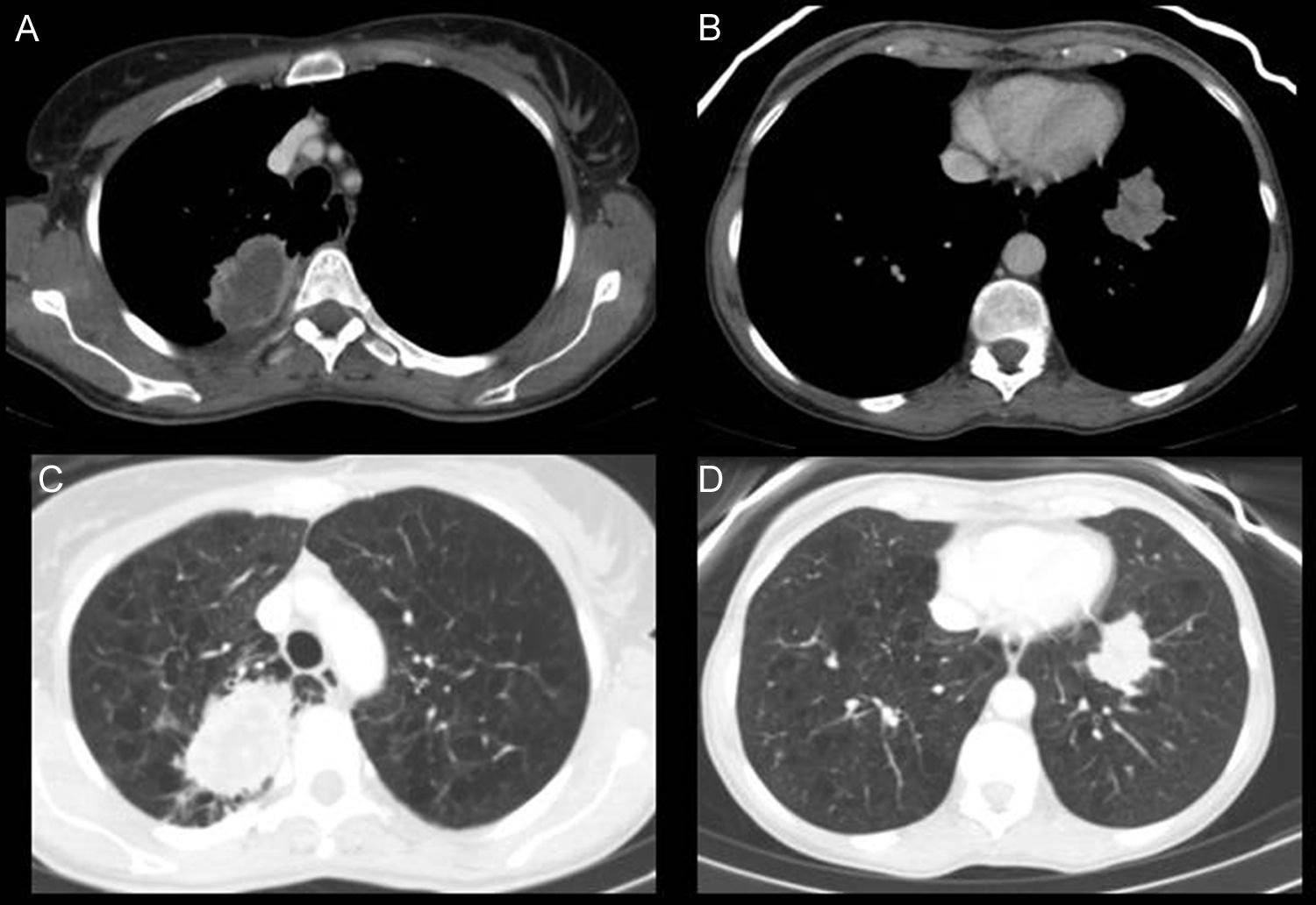
A 57-year-old woman, former smoker, consulted due to irritative cough. Chest radiograph showed a right paratracheal mass and a nodule in the left lower lobe (LLL) with characteristics of malignancy. CT revealed a solid, necrotized mass with peripheral enhancement in the right upper lobe (RUL) (Fig. 1A and C), and another similar subpleural lesion in the LLL (Fig. 1B and D), and pathologically enlarged hilar lymph nodes. All lesions were observed on PET.
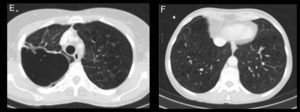
(A and C) Axial CT slices in the mediastinal and lung windows, respectively. A solid mass 6cm×4cm with infiltrative margins, containing necrosis, and peripheral enhancement in the posterior segment of the RUL adjacent to the posterior pleura. (B and D) Axial CT slices in the mediastinal and lung windows. Another solid lesion is seen in the LLL, adjacent to the diaphragmatic pleura, with infiltrative contours and less necrosis. (E and F) Axial CT slices in lung window, 6 months after starting bevacizumab treatment. In E, the RUL lesion can be seen to be larger, cavitated and with no solid component, and in F, the solid tumor in the LLL is smaller with lower attenuation than in images B and D.
FNAB was performed in both lesions, and the pathology report found EGFR-mutation negative and ALK-mutation negative lung adenocarcinoma. Treatment was started with taxol–carboplatin–bevacizumab (antiangiogenic), followed by maintenance bevacizumab.
In the follow-up CT, the RUL lesion had increased in size, with cavitation and reduced solid component (Fig. 1E). The LLL tumor and lymphadenopathy had reduced in size and attenuation (Fig. 1F).
There have been far-reaching changes in the treatment of advanced lung cancer, with the introduction of molecular targets, and immunological and antiangiogenic therapy that have different mechanisms of action and patterns of response from those of conventional chemotherapy. The effects of antiangiogenics include not only change in size, but also the appearance of cavitation (20%), considered a criterion for good treatment response. Although the overall size of the lesions increases, cavitation and reduced solid component are considered a positive response.1
Please cite this article as: Fernández-Rodríguez L, Linares-Beltrán A, Torres-Sánchez, I. Cavitación de adenocarcinoma de pulmón como respuesta al tratamiento con bevacizumab. Arch Bronconeumol. 2016;52:531–532.