During the last 20 years, there has been a general increase in asthma prevalence1,2 that has affected most countries and become an important public health problem. At the same time, there have been important advances made in our understanding of the physiopathology3,4 and treatment of asthma.5 Among these advances is the establishment of the inflammatory base of the disease, the clinical benefit of anti-inflammatory treatment with inhaled steroids, as well as the potentially harmful effects of the use of short-acting beta 2-agonist bronchodilators.6 Mention should also be made of the widespread diffusion of said advances in the medical community through international guidelines7–9 and the Spanish Guidelines for the Management of Asthma, published some years later.10 Despite the importance of these therapeutic changes and their widespread diffusion, there is little information of how these changes have been implemented in the asthma population of Spain as a whole.
In 1991, the European Community Respiratory Health Survey (ECRHS-I)11 determined asthma treatment patterns in Europe12 as a whole and in Spain13 alone. This latter study analyzed the treatment followed by individuals who were epidemiologically identified as asthmatics and those with physician-diagnosed asthma in the participating regions. The analysis of the ECRHS-I Spanish database demonstrated a high proportion of underdiagnosis and undertreatment as well as improper treatment. Although there are other studies in clinical populations that report the asthma treatment pattern in our country, the ECRHS was the first to provide said information in a general population of young adults. The follow-up of the general population cohort from the ECRHS-I 10 years after the first study offers us the possibility to report, from a historical perspective, the changes that have occurred in the treatment of the asthma population in Spain from 1991 to 2001.
ProcedureThe ECRHS-II14 is a multicenter follow-up study of a population-based cohort of 2649 individuals who participated in the ECRHS-I in 5 Spanish health-care centers (Albacete, Barcelona, Galdakao, Huelva and Oviedo) and who completed, in both studies, the questionnaires about asthma-related symptoms, tobacco habit, treatment and use of health-care resources. The study involved respiratory function testing and taking blood samples for the determination of total IgE and specific IgE. The design, protocol and participation of the Spanish centers in the ECRHS-I and II have already been reported in preceding articles11,14 and at http://www.ecrhs.org. The protocol was approved by each of the ethics committees from each participating center, and each participant gave her/his written informed consent.
Definitions of AsthmaGiven the difficulties inherent in the epidemiological approach to asthma, different approaches were adopted for the diagnosis of asthma. In accordance with the ECRHS protocol, we have defined: (1) Asthma-related symptoms (ARS), if the participant responded affirmatively to any of the following questions: (a) Have you woken at night due to an attack or lack of air at any time in the last 12 months?, (b) Have you had an asthma attack at any time in the last 12 months?, or (c) Have you taken any asthma medication in the last 12 months? (2) Epidemiological diagnosis of asthma (EDA), if the individual admits having asthma-related symptoms in the last 12 months together with the presence of bronchial hyperreactivity.13 (3) Physician-diagnosed asthma (PDA), when the patient answers positively to the questions: Do you have or have you ever had asthma? and, Has it been confirmed by a physician? (4) Does not consider himself/herself asthmatic (asthma underdiagnosis): individuals who, despite presenting symptoms related with asthma in the last 12 months and bronchial hyperreactivity, respond negatively to the question: Do you have or have you ever had asthma?
Definition of AtopyBoth the ECRHS-I11 and ECRHS-II14 analyzed the presence of total IgE and specific IgE in blood using the CAP system by Pharmacia (Pharmacia Diagnostics, Upssala, Sweden). Atopic individuals were considered those who demonstrated specific IgE equal to or greater than 0.35kU/l for, at least, one of the following allergens: (a) Dermatophagoides pteronyssinus, (b) cat epithelium, (c) Phleum pratense, and (d) Cladosporium herbarum.
Bronchial HyperreactivityIn order to evaluate whether the individual presented bronchial hyperreactivity, non-specific bronchial challenge tests with methacholine were used with the same protocol as in the ECRHS-I, as described in earlier studies.11 Individuals with bronchial hyperreactivity were considered those who presented a fall in FEV1 of 20% or higher compared with the best post-saline solution FEV1. The maximum accumulated dose allowed by the protocol was 5.117μmol of inhaled methacholine, or extrapolating to a dose of 8μmol of inhaled methacholine.
Asthma TreatmentThe questions about treatment refer to the previous 12 months and are identical in the ECRHS-I11 and ECRHS-II,14 except for long-acting beta-2 agonists (LABA), which appeared as a new treatment for asthma (2000–2001), simultaneously with the field work for the ECRHS-II, and therefore it was only included in the second study.
In order to compare the treatment data with those of the earlier study,13 we used the following classification, considering these categories exclusive: (1) Absence of treatment: the patient reports following no asthma treatment. (2) Recommended asthma treatment: the participant reports following some of the treatment steps recommended by the Global Initiative for Asthma (GINA).9 In this type of treatment, we have established 3 groups, following the ECRHS-I11: (a) inhaled short-acting beta-2 agonist bronchodilators, used alone, (b) inhaled corticosteroids, without specifying daily dosage, associated or not with other drugs, generally with inhaled LABA bronchodilators, and (c) oral corticosteroids needed at some time, either short-term or as continuous therapy. (3) Treatment not recommended for asthma: the participant reports following treatment with drugs that are not found in any of the steps of the therapeutic guidelines for asthma (mucolytics, cough medicine, antihistamines, etc.).
Statistical AnalysisA descriptive analysis was performed of the sample by calculating frequencies and percentages as well as means and standard deviations (SD). In order to identify the risk factors associated with not realizing that the subject is asthmatic when he/she presents epidemiological diagnosis of asthma, logistic regression models were used (one for each period). The results report the odds ratio (OR) of not realizing that one is asthmatic together with the 95% confidence interval (95% CI).
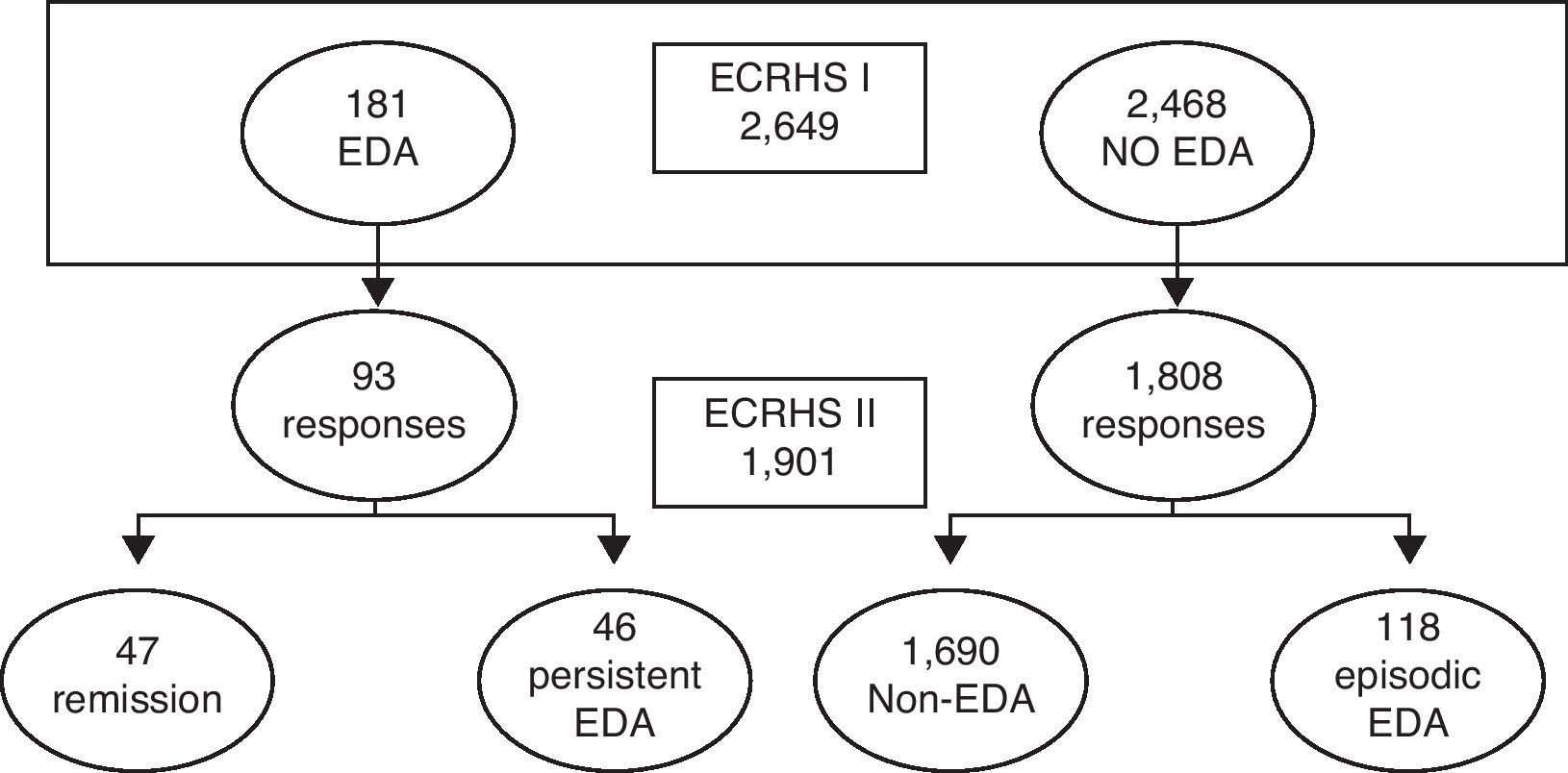
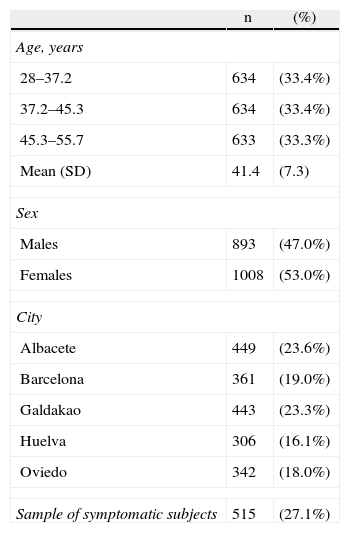
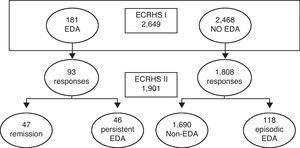
ResultsChanges Observed in the Treatment of Asthma From 1991 to 2001Out of the 2649 individuals who participated in the ECRHS-I11 at the 5 different Spanish centers, information was obtained from 1901 (53% women) 10 years later in the ECRHS-II study,14 with a global response rate of 71.7%. The participants’ ages ranged from 28 to 55 (Fig. 1 and Table 1).
Characteristics of the Study Population Who Participated in Both Analyses (ECRHS-I and ECHRS-II) (n=1901).
| n | (%) | |
| Age, years | ||
| 28–37.2 | 634 | (33.4%) |
| 37.2–45.3 | 634 | (33.4%) |
| 45.3–55.7 | 633 | (33.3%) |
| Mean (SD) | 41.4 | (7.3) |
| Sex | ||
| Males | 893 | (47.0%) |
| Females | 1008 | (53.0%) |
| City | ||
| Albacete | 449 | (23.6%) |
| Barcelona | 361 | (19.0%) |
| Galdakao | 443 | (23.3%) |
| Huelva | 306 | (16.1%) |
| Oviedo | 342 | (18.0%) |
| Sample of symptomatic subjects | 515 | (27.1%) |
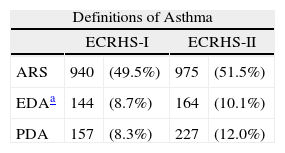
Between the two periods, an increase was detected in the proportion of asthmatics, regardless of the definition of asthma used: both individuals with asthma-related symptoms as well as those with epidemiologic diagnosis of asthma or with physician-diagnosed asthma (Table 2).
Asthma Symptoms and Diagnosis in the Study Populations of the ECRHS-I and ECRHS-II (n=1901), According to the Different Definitions of Asthma.
| Definitions of Asthma | ||||
| ECRHS-I | ECRHS-II | |||
| ARS | 940 | (49.5%) | 975 | (51.5%) |
| EDAa | 144 | (8.7%) | 164 | (10.1%) |
| PDA | 157 | (8.3%) | 227 | (12.0%) |
ARS (asthma-related symptoms): responds affirmatively to one of the following questions: (a) Have you woken at night due to an attack or lack of air at any time in the last 12 months?, (b) Have you had an asthma attack at any time in the last 12 months?, or (c) Have you taken any asthma medication in the last 12 months?.
EDA (epidemiologic diagnosis of asthma): presents ARS as well as bronchial hyperreactivity.
PDA (physician-diagnosed asthma): affirmative response to Do you have or have you ever had asthma? and Has your asthma been confirmed by a physician?.
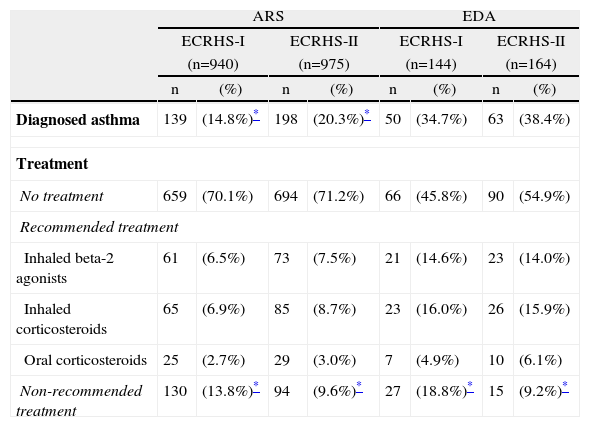
In the groups of individuals who met the definition of asthma-related symptoms, there was an observed significant increase in the number of individuals who had been diagnosed with asthma by a physician (from 14.8% to 20.3%; P<.05) (Table 3). The underdiagnosis of asthma, defined as the presence of epidemiologic diagnosis of asthma without a doctor's diagnosis, was 65.3% and 61.5% in each period, respectively.
Diagnosed Asthma and Treatment Followed by Subjects With Asthma-Related Symptoms (ARS) and With Epidemiologic Diagnosis for Asthma (EDA) in the ECRHS-I and ECRHS-II.
| ARS | EDA | |||||||
| ECRHS-I | ECRHS-II | ECRHS-I | ECRHS-II | |||||
| (n=940) | (n=975) | (n=144) | (n=164) | |||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Diagnosed asthma | 139 | (14.8%)* | 198 | (20.3%)* | 50 | (34.7%) | 63 | (38.4%) |
| Treatment | ||||||||
| No treatment | 659 | (70.1%) | 694 | (71.2%) | 66 | (45.8%) | 90 | (54.9%) |
| Recommended treatment | ||||||||
| Inhaled beta-2 agonists | 61 | (6.5%) | 73 | (7.5%) | 21 | (14.6%) | 23 | (14.0%) |
| Inhaled corticosteroids | 65 | (6.9%) | 85 | (8.7%) | 23 | (16.0%) | 26 | (15.9%) |
| Oral corticosteroids | 25 | (2.7%) | 29 | (3.0%) | 7 | (4.9%) | 10 | (6.1%) |
| Non-recommended treatment | 130 | (13.8%)* | 94 | (9.6%)* | 27 | (18.8%)* | 15 | (9.2%)* |
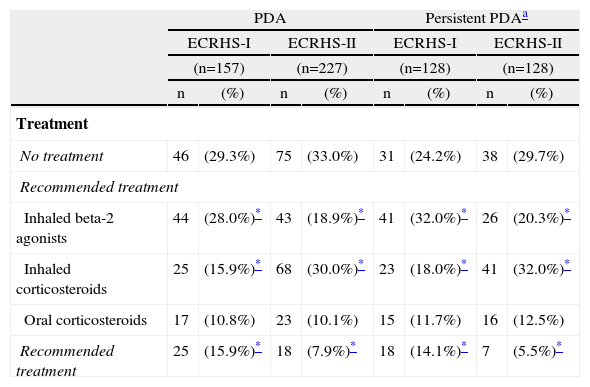
Both among the individuals with asthma-related symptoms and in those with epidemiologic diagnosis of asthma, there was a statistically significant decrease in the proportion of individuals who reported following a treatment that is not recommended for asthma by therapeutic guidelines (Table 3). This is also seen in the group of patients who report physician-diagnosed asthma in both studies (Table 4).
Treatment in Subjects With Physician-Diagnosed Asthma (PDA).
| PDA | Persistent PDAa | |||||||
| ECRHS-I | ECRHS-II | ECRHS-I | ECRHS-II | |||||
| (n=157) | (n=227) | (n=128) | (n=128) | |||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Treatment | ||||||||
| No treatment | 46 | (29.3%) | 75 | (33.0%) | 31 | (24.2%) | 38 | (29.7%) |
| Recommended treatment | ||||||||
| Inhaled beta-2 agonists | 44 | (28.0%)* | 43 | (18.9%)* | 41 | (32.0%)* | 26 | (20.3%)* |
| Inhaled corticosteroids | 25 | (15.9%)* | 68 | (30.0%)* | 23 | (18.0%)* | 41 | (32.0%)* |
| Oral corticosteroids | 17 | (10.8%) | 23 | (10.1%) | 15 | (11.7%) | 16 | (12.5%) |
| Recommended treatment | 25 | (15.9%)* | 18 | (7.9%)* | 18 | (14.1%)* | 7 | (5.5%)* |
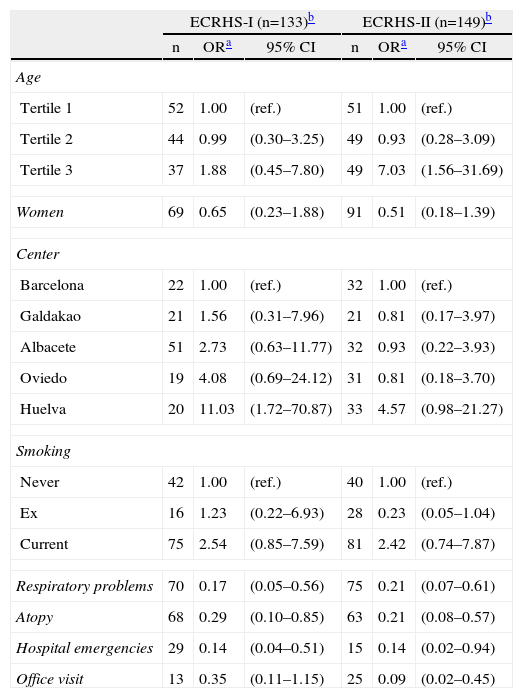
When analyzing the treatment pattern of the individuals who declare physician-diagnosed asthma, relevant changes were observed, such as a significant reduction in the use of inhaled beta 2-agonist bronchodilators, not LABA, as the only treatment. In the ECRHS-II, it was detected that 33 individuals out of the 227 with physician-diagnosed asthma (14.5%) were already being treated with LABA, 27 (81.8%) of whom took them in conjunction with inhaled corticosteroids, while the remainder took them either alone or associated with a short-acting beta-2 adrenergic agonist. 60% of the patients were prescribed LABA in dry powder form, and the rest in metered-dose inhalers. Another notable datum among the individuals with physician-diagnosed asthma was the statistically significant increase in the number of people treated with inhaled corticosteroids, a number which nearly doubled (Table 4). Among the individuals with epidemiologic identification of asthma in the ECRHS-II,14 the probability of not identifying oneself as asthmatic (Table 5) was greater in the group of smokers and in seniors.
Factors Associated With Not Realizing One is Asthmatic in Subjects With Epidemiologic Diagnosis of Asthma (EDA) in ECRHS-I and in ECRHS-II.
| ECRHS-I (n=133)b | ECRHS-II (n=149)b | |||||
| n | ORa | 95% CI | n | ORa | 95% CI | |
| Age | ||||||
| Tertile 1 | 52 | 1.00 | (ref.) | 51 | 1.00 | (ref.) |
| Tertile 2 | 44 | 0.99 | (0.30–3.25) | 49 | 0.93 | (0.28–3.09) |
| Tertile 3 | 37 | 1.88 | (0.45–7.80) | 49 | 7.03 | (1.56–31.69) |
| Women | 69 | 0.65 | (0.23–1.88) | 91 | 0.51 | (0.18–1.39) |
| Center | ||||||
| Barcelona | 22 | 1.00 | (ref.) | 32 | 1.00 | (ref.) |
| Galdakao | 21 | 1.56 | (0.31–7.96) | 21 | 0.81 | (0.17–3.97) |
| Albacete | 51 | 2.73 | (0.63–11.77) | 32 | 0.93 | (0.22–3.93) |
| Oviedo | 19 | 4.08 | (0.69–24.12) | 31 | 0.81 | (0.18–3.70) |
| Huelva | 20 | 11.03 | (1.72–70.87) | 33 | 4.57 | (0.98–21.27) |
| Smoking | ||||||
| Never | 42 | 1.00 | (ref.) | 40 | 1.00 | (ref.) |
| Ex | 16 | 1.23 | (0.22–6.93) | 28 | 0.23 | (0.05–1.04) |
| Current | 75 | 2.54 | (0.85–7.59) | 81 | 2.42 | (0.74–7.87) |
| Respiratory problems | 70 | 0.17 | (0.05–0.56) | 75 | 0.21 | (0.07–0.61) |
| Atopy | 68 | 0.29 | (0.10–0.85) | 63 | 0.21 | (0.08–0.57) |
| Hospital emergencies | 29 | 0.14 | (0.04–0.51) | 15 | 0.14 | (0.02–0.94) |
| Office visit | 13 | 0.35 | (0.11–1.15) | 25 | 0.09 | (0.02–0.45) |
Atopy: an individual was considered atopic when there was a presence of at least one specific IgE ≥0.35kU/l for 4 allergens: Dermatophagoides pteronyssinus, cat, Phleum pratense and Cladosporium herbarum.
Hospital emergencies: Have you been treated in the hospital emergency department due to respiratory problems in the last 12 months?
Office visit: Have you been treated by a primary care physician for your respiratory problems or because you were breathless in the last 12 months? During the last 12 months, have you gone to a specialist for your respiratory problems or because you were breathless?
Age tertiles in ECRHS-I: tertile 1, under the age of 28.6; tertile 2, between the ages of 28.6 and 36.9; tertile 3, over the age of 36.9.
Tertiles according to age in ECRHS-II: tertile 1, under the age of 37.2; tertile 2, between the ages of 37.2 and 45.3; tertile 3, over the age of 45.3.
Few data are available about the treatment of the asthma population in Spain. The comparison of the results from the ECRHS-I and ECRHS-II13 provides a unique opportunity to report the differences in the populational treatment patterns between 1991 and 2001.
The results of our study demonstrate that during the 10 years that transpired between the ECRHS-I11 and ECRHS-II,14 important changes came about in asthma treatment in the participating Spanish centers as a whole. Among these changes, the most notable is the striking increase (almost doubled) in the use of inhaled corticosteroids in the population with physician-diagnosed asthma, with the simultaneous reduced use of inhaled short-acting beta-2 agonist bronchodilators as monotherapy. Likewise, it should be mentioned that there was a decrease in the use of treatments that are not recommended for asthma, regardless of the definition used: those who only presented symptoms, those who presented bronchial hyperreactivity and those with physician-diagnosed asthma. Although this pattern of change coincided with the widespread diffusion of the therapeutic guidelines for asthma in Spain, it also reflects, as shown by Plaza et al.,15 that compliance with these guidelines by medical physicians in our country is low.
Changes in the Use of Inhaled CorticosteroidsIn the 1960s and 1970s, the clinical characterization of asthma with the presence of wheezing16 entailed a therapeutic model based on bronchodilators. At the end of the 1980s, the inflammatory substrate of the disease began to be established17 and there was a change to the therapeutic model based on the use of inhaled corticosteroids as a first-line treatment in persistent bronchial asthma.7 Along the lines of this trend, the results from the ECRHS-I11 showed that in Europe12 and in Spain13 the treatment of asthma in the general population continued to be based on the use of bronchodilators, with scarce inhaled corticosteroid use. As to be expected, the study, done in the same population as the ECRHS-I11 10 years later,14 showed a significant increase in the use of inhaled corticosteroids in the treatment of individuals with physician-diagnosed asthma; meanwhile, in the subjects with epidemiologic diagnosis of asthma, the proportion of inhaled corticosteroid use remained invariable. The latter datum is possibly due to the fact that the therapeutic changes observed in the population with physician-diagnosed asthma are not intense enough to be seen in the population of individuals with epidemiologic identification of asthma, of which only 38.4% report having been diagnosed with asthma by a physician.
Despite the fact that only 32% of people who declared physician-diagnosed asthma in both periods of the ECRHS used inhaled corticosteroids at the time of the ECRHS-II,14 and it therefore may be thought that said percentage reflects low compliance with therapeutic guidelines, this value was actually average when taking into consideration the results from other countries: the highest rates (almost 50% inhaled corticosteroid use) were seen in Belgium, Sweden and the United Kingdom, while the lowest rates (less than 20%) were obtained in Switzerland and Italy.18 Furthermore, it must be pointed out that said proportion, 10 years earlier, in the ECRHS-I was only 18%, so the increase was considerable. The proportion of diagnosed asthmatics who had been prescribed inhaled corticoids in 2001 was slightly higher than the 23% reported in the AIRE study,19 done in the same time period, for the 7 European countries together (including Spain), although in said study the treatment rate referred to the month prior to the interview.
The increased use of inhaled corticosteroids in individuals with physician-diagnosed asthma was similar in the subjects who only reported physician-diagnosed asthma in one of the 2 periods as in those who reported physician-diagnosed in both periods (persistent). These data inform us of the therapeutic changes attributable to prescriptions or the use of medication because they are from subjects with physician-diagnosed asthma in both studies. Contrarily, data from the former group are more difficult to interpret because the asthma pattern had changed between the two periods (in some patients, the asthma could have remitted, while in others it may have appeared for the first time) (Fig. 1 and Table 4).
Reduction in the Use of Short-Acting Inhaled Beta-2 Agonist Bronchodilators as MonotherapyIt is well-known that there has been an excessive use of inhaled short-acting beta-2 agonist bronchodilators in the treatment of asthma, and even deaths have been documented from overdosing on these drugs.20 Obviously, excluding mild intermittent asthma, one of the main objectives of therapeutic guidelines has been to eliminate the use of inhaled short-acting beta-2 agonist bronchodilators, used alone, as the only treatment of asthma. In the ECRHS-II, complementary to what was observed in the case of inhaled corticosteroids, there was a notable reduction in the use of inhaled short-acting beta-2 agonist bronchodilators used as monotherapy in individuals with physician-diagnosed asthma. Another important finding in this group was the presence of the new LABA agonist bronchodilators, like salmeterol and formoterol, and the formulations associated with inhaled corticosteroids. Thus, in the ECRHS-II, which took place at the same time as the appearance on the market of this type of drugs, 14.5% of the individuals were already being treated with LABA, the majority of which was associated with inhaled corticosteroids and administered with dry powder devices. In the ESCASE21 study, posterior to ours, it was detected that 78% of asthmatics followed treatment with imitation betas, either short-acting or LABA, either as monotherapy or combined with inhaled corticosteroids. Coinciding with the period of fieldwork of our study, there were notable changes in Spain in the availability of drugs for asthma treatment, particularly the combinations of salmeterol/fluticasone in 2000 and formoterol/budesonide in 2001. This had an immediate impact on medical prescriptions, as demonstrated by a primary care study done in Madrid in 2005,22 and the results that we present.
Reduction in Non-recommended Treatment for AsthmaAnother relevant aspect in asthma treatment is the persistence of prescriptions other than those that are recommended by international consensus for the treatment of asthma, such as antihistamines, ipratropium bromide, mucolytic agents and cough medicine. The reduction in the use of this type of treatments in the study period is one of the most significant findings of our study, having been seen in persons with asthma symptoms as well as in those who reported having been diagnosed with asthma by a physician. The ASES study,23 carried out in Spain in 1998 and 1999, indicated that there was greater frequency of use of treatments that are not recommended by guidelines among asthma patients treated in primary care than those seen in pulmonology departments. In the current study, it was not possible to evaluate this aspect.
Perception of AsthmaThe ECRHS-I shows that the factors associated with not realizing one is asthmatic were: smoking, not being atopic, not having wheezing, not having been to the ER or not having been hospitalized due to respiratory problems.13 In the present study, by comparing the logistic models of each time period, we observed that the factors associated with not having a perception of being asthmatic continue to be the same. In the 2001 analysis, current or past tobacco consumption was related with increased risk for not realizing one is asthmatic, although it was not significant. The magnitude of risk (OR: 2.54), as well as having found even greater and significant risk in the former study (OR: 3; 95% CI: 1.3–6.8),13 lead us to believe that said risk is real and that the consumption of tobacco is associated with fewer office visits, diagnostic bias (in favor of chronic bronchitis or COPD) or not coming to terms with a well-established diagnosis. Any of these 3 factors would explain the role of smoking in not realizing or admitting that one has asthma. In the study by López-Viña et al.23 that compared the management of asthma among primary care physicians and specialists in Spain, tobacco use was more than double in asthmatics treated in primary care compared with those treated in pulmonology departments, which may contribute even more to not having a perception of being asthmatic and to underdiagnosis.
A new result in this study is the association between older age and not realizing one is asthmatic. This leads us to believe that after a certain age there is a greater tendency toward not attributing symptoms to asthma due to reasons that may be similar to those described in the case of smoking.
Underdiagnosis and UndertreatmentBy comparing the ECRHS-I with ECRHS-II, we have observed an increase in the diagnosis of asthma in persons with asthma-related symptoms, although the increase is paradoxically smaller when considering the population with simultaneous presence of symptoms and bronchial hyperreactivity. This increase correlates with that reported by Urrutia et al.24 in a previous analysis of the same data and that of Chinn et al.25 for the global European study.
With regards to undertreatment, we have observed a slight but statistically significant increase in the proportion of asthmatics who follow treatment recommended by the therapeutic guidelines, both when asthma is defined by symptoms and when adding to the definition the presence of bronchial hyperreactivity, and also in persons who report having been diagnosed with asthma by a physician. Said increase coincides with previous documentation in earlier studies by our group with the same database, both at the Spanish13 and European levels.18
In any event, as for underdiagnosis and undertreatment, we must consider that, in an epidemiologic population-based study that proposed different definitions of asthma, the cases that are detected most are the most frequent, meaning cases with mild intermittent asthma.
Study Limitations and StrengthsThe present study is the only population-based study in Spain that is able to assess the changes in asthma treatment over the course of a decade (1991–2001) in the follow-up of a cohort. Nevertheless, our study presents some limitations that may have influenced the results obtained. One limitation of the population-based study of this pathology is the epidemiological identification of asthma itself, although currently the most accepted definition includes the presence of symptoms related with asthma in the last 12 months and the demonstration of bronchial hyperreactivity. Another exception of the study is the high nonresponse rate, as 51.3% of the people who met the epidemiologic definition of asthma in the ECRHS-I11 did not participate in the ECRHS-II14 (Fig. 1). Although the sample size was adequate for the global analysis of the 5 participating Spanish centers, comparisons cannot be established between cities for the majority of the parameters studied. Likewise, the extrapolation of our results to Spain as a whole could be objectionable. Although the patterns and trends of asthma treatment that we have obtained are coherent with other studies done in the same time period in Spain, we cannot rule out the possibility that the inclusion of other geographical areas may have translated into different results.
ConclusionsThe results of this study give us a perspective of the changes that have taken place over time in the treatment of asthma in the Spanish population of the ECRHS from 1991 to 2001. The most significant differences found were: reduced use of treatment not recommended by the guidelines, decreased use of short-acting inhaled beta-2 adrenergic agonist bronchodilators as monotherapy, the onset and quick implementation of inhaled LABA bronchodilators that are mostly used in formulas associated with inhaled corticosteroids and administered in dry powder devices. The most noticeable change was the increase in the use of inhaled corticosteroids, which nearly got doubled. The aforementioned can be interpreted as a notable improvement in the prescription pattern and use of asthma treatment. Unfortunately, this change has little impact on the overall population with asthma symptoms, which is partially due to the high proportion of undiagnosed asthmatics, the high percentage of unrecognized asthma and the insufficient compliance with therapeutic guidelines.
This all suggests that the populational control of asthma in Spain in 2001 presented important challenges. Another follow-up study currently being done in the same population will be able to assess further changes.
FundingECRHS-I (1991–1993): Ministerio de Sanidad y Consumo FIS (91/0016060/00E-05E, 92/0319, 93/0393), Hospital General Universitario de Albacete, Hospital General Juan Ramón Jiménez, Consejería de Sanidad del Principado de Asturias.
ECRHS-II (1999–2002): European Commission (QLK4-CT-1999-01237), Fondo de Investigaciones Sanitarias (FIS) (97/0035-01, 99/0034-01 and 99/0034-02), Complejo Hospitalario Universitario de Albacete, Consejería de Sanidad, SEPAR, NIH (R01 HL62633-01), CIRIT (1999SGR 00241), Red Respira ISCIII, Departamento de Salud del Gobierno Vasco.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Martínez-Moratalla J, et al. Cambios en el tratamiento del asma en la cohorte española del European Community Respiratory Health Survey (ECRHS) en el período 1991-2001. Perspectiva del tiempo. Arch Bronconeumol. 2013;49:113–8.