Chronic pulmonary aspergillosis (CPA) is a rare disease, frequently affecting patients with current or prior lung disease, leading to the development of air cavities in the middle of lung parenchyma. Chronic cavitary pulmonary aspergillosis (CCPA) is the most common form of CPA, presenting as a single or as multiple pulmonary cavities with thickened walls, with or without an aspergilloma inside. When not treated appropriately, it can progress to chronic fibrosing pulmonary aspergillosis (CFPA), which is characterized by severe fibrotic destruction of at least two lobes of lung, ultimately leading to a major loss of lung function .1
These two forms of CPA, similarly to what happens to single aspergilloma and Aspergillus nodules, usually occur in patients who are not immunosuppressed, differently from what happens in invasive pulmonary aspergillosis. On another hand, subacute invasive aspergillosis (SAIA), previously named chronic necrotizing aspergillosis, contrasts from invasive pulmonary aspergillosis due to its slower progression (usually 1–3 months), befaling in mildly immunocompromised patients and having similar clinical and radiological features to CCPA but a more rapid progression.1
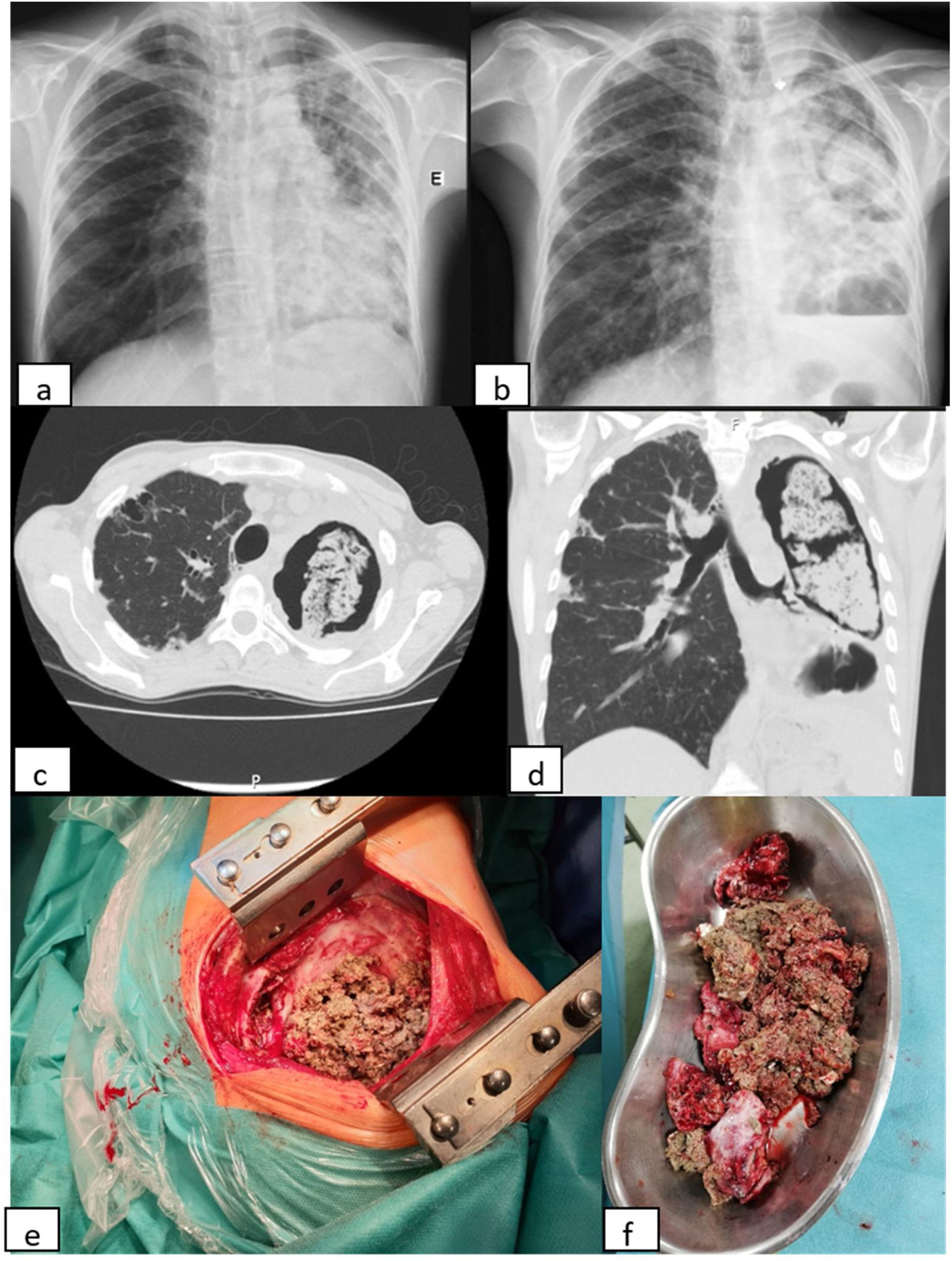
We report the case of a 44-year-old woman with bronchiectasis due to whooping cough in childhood. She was referred to an autoimmune diseases consultation due to a lower limb vasculitis, whose study was negative except for anti-neutrophil cytoplasmic antibodies (ANCAs – atypical pattern) of 1/160. She started steroid therapy in considerable doses in order to control her disease. Chest X-rays demonstrated evolution of previous lung lesions to aspergilloma and a six-month course of itraconazole was prescribed. Despite that, clear worsening of the lesions with complete destruction of the left lung was perceived and the patient was proposed for left pneumectomy. At the surgery, filling of the left pleural cavity with brown necrotic material was observed. Histological exam of the surgical fragments revealed one re-epithelized cavitated lesion associated with fungal structures of the Aspergillus type. The microbiology of the surgical specimen identified Aspergillus fumigatus. Patient status after surgery has improved (Fig. 1).
(a, b) X-ray evolution of the patient. The X-ray on the left (a) was performed before corticosteroids therapy and the one on the right (b) about seven months after the beginning of that therapy; (c, d) coronal and axial views of thoracic computed tomography performed after six months of Itraconazole, showing giant aspergilloma in left lung; (e, f) necrotic material of fungus ball observed during surgery.
This case highlights the multiple forms of CPA. The progression of this patient lesions do not fit the definition of SAIA, but we consider that the new imunossupressive status contributed to a more rapidly progression from CCPA to CFPA.