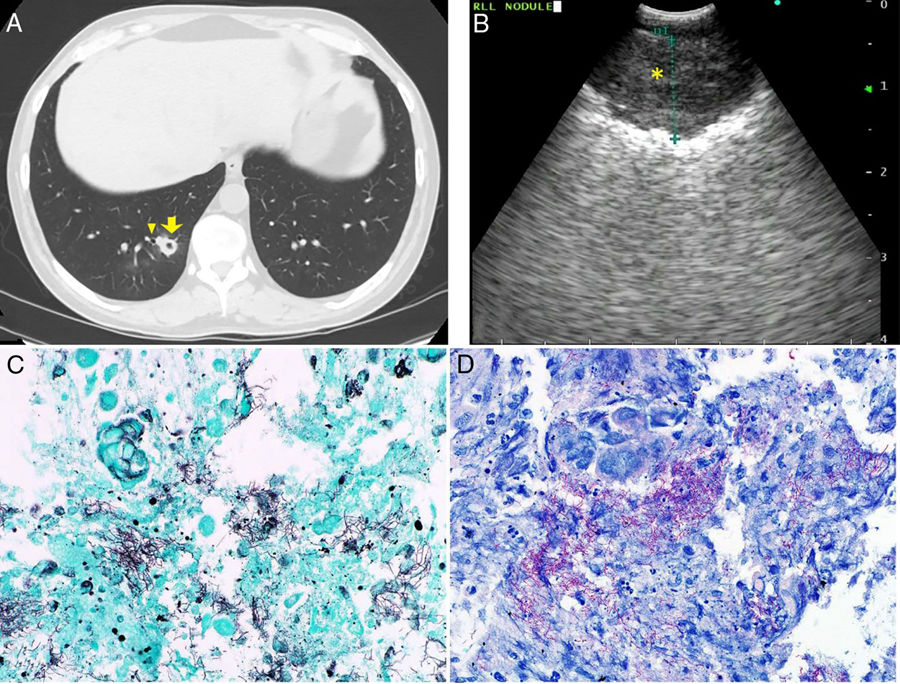
A middle-aged man with chronic lymphocytic leukemia status post hematopoietic stem cell transplantation (day 210) was admitted with diarrhea. His clinical course was complicated with skin and gastrointestinal (grade IV) graft-versus-host disease. He was maintained on antimicrobial (valacyclovir, levofloxacin, atovaquone, isavuconazonium) and immunosuppressive therapy (tacrolimus, methylprednisolone, sirolimus, ruxolitinib, vedolizumab, extracorporeal photopheresis). He developed a dry cough, and a computed tomograpy (CT) scan of the chest revealed 2 cavitary opacities (Fig. 1A). Cavitary lesions were thick walled and located in the right lower lobe and left upper lobe without associated parenchymal lesions. Given its proximity to the airway, in addition to a bronchoalveolar lavage (BAL), convex-probe-endobronchial ultrasound (c-EBUS) guided transbronchial needle aspiration (TBNA) (Fig. 1B) was performed. Cytology revealed gram-positive filamentous branching rods later on identified as Nocardia kruczakiae (Fig. 1C & D). Additional anti-bacterial therapy was initiated. Unfortunately, clinical course was complicated by gastrointestinal bleeding, and he passed away 2 months later.
(A) Computed tomography of chest reveals new cavitary nodules in the right lower lung. The right lower lung cavitary lesion (yellow arrow) is adjacent to a bronchus (yellow carrot). (B) Convex-probe endobronchial ultrasound image of thickened cavitary wall (yellow asterisk) of right lower lobe opacity. (C) Gomori Methenamine-Silver nitrate statin (A, 600×) highlights the branching gram-positive filamentous organisms. (D) Nocardia is weakly acid-fast, and FITE (B, 600×) stain, which is a modified acid fast stain, is positive with the branching filamentous organism.
Nocardia is an opportunistic gram-positive organism notorious for its ability to invade any organ, and lungs and the central nervous system are frequently affected.1 Inhalation is the typical route of infection, but inoculation and transmission from the gastrointestinal tract are also reported. Pulmonary nocardiosis occurs most frequently in immunocompromised patients, and risk factors include diabetes, organ transplantation, use of steroids and calcineurin inhibitor.2 Radiographic presentation may vary and includes consolidation, nodules, cavities and masses, and these are typically mistaken for fungal infection or malignancy.1 In our case, BAL and EBUS-TBNA confirmed Nocardia, and cytology facilitated prompt diagnosis. In those with acceptable hematologic parameters and accessible lesions, EBUS-TBNA may be a helpful adjunct to BAL as a diagnostic tool.
Author contributionsBP, AS, SAF: conception and design, acquisition of radiological and pathological data, drafting the article, critical revision of intellectual content and final approval of the version to be published
FundingThis research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant (CA016672).
Conflicts of interestThe authors declare that no conflicts of interest exist