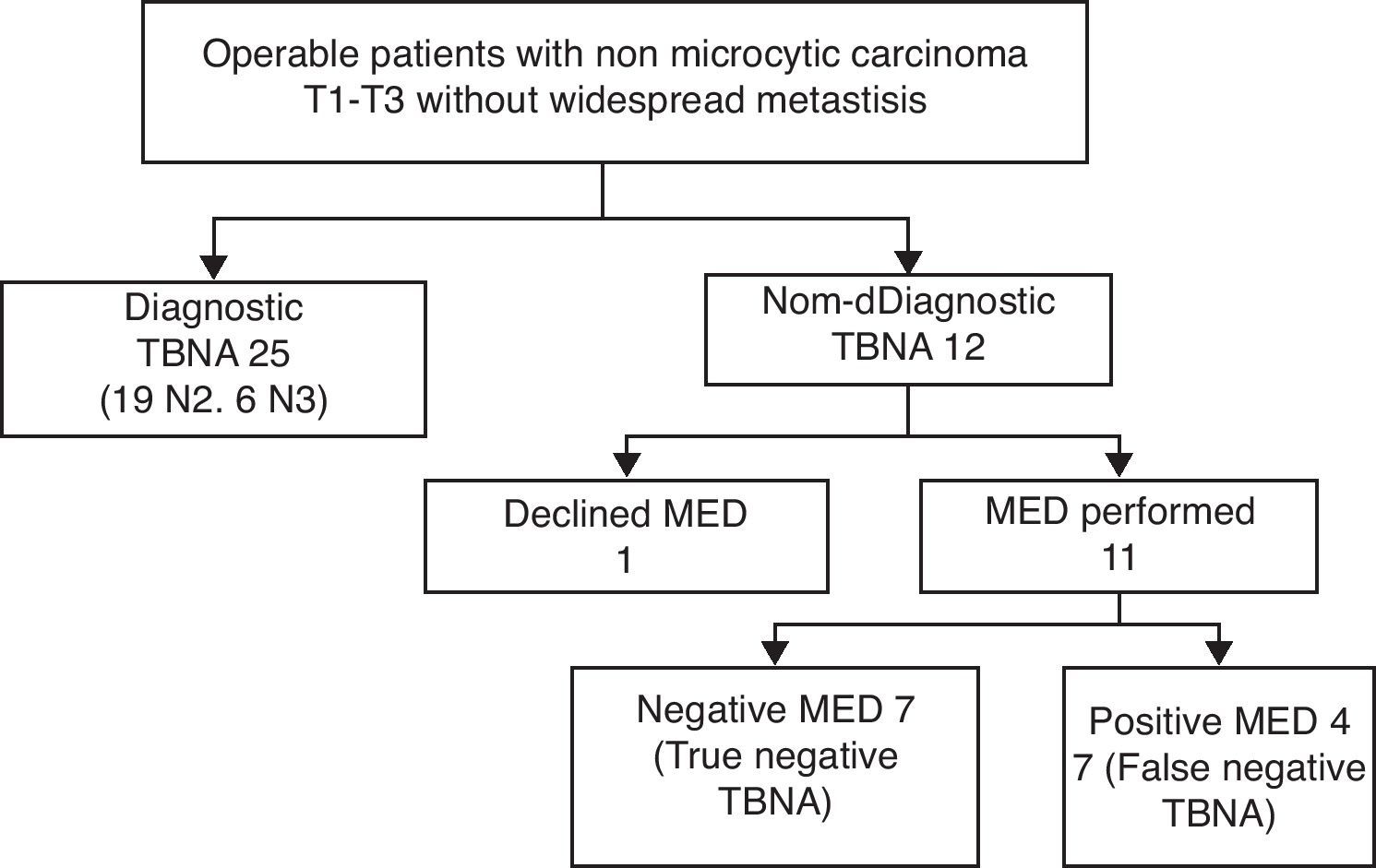
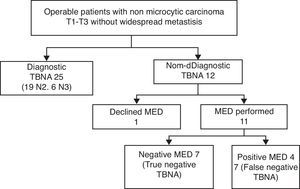
In 54 patients (28.1%) the TBNA was the only endoscopic technique that enabled BC to be diagnosed. Of the 192 patients, 37 presented non-microcytic BC, T1–T3, with no widespread metastasis, and surgery was viable, which suggested the appropriateness of staging mediastinoscopy. In 25 (67.6%) (19 N2, 6 N3) of these cases TBNA revealed the presence of a mediastinal tumour, as a result of which mediastinoscopy was unnecessary. Of the remaining 12 patients, one opted against mediastinoscopy, and of the other 11, tumours were shown to be absent in 7 cases (true cases of negative TBNA) and present in 4 (3 adenocarcinomas, 1 epidermoid) (false TBNA negatives). The flow of patients is shown in Fig. 1. The prevalence of mediastinal tumours in this sub-group of patients was 74.4%, and TBNA, and the sensitivity of the TBNA was 86.2%, its specificity 100% and its negative value 63.6%.
Economic ImpactThe added cost of the performance of TBNA is the sum of the cast of needle aspiration and the cytological study carried out on the sample. That is to say: 80EUR+38EUR per patient, the total cost for the whole study population therefore being (192×118) 22656EUR. The saving represented by the TBNA is the result of two factors: (a) the avoidance of 25 staging mediastinoscopies: which, multiplied by 3000EUR means a saving of 75000EUR. (b) In 54 additional cases, TBNA was the only endoscopic technique that enabled BC to be diagnosed. In 10 of these patients the diagnosis had already been made by other means (in 7 pleural liquid, in 2 by supraclavicular adenopathy aspiration and in one case by aspiration of the lesion occupying the hepatic space). But in the case of the 44 remaining patients, it would have been necessary, in the absence of TBNA, to use some other diagnostic technique. In 31 of these patients, the chosen technique would have been the CT-guided FNAC (a saving of 23777EUR), in 10 a bronchoscopy would have been performed (a saving of 1580EUR), and in 3 the chosen method would have been the performance of a diagnostic mediastinoscopy (a saving of 9000EUR). The total amount saved in this section comes to 34357EUR. The total economic impact has therefore been a saving of 86701EUR during the period of the study, which represents a saving of 451.57EUR per patient.
DiscussionThe results of this study may well help to provide answers to some of the questions surrounding the use of TBNA in patients with BC and adenopathies revealed in the thoracic CT scan.
What Are the Factors That Enable Us to Predict a Valid Sample From Aspiration?This aspect has been analysed on numerous occasions. In previous studies6,7,19,20 the main factors associated with the obtaining of a valid sample have been the size of the adenopathy, the location of the adenopathy in the right or central lymph nodes and the fact of it being a microcytic carcinoma. The best study in this respect is that of Fernández-Villar et al.,21 as it is based on a large number of patients and is one of the few studies in which a multivariate analysis is carried out. In this series the main factor associated independently with the obtaining of diagnostic samples was the diameter of the adenopathy, with the presence of indirect signs in the location of the aspiration also reaching statistical significance. In our study, like in the other published studies, as the diameter of the adenopathy increases, so too does the probability of obtaining a diagnostic aspiration.
While the cut-off point at which a TBNA is considered advisable has conventionally been less than 10mm at its minor axis, of the 10 patients who presented adenopathies that were smaller than this 4 produced valid samples, even though only one resulted in cancer diagnosis (one case of microcytic carcinoma).
In the multivariate analysis for obtaining a valid aspiration, the diameter of the adenopathy is of particular relevance, in line with studies published hitherto. What is also of statistical significance, and this is an aspect which is analysed here for the first time, is the number of lymph nodes biopsied during the bronchoscopy (in 34% of the bronchoscopies carried out more than one lymph node, as opposed to 17.4% in the study conducted by Fernández-Villar, but it must be borne in mid that a cytologist was present in the bronchoscopy room), without significant differences being observed in the diameter (18.7±6.4mm in the patients in which more than one adenopathy was biopsied. as opposed to 17.5±6.4mm in patients in whom only one was; P=.22). The percentage of microcytic carcinoma was higher in whom only one adenopathy was biopsied (36 out of 125 [38.8%] as opposed to 9 out of 67 [13.4%]; P=.02).
In the multivariate analysis for obtaining a diagnostic aspiration it is possible to observe a trend, which is close to achieving statistical significance in favour of the presence of microcytic carcinoma, which could be explained by the well-known greater aggressiveness of this histological type.6,7,22 No significant reduction has been observed in the diagnostic reliability of TBNA between bronchoscopies in which other additional diagnostic techniques (brushing, bronchioalveolar lavage, bronchial biopsy, transbronchial biopsy) and those in which only one endoscopic technique was used during diagnostic bronchoscopy.
With regard to the laterality of the adenopathies, there is no difference in the probability of either valid or diagnostic aspiration whether the left nodes, right nodes, and nodes situated in the centre are biopsied or bilateral nodes, a result which is reinforced by the fact that the size is similar (17.0±5.2mm in the left nodes and 17.4±6.3mm in the right or middle nodes, P=.72). There was no significant difference in the percentage of microcytics (23.2% in the left; 20.4% in the right or central; P=.71). Nor were any differences observed between the right paratracheal, the left paratracheal, the subcarinal or the hilar adenopathies, although there was a tendency, albeit not a significant one, towards a greater diagnostic performance in the hilar adenopathies, without any significant difference in size being observed (18.3±5.7mm in the hiliar adenopathies; 17.2±6.2 in the non-hilar adenopathies; P=.39), probably on account of the fact that the there are more reliable anatomical references for aspiration of hilar adenopathies.
Is Conventional Transbronchial Needle Aspiration Clinically Useful?Although there is no canonical definition for the concept of the clinical usefulness23,24 of a diagnostic test such as TBNA, it could be said to be clinically useful when the result permits us to confirm (or rule out) a given diagnosis, or when it has resulted in the diagnostic or therapeutic approach to the patient being modified.
In our study, TBNA is the only endoscopic technique that has resulted in a BC diagnosis in 28.1% of the patients. This result is slightly lower than that obtained by Fernández-Villar,22 and similar to results reported by other authors.6,16,19 Of the 54 patients in whom TBNA was the only endoscopic technique which produced a diagnosis, in 44 cases (22.9%) additional diagnostic tests could be avoided, so that money is saved, diagnostic delays are avoided and mortality might well be reduced.
On the other hand, the group in which TBNA has a direct impact on the diagnostic and therapeutic approach to be adopted is that made up of operable patients with potentially resectable non-microcytic carcinoma. Of the 37 patients in our series belonging to this group, TBNA produced a positive N2 or N3 diagnosis in 25 (67.6%), with the resulting avoidance of a mediastinoscopy. In this group TBNA showed a sensitivity of 86.2%, and a negative predictive value of 63.6%, with a mediastinal tumour prevalence of 74.4%.
These results are similar to those recorded by other authors.9,10,16,25 There is a small difference between the percentage of patients with non-microcytic carcinoma in whom a diagnostic aspiration was obtained with respect to the whole group (61.2%) and the operable and potentially resectable group (67.6%). This difference could be explained by the fact that in the total group of patients more than one adenopathy was biopsied in 46 out of 147 (31%), while in the operable group this was done in 19 out of 35 (55%) (the most frequent combination was aspiration in adenopathies 4R and 7). Undoubtedly, the performance of a more sophisticated technique, such as PTB-EBUS or PET-EUS would have improved on those results,26,27 but it must be borne in mind that, whether or not it is available, this method requires a second examination and its economic cost is higher. TBNA can be carried out during diagnostic bronchoscopy, which improves diagnosis and staging in a single endoscopic action. Our data call into question the performance of the above-mentioned examinations, in terms of both effectiveness and of patient wellbeing, unless the TBNA has been carried out beforehand, when pathological mediastinal adenopathies have been observed in the thoracic CT scan.
Is Conventional Transbronchial Aspiration Economically Viable?Bearing in mind the added cost which the performance of an aspiration represents, and the saving resulting from the avoidance of additional diagnostic techniques and staging mediastinoscopies, the introduction of TBNA has, in our clinical setting, led to a net saving of 451.57EUR per patient. This result is comparable to the results recorded by other groups.9,10,16
Recently two articles were published offering an economic analysis of different diagnostic strategies in the evaluation of mediastinal tumours in BC; in both cases specialised software was used based on a decision tree.
Harewood et al.28 examined the cost-effectiveness of 7 variants: mediastinoscopy, TBA-USEB, conventional TBNA, TBA-EBUS+PET-EUS, TBNA+PET-EUS, and TBNA+TBNA-EBUS, in the mediastinal staging of patients with non-microcytic carcinoma. They conclude that the combination of TBA-EBUS and PET-EUS is the most economical strategy when there is a high probability of lymph node metastasis, while if it is low PET-EUS is preferable. However, in order to arrive at these results the authors assume 36% sensitivity for the TBNA, a figure which is much lower than that given by other authors, and they also begin with the assumption of 30% prevalence of mediastinal tumour, which differs greatly from what is normally regarded to be the case.29 Furthermore, they assign a cost to TBNA which is only slightly inferior to TBA-EBUS (1430 as opposed to 1711EUR). Steinfort et al.30 compare 4 diagnostic strategies in mediastinal staging of patients with non-microcytic carcinoma and pathological adenopathies in thoracic CT scans or in the PET: PTB-EBUS with histological confirmation of the negative results, TBA-EBUS without histological confirmation of the negative results, conventional TBNA and mediastinoscopy. The final result is that the most cost-effective strategy is TBA-EBUS without histological confirmation of the negative results. However, this work is based on the premise that TBNA is performed during a bronchoscopy intended exclusively for mediastinal staging, and a similar cost is assigned to it as to TBA-EBUS. The result might have been different if it had been assumed that TBNA would be carried out during the diagnostic bronchoscopy, which must necessarily have already been carried out on all patients. Besides, as the same authors show, the cost of the acquisition of the ecobronchoscope has not been factored into the analysis.
Weaknesses and Strengths of the StudyThe main limitation of this paper is that it is a based on a retrospective study. Nevertheless, the fact that the patients suspected of having BC have access to a thoracic CT scan prior to the diagnostic bronchoscope, and that in these patients TBNA was systematically performed, minimises this drawback. Another limitation of the paper, which is one that it has in common with all studies of this kind, consists in the fact that, in view of the high degree of specificity described when the recommended technical principles are applied, the diagnostic results of the TBNA are not confirmed by means of a surgical technique, and are assumed to be true positives. Furthermore, as it is also common to studies of this kind, most of the diagnostic results have not been confirmed by means of mediastinoscopy, either on account of the irresectability of the tumour or the inoperability of the patient. Only operable patients with potentially resectable tumours have been subjected to a mediastinoscopy for confirmation of non-diagnostic results.
The main strength of the study is that it has included a homogeneous, complete, and non-selected group of students, as this is the only centre in our area where patients suspected of having BC are admitted and as we take full responsibility for the entire process with regard to the diagnosis and follow-up of these patients. Furthermore, the fact that most of the bronchoscopies are carried out by the same endoscopist minimises the variations attributable to technical personnel and individual skill.
ConclusionsIn patients with BC and pathological adenopathies in the thoracic CT scan, TBNA is a clinically useful technique, given that it obviates the need for additional staging mediastinoscopies (thus avoiding diagnostic delays and, in the event, mortality). It has also proven to be cost-effective. For this reason, it is our opinion that it should systematically be carried out, as a routine part of the endoscopic process, during diagnostic bronchoscopy of patients suspected, on the basis of clinical and radiological tests, of having BC who subsequently present accessible mediastinal or hilar adenopathies in the thoracic CT.
Financial AidThis study has not received financial assistance of any kind.
Conflict of InterestsThe authors declare the absence of any conflict of interests.
Please cite this article as: Castelao Naval J, et al. Utilidad clínica e impacto económico de la punción transbronquial convencional de adenopatías mediastínicas en el carcinoma broncogénico. Arch Bronconeumol. 2013;49:41–6.