Chylothorax is an uncommon entity associated with various processes that damage or obstruct the thoracic duct (TD) and its tributaries, causing chyle to leak into the pleural space.
Chylothorax can be a result of trauma or other causes. Non-traumatic causes mainly include cancers; most commonly, lymphomas. A more unusual cause is venous thrombosis of the jugular-subclavian junction, which obstructs TD drainage, due to medical or non-surgical traumatic procedures, such as central line placement.
Management is generally conservative, with chest drainage and dietary modifications, including medium-chain triglyceride (MCT) supplements, although TD ligation may be necessary.
We report 2 cases of chylothorax as a complication of chronic thrombosis of the tributary venous TD drainage territory.
Case 1. A 34-year-old woman, with no allergies, diagnosed with ulcerative colitis 11 years previously. She presented with a 2-month history of dyspnea on moderate exertion after an episode of spontaneous venous thrombosis of the left jugular and subclavian veins. Platelet concentrations were normal. Chest radiography revealed right pleural effusion. Thoracocentesis of the fluid was consistent with chylothorax (triglycerides 1349, cholesterol 103). A chest computed tomography (CT) was performed, showing absence of filling of the left subclavian intrathoracic vein, suggesting chronic non-recanalized thrombosis; right pleural effusion and signs of dilation in the lower area of the TD. Phlebography of the left upper limb revealed extensive thrombosis of the subclavian vein, with significant collateral and even contralateral circulation. Jugular veins were not highlighted due to probable thrombosis. A chest tube was placed and parenteral nutrition was started, followed later with a low-fat, MCT-rich diet. The quantity of chyle drained was minimized and the chest tube was removed. The patient continued on a specific diet for 4 weeks, with good progress.
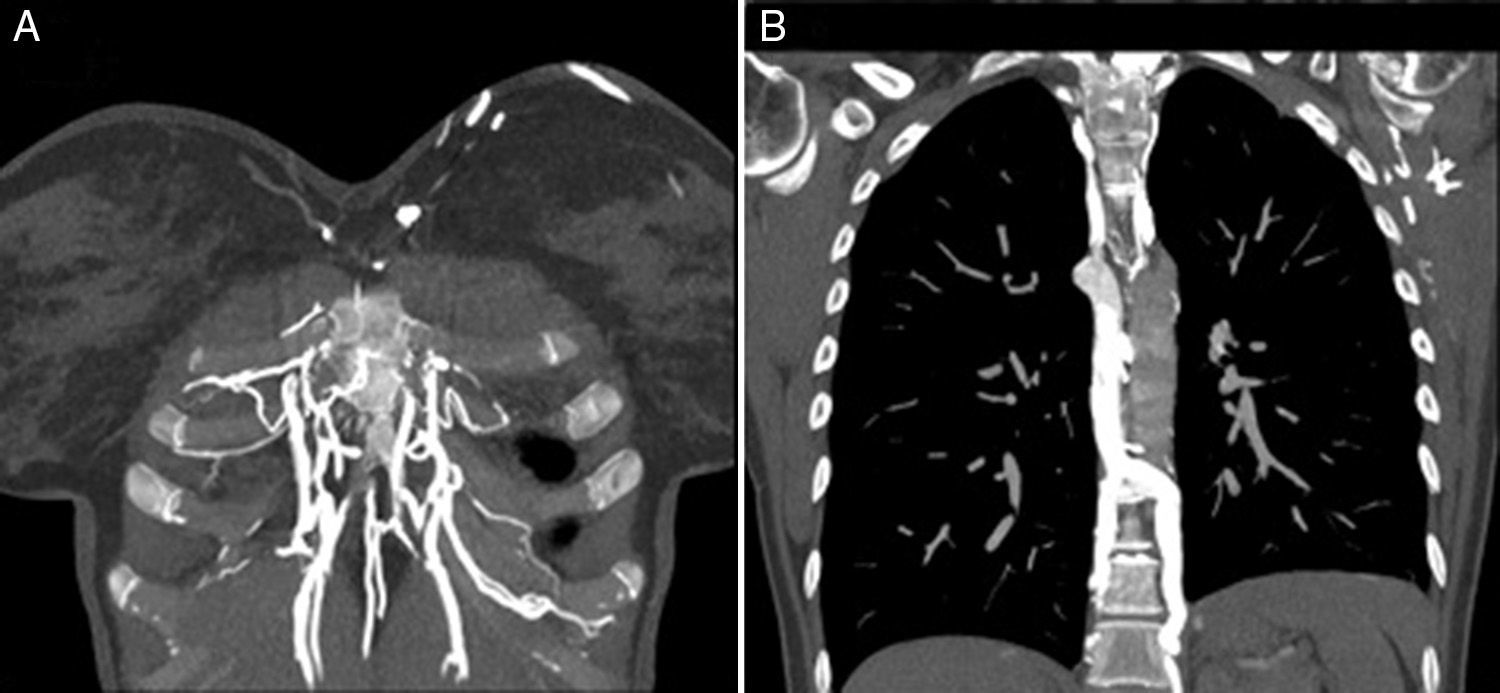
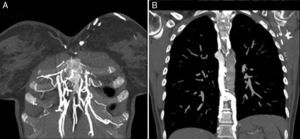
Case 1. A 27-year-old woman, with a 5-year history of acute lymphoblastic leukemia and allogeneic bone marrow transplant with major ABO incompatibility. Overall graft-versus-host disease (GVHD) grade 2 (digestive grade 1, cutaneous grade 1) in remission. She had presented Hickman catheter thrombosis 4 months previously, with bilateral pulmonary thromboembolism (PTE). PTE progress was favorable, but a subsequent venous Doppler revealed echogenic material in the right internal jugular vein, with reduced caliber, associated with chronic venous thrombosis; right subclavian vein with parietal thickening, patent but with weak flow and linear morphology suggesting involvement of the brachiocephalic venous trunk or superior vena cava. On chest CT angiogram: small-caliber superior vena cava, showing filiform contrast medium filling proximal to the arch of the azygos vein, distal to which no contrast medium was observed; the intrathoracic subclavian and innominate veins could not be identified; abundant collateral circulation; bilateral pleural effusion and minimal pericardial effusion, findings consistent with chronic thrombosis of both innominate veins and superior vena cava. Chylothorax was identified by thoracocentesis, and we decided to take a conservative approach, resulting in resolution of pleural and pericardial effusion.
Interruption of drainage in the distal end of the TD as a consequence of venous thrombosis of the jugular-subclavian junction may cause TD rupture and chylothorax. Treatment may be conservative or surgical. Dietary strategies include parenteral nutrition and/or oral MCT supplementation. Conservative management is successful in 40%–90% of cases, while in non-traumatic chylothorax some studies report a success rate of almost 100%.1
In congenital heart disease surgery, post-operative central venous thrombosis is known to be a cause of potentially fatal chylothorax. Treatment with an MCT-rich diet and drainage may be sufficient, but refractory cases may require TD ligation or unblocking of the venous obstruction with angioplasty or stenting.2,3
In both our patients, chylothorax occurred as a complication of deep vein thrombosis. In inflammatory bowel disease (IBD), there is an increased risk of multifactorial thrombotic phenomena: nutritional deficiencies, hospitalization, surgery, and prothrombotic factors.4 Nevertheless, thromboembolic venous disease is an uncommon complication of IBD. Patients with IBD should only receive prophylaxis in some generally agreed situations (admission for medical disease, need for surgery, etc.). Venous thrombosis associated with the use of central venous lines has also been described as a potential cause of chylothorax and chylopericardium,5 and pacemaker implantation may also be exceptionally associated with thrombosis and chylothorax.
Chylothorax has a characteristic appearance, but nevertheless, it should always be suspected if pleural effusion develops after subclavian or jugular vein thrombosis (Fig. 1)
Please cite this article as: Álvarez Vega P, Cadenas Menéndez S, Sánchez Serrano A, Fernández Sánchez JL, Martín Sánchez MJ, López Zubizarreta M. Quilotórax secundarios a trombosis del sistema venoso superior. Arch Bronconeumol. 2017;53:83–84.