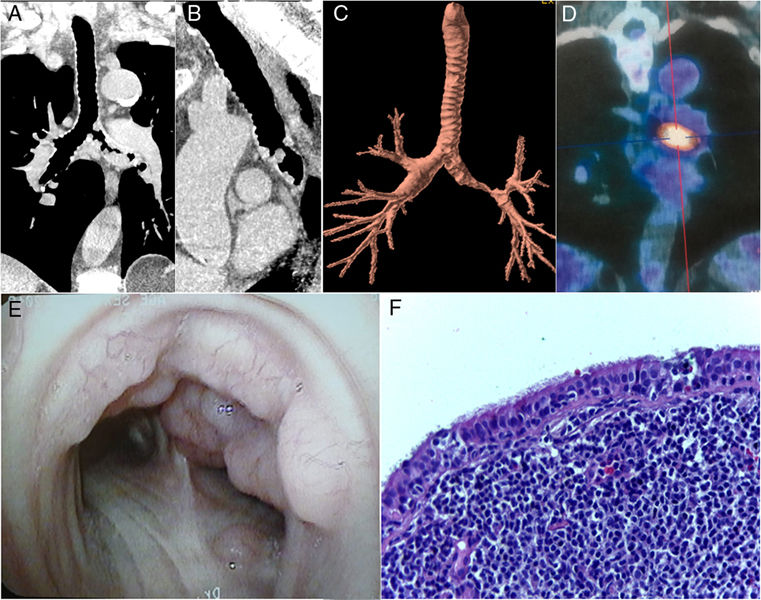
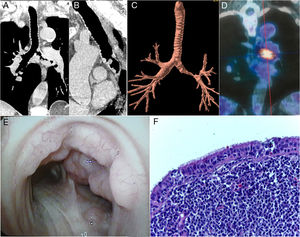
A 72-year-old man presented with a 1-year history of progressive dyspnea. Chest radiography findings were normal. Chest computed tomography showed nodular lesions in the trachea and left main bronchus, with irregular luminal narrowing and severe stenosis (Fig. 1A–C). Pulmonary function testing revealed a variable intrathoracic obstruction. 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography showed increased FDG uptake in the left main bronchus, with a maximum standard uptake value of 8.4 (Fig. 1D). Fiberoptic bronchoscopy revealed multiple small mucosal lesions along the trachea and left main bronchus (Fig. 1E). Histopathology showed proliferation of atypical small lymphoid cells infiltrating the bronchial mucosa and submucosa (Fig. 1F). Immunohistochemical staining supported the diagnosis of extranodal marginal-zone mucosa-associated lymphoid tissue (MALT) lymphoma. The patient was referred for radiotherapy.
Coronal (A) and sagittal (B) reformatted images and a three-dimensional external rendering (C) of a chest computed tomography image show nodular lesions in the trachea and left main bronchus, with irregular luminal narrowing and severe stenosis. (D) 18F-fluorodeoxyglucose positron emission tomography/computed tomography demonstrated increased fluorodeoxyglucose uptake in the left main bronchus, with a maximum standard uptake value of 8.4. (E) Fiberoptic bronchoscopy revealed multiple small nodular mucosal lesions with a cobblestone appearance along the trachea and left main bronchus. (F) A histopathological section demonstrating the proliferation of atypical small lymphoid cells, compatible with lymphoma (hematoxylin and eosin stain, 100× magnification).
MALT refers to the lymphoid tissue underlying the epithelia of the gastrointestinal, respiratory, and urogenital tracts. MALT related to the respiratory tract epithelia is called bronchus-associated lymphoid tissue. MALT lymphoma comprises a group of low-grade extranodal B-cell neoplasms. These tumors arising in the bronchial or tracheal wall are extremely rare. The treatment strategy for this condition has not been completely elucidated, and surgery, radiotherapy, or chemotherapy has been used, alone or in combination.1,2
Conflicts of interestThe authors declare that they have no conflicts of interest to express.