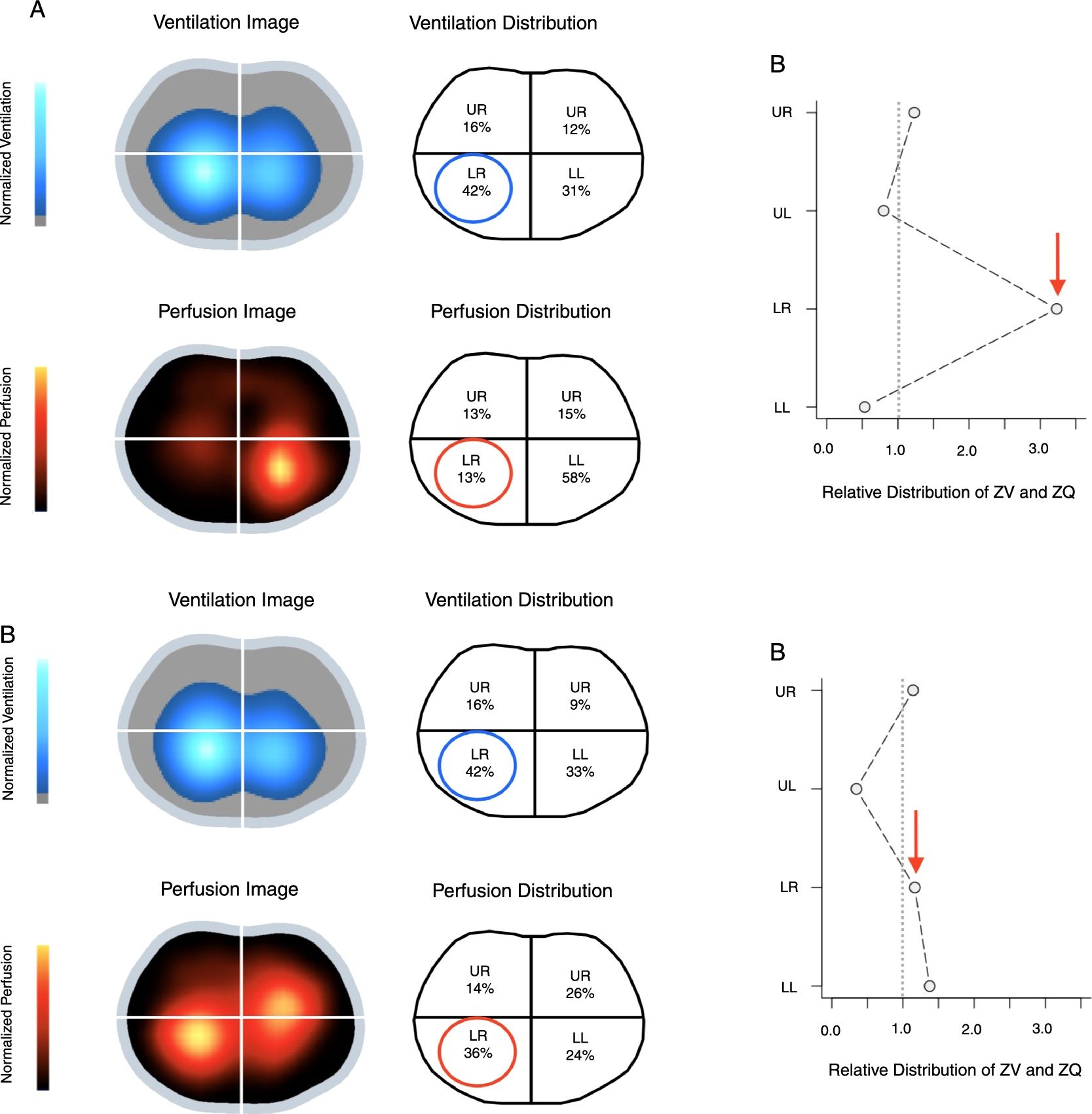
A 59-year-old male was admitted to ICU for subarachnoid and lobar hemorrhage. The patient developed acute respiratory failure secondary to aspiration pneumonia that met criteria for acute respiratory distress syndrome (ARDS) with hemodynamic instability requiring noradrenaline at 0.9μg/kg/min. Despite deep sedation and neuromuscular blockade, the patient remained hypoxemic. In supine position, the patient was ventilated in volume-assisted control with a tidal volume of 7.8ml/kg of predicted body weight and PEEP of 10cm of H2O at 24breaths/min. In this situation, the plateau pressure was 24cm of H2O and the compliance of the respiratory system was 36ml/cm H2O. The ratio between partial pressure of oxygen and the fraction of inspired oxygen (PaO2/FIO2) was 84mmHg. Prone positioning could not be performed due to the increased intracranial pressure. Subsequently, respiratory monitoring was complemented with thoracic electrical impedance tomography (EIT). Surprisingly, it revealed a relatively homogeneous ventilation with decreased perfusion of the right lung (Fig. 1a). In view of these findings, inhaled nitric oxide (iNO) therapy was initiated at 5ppm and increased up to 10ppm. After one hour of iNO therapy at 10ppm, PaO2/FIO2 rose to 128mmHg and was associated with a more homogeneous distribution of perfusion (Fig. 1b) measured by EIT. No adverse effects associated with iNO therapy were observed. This case illustrates that iNO can be considered in selected cases of severe hypoxemia. EIT perfusion analysis is a monitoring tool that may be useful in these clinical situations.
Electrical impedance tomography (EIT) ventilation and perfusion images obtained before (a) and after (b) inhaled nitric oxide therapy at 10ppm. Color scale adjusted by linear normalization. LL: lower left; LR: lower right; UL: upper left; UR: upper right; ZV: ventilation estimated by EIT; ZQ: perfusion estimated by EIT. (a) Baseline: perfusion reduction in the RL lobe with no changes in ventilation. (b) After 1h of iNO therapy at 10ppm: increase in perfusion in the RL lobe with an improvement in the ventilation–perfusion ratio.
The authors would like to thank Dr. Caio Morais for his technical assistance in preparing the figures.