Aspergillus tracheobronchitis comprises less than 7% of pulmonary aspergillosis cases.1 It occurs most frequently in immunocompromised hosts and rarely in immunocompetent individuals. The clinical manifestations of this infection are usually nonspecific, and include cough, exertional dyspnoea, white or purulent sputum, fever and wheezing.1
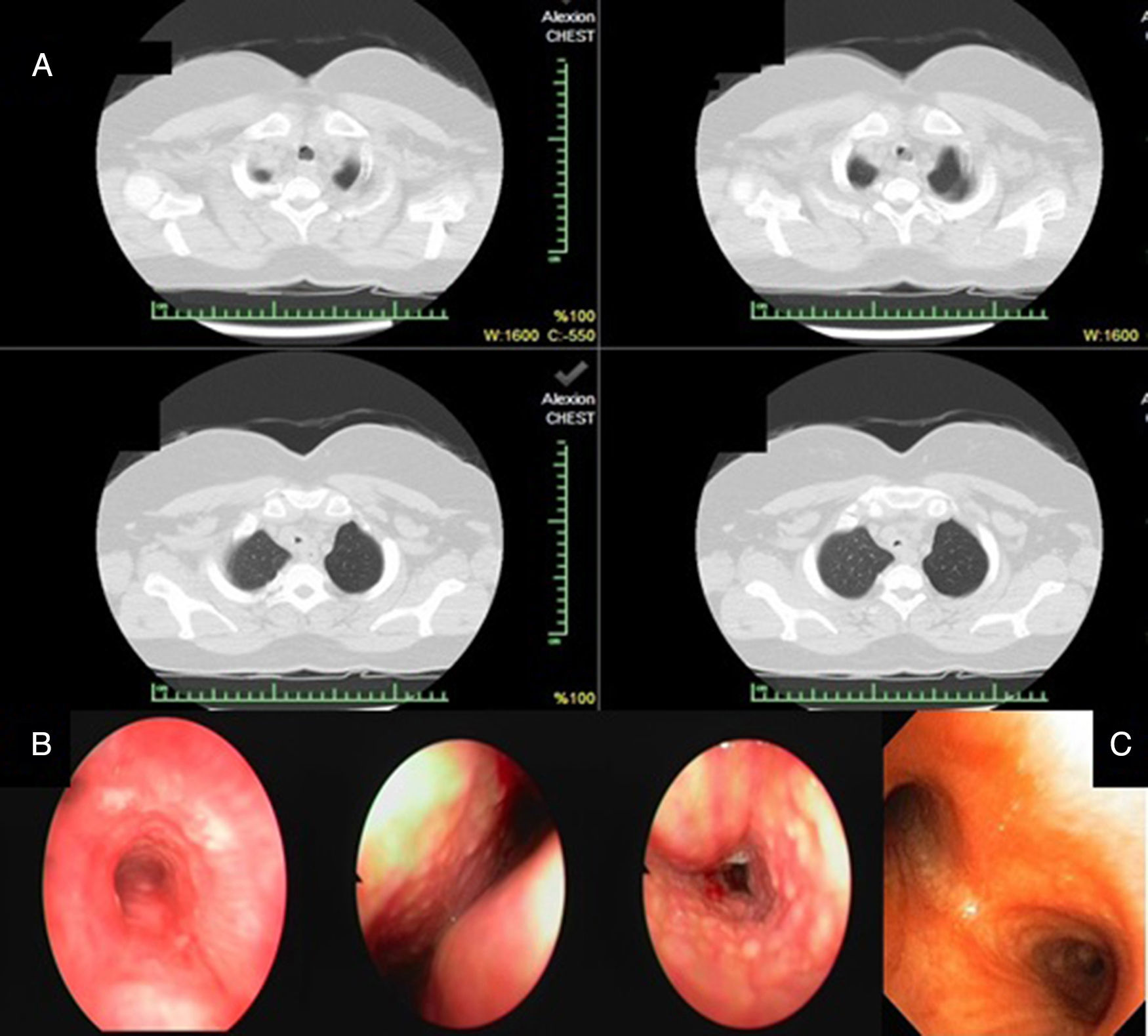
A 54-year-old female who had been suffering from allergic symptoms (sneezing, red eye, rhinitis, unproductive cough, chest discomfort and dyspnoea) for 6 months was admitted to our hospital. Inhaled steroids and antibiotic therapy were initiated due to suspicion of asthma and community-acquired pneumonia; however, her symptoms worsened. To identify the underlying pathology, thorax computed tomography (CT) was performed, and plaques in the trachea and main bronchus were detected (Fig. 1A). A rigid bronchoscopy was planned to ensure a patent airway and evaluate the bronchial system because of her respiratory symptoms and the diffuse plaques and airway obstruction observed on thorax CT. Mucoid impaction and numerous gelatinous whitish plaques along the trachea and the right and left main bronchi were observed (Fig. 1B). Pathological evaluation of the biopsy material taken from the main bronchi and trachea revealed chronic inflammation and fungal hyphae. A fungal culture yielded no growth. Although the pathology was not confirmed, we made a presumptive diagnosis of bronchocentric granulomatosis and Aspergillus tracheobronchitis based on her symptoms, discriminative bronchoscopic findings and unresponsiveness to antibiotics. Differential diagnosis was performed as the pathology was negative for cancer, lavage was negative for Mycobacterium tuberculosis and serum was negative for anti-neutrophilic cytoplasmic antibodies (ANCA). The patient was started on oral prednisolone due to her respiratory symptoms and tracheal lesions. Prednisolone was tapered after 7 days as the cough and dyspnoea had resolved. Galactomannan levels were measured twice at a 1-week interval, and were 0.21 and 0.29ng/ml; these are lower than the 0.5ng/ml reference value and so were accepted as negative. None of the specimens obtained yielded fungal growth. After 1 month of treatment, surveillance bronchoscopic examination revealed significant improvement in the gelatinous whitish plaques in the trachea and main bronchi (Fig. 1C). At the beginning of the treatment, her respiratory function was as follows: FEV1 1.15 (51.8%), FVC 1.87 (71.6%) and FEV1/FVC 59%. These values improved after treatment to FEV 1.85 (84%), FVC 2.40 (83.8%) and FEV1/FVC 76.2%. Prednisolone was stopped and the patient has been followed up for 1 year without treatment.
(A) Plaques in the trachea by thorax computed tomography. (B) Mucoid impaction and gelatinous whitish plaques along the trachea and the right and left main bronchus were observed by rigid bronchoscopy. (C) Surveillance bronchoscopic examination revealed a significant improvement in symptoms.
By definition, bronchocentric granulomatosis is an abnormal cell-mediated response to Aspergillus. A diagnosis of tracheobronchial aspergillosis can be made when tissue histopathology shows hyphae, with or without a positive culture for Aspergillus from the same site. Aspergillus hyphae are identified in 40%–50% of cases.2Aspergillus tracheobronchitis is diagnosed by one of the following: histologic evidence of tissue invasion by Aspergillus in a biopsy, histology suggestive of aspergillosis associated with positive culture of Aspergillus, clinical and radiological findings strongly suggestive of aspergillosis associated with microbiologic identification in lavage fluid, or a positive galactomannan serum assay.1 A background inquiry revealed that the patient had moved to a new house and received a large quantity of flowers before the onset of her symptoms. Because the patient was not immunocompromised, a diagnosis of fungal tracheobronchitis was not initially considered; this delayed the diagnosis by 6 months, which is in agreement with the literature.3 In immunocompetent patients, we consider Aspergillus tracheobronchitis in the presence of numerous gelatinous whitish plaques in the trachea and right and left bronchi. In this case, the earliest indication of an Aspergillus infection was mucoid impaction along the bronchus. Although hyphae were seen in the biopsy, fungal cultures of sputum and respiratory secretions were negative, and no galactomannan positivity was identified. Mucoid impaction and bronchocentric granulomatosis are seen in half of ABPA cases.4 After failing to identify an alternative cause, we interpreted bronchocentric granulomatosis in this patient as a histopathologic manifestation of fungal hypersensitivity.4
Cases of bronchocentric granulomatosis are classified according to the clinical presentation. The first subtype includes asthma and atopy, while the second subtype is idiopathic; some case reports suggest an association with other underlying diseases such as bronchogenic carcinoma, post-radiation pulmonary fibrosis, rheumatoid arthritis, and granulomatosis with poliangeitis.4 Patients with the first subtype tend to be younger (20–40 years), while non-asthmatic patients tend to be older (30–70 years). In our case, atopy was the only co-morbidity.4 Corticosteroids are effective mainly in patients with asthma and atopy.5,6 Corticosteroid therapy was effective in our patient, and resolved all symptoms.
In conclusion, bronchocentric granulomatosis caused by Aspergillus tracheobronchitis should be considered in immunocompetent patients with tracheobronchial infiltrates on CT scan who do not respond to inhaled steroids or broad-spectrum antibiotics. Our patient yielded negative cultures and normal galactomannan values, but tracheal involvement was suggestive of Aspergillosis tracheobronchitis, and hyphae without tissue or vascular invasion were identified in a biopsy. Therefore, recovery of fungal hyphae in a biopsy specimen from an immunocompetent patient with atypical respiratory symptoms and CT findings should not be dismissed as contamination.