Pneumothorax (PTX) occurs when gas accumulates in the pleural space, it is a common complication of neonatal pulmonary disease and leads to a considerable increase in neonatal mortality. The early and accurate diagnosis followed by correct treatment is imperative to improving the prognosis of patients with PTX.
Lung ultrasonography (LUS) has been successfully used to diagnose PTX. Generally, LUS is used to diagnose PTX on the basis of the following ultrasound characteristics1,2: (1) the disappearance of lung sliding; (2) the absence of B-lines; (3) the presence of pleural lines and A-lines; (4) sandy beach signs are replaced by stratosphere signs on M-mode imaging; and (5) the presence of lung points in mild to moderate PTX. The aim of this study was to investigate the new signs using LUS to diagnose neonatal pneumothorax and the feasibility of pleural puncture under the guidance of those signs.
The study protocol was approved by the ethics committee of the Beijing Chaoyang District Maternal and Child Healthcare Hospital (No. 2011-LC-Ped-01). All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from the participants’ parents. Since 2017, 48 patients have been diagnosed with PTX were included in this study. To determine the value of cardiac ultrasound image disappearance (CUID) in the precordial area in the diagnosis of PTX, we conducted a retrospective case–control study with a ratio of 1:1:1 (PTX (case)/control/case–control). The patient's gestational age (GA), sex, and age at admission were selected as matching conditions to minimize bias between subgroups. The case–control group also included the subgroups of respiratory distress syndrome (RDS),3,4 transient tachypnea of the newborn (TTN),3,5 meconium aspiration syndrome (MAS),3,6 and pneumonia.3,7 In each subgroup, the number of cases was also selected at a 1:1 ratio to minimize statistical error. Thus, 288 newborns were included in this retrospective study. All LUS examinations were performed by well-trained neonatologists or ultrasonologists.
Thoracentesis was performed in accordance with the guidelines in patients with PTX,1 that is, the selection of puncture sites followed the following principles: the intercostal spaces where lung sliding is absent on real-time ultrasound, or the intercostal spaces where LUS presented as a “bamboo sign” on B-mode ultrasound, or the intercostal spaces where LUS presented as a “stratosphere sign” on M-mode ultrasound,1 If thoracentesis at the above puncture points is ineffective or there is still too much gas in the precardiac area after the puncture, it is necessary to perform the puncture in the precardiac area under LUS monitoring.
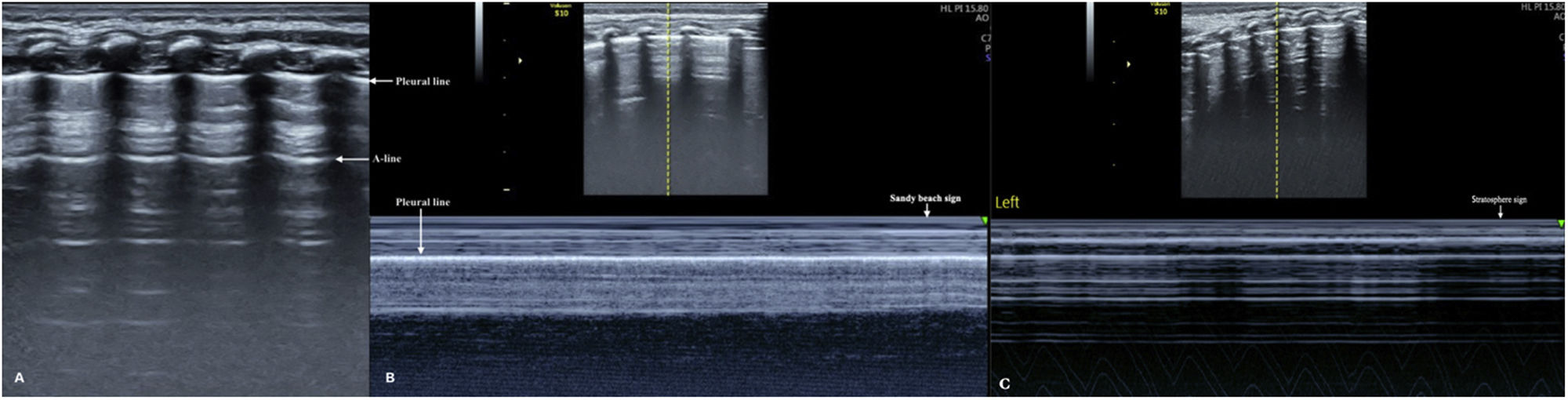
The neonatal normal lung showed a bamboo sign on B-mode LUS and a sandy beach sign on M-mode LUS (Fig. 1A & B). Lung sliding was clearly evident on real-time LUS. Additionally, the heart and cardiac movement in the left precardiac area were visible.
Normal lung ultrasound manifestations. The healthy lung shows a bamboo sign on B-mode ultrasound (A) and a seashore sign (B) on M-mode ultrasound. If the lung sliding disappears on real-time ultrasound, the series of horizontal parallel lines can be seen on M-mode ultrasound; this is the so-called stratosphere sign, which is the specific sign of PTX on M-mode ultrasound (C).
The major LUS manifestations of PTX included the disappearance of lung sliding on real-time LUS (100% of PTX patients). There was an absence of B-lines in 46 patients with PTX (that is, two (4.2%) patients had B-lines). We observed pleural and A-lines in all patients with PTX. Lung point was observed in 31(65%) patients with mild or moderate PTX. Spared areas were observed in 12 (25%) PTX patients, and stratosphere signs were observed in all of the PTX patients (Fig. 1C). CUID in the precordial area was found in eight (16.7%) PTX patients (Video 1).
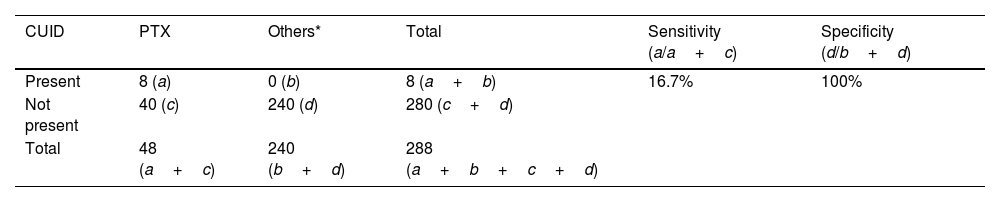
The ultrasound signs of pleural lines and A-lines, the presence of lung point, the disappearance of lung sliding, and the stratosphere sign were only observed in patients with PTX. These signs have been reported in previous studies and are well known,1,8–11 and only CUID has not been previously reported. Therefore, CUID was used as a parameter to calculate the sensitivity and specificity of LUS in diagnosing neonatal PTX. We found that CUID in the precordial area showed a sensitivity of 16.7% and a specificity of 100% for diagnosing neonatal PTX (Table 1).
The sensitivity and specificity of cardiac ultrasound image disappearance for diagnosing pneumothorax.
| CUID | PTX | Others* | Total | Sensitivity (a/a+c) | Specificity (d/b+d) |
|---|---|---|---|---|---|
| Present | 8 (a) | 0 (b) | 8 (a+b) | 16.7% | 100% |
| Not present | 40 (c) | 240 (d) | 280 (c+d) | ||
| Total | 48 (a+c) | 240 (b+d) | 288 (a+b+c+d) |
Note: Others: include TTN (transient tachypnea of the newborn), RDS (respiratory distress syndrome), MAS (meconium aspiration syndrome), pneumonia and normal lungs. CUID: cardiac ultrasound image disappearance.
Among the 48 patients with PTX, needle aspiration was performed in 42 (87.5%) patients with clinical symptoms under LUS monitoring. The gas was completely removed after puncture in 40 (95.2%) patients, with a total drainage gas volume of 55–520mL. The remaining two patients underwent closed thoracic drainage for 1–3 days. The other six patients with mild PTX did not require thoracentesis, and the gas was absorbed spontaneously within 24–68h.
The puncture site was at the second intercostal space of the left or right midclavicular line (the traditional puncture site) in 14 PTX patients. The puncture site was at the fifth to sixth intercostal space of the left or right midaxillary line in 12 patients, and at the seventh to eighth intercostal space of the left or right subscapular line in eight patients. The puncture site was at the precardiac area in eight patients. Among these patients, the puncture site was at the sixth intercostal space of the left midclavicular line in five patients and at 1cm medial to the fifth intercostal space of the left midclavicular line in three patients. No infant died and no puncture complications occurred in this study.
This study is the first to report that CUID in the precordial area is an unusual but specific new sign for diagnosing PTX using LUS. In the present study, CUID in the precordial area was observed in 16.7% of patients with PTX, while it was not observed in patients with TTN, RDS, MAS, pneumonia, or healthy lungs. Therefore, we believe that CUID in the precordial area is a specific LUS sign of neonatal PTX. The sensitivity and specificity of CUID in the precordial area were 16.7% and 100%, respectively (Table 1). Therefore, although this sign is uncommon, it is specific for PTX, and thus, could contribute to avoiding missing the diagnosis of PTX. The possibility of PTX should be considered if this sign is found during a lung ultrasound examination.
In previous studies, PTX was excluded when B-lines were present.1,8,9 However, this study showed that there were B-lines in two PTX patients, but they were also accompanied by CUID in the precordial area (Video 1). Therefore, caution should be exercised when B-lines are detected during an LUS examination at the anterior chest. Our finding suggests that if there is a B-line in the precardiac area, sonographers should search for a cardiac image. We believe that PTX may be excluded if cardiac imaging is present, and conversely, PTX may be present if the cardiac image disappears.
Originally, the most commonly selected puncture site for the treatment of PTX based on chest X-ray (CXR) used to be the second intercostal space in the midclavicular line. However, thoracic puncture under LUS completely changed the traditional methods.1 The results of this study suggest that, in patients with CUID in the precordial area, the precardiac area can also be selected as the puncture site when thoracentesis at the other puncture points is ineffective or there is still significant in the precardiac area after the puncture. Eight patients underwent puncture at this area, including five who had puncture at the sixth intercostal space of the left midclavicular line and three who had puncture at 1cm medial to the fifth intercostal space of the left midclavicular line. To the best of our knowledge, this is the first report to use the precardiac area as the puncture site for the treatment of neonatal PTX. Performing pleural puncture in this area to treat PTX would not have been possible before LUS was developed.
The major limitation of this study is that LUS examinations should be performed by well-trained doctors. Results that are obtained by less experienced examiners may not be reliable. For the thoracentesis, when the precardiac area is chosen as the puncture site, success is dependent on the operator's experience.
In conclusion, this study performed an in-depth investigation of the LUS characteristics of neonatal PTX and treatment under LUS monitoring. We found that CUID in the precordial area is a specific ultrasound sign that could be used to diagnose neonatal PTX. Moreover, in the treatment of neonatal PTX with signs of CUID, selecting the anterior cardiac region as the puncture site under ultrasound monitoring may be feasible.
Institutional review board statementThe study was conducted in accordance with the Declaration of Helsinki, and approved by the ethics committee of Beijing Chaoyang District Maternal and Child Healthcare Hospital (No. 2011-LC-Ped-01).
FundingThis work was supported by a grant from the Social Development Projects, Beijing Chaoyang District Bureau of Science, Technology and Information (SYSF1820, CYSF1922).
Conflict of interestThe authors declare that there are no conflicts of interest.
The following are the supplementary data to this article: