Although lung cancer is the second most common cause of mortality due to cancer in young adults, it is an entity that is rarely taken into consideration in young individuals with respiratory diseases.1–4
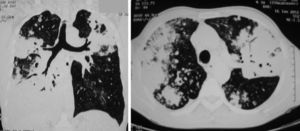
We present the case of a previously healthy 35-year-old smoker (35 packs/year). In October 2011, he was admitted to the local hospital in the Tulcea district (Romania) due to a two-week history of chest pain, cough and fatigue; he was afebrile and had not lost weight. The patient's general poor health was evident on physical examination. Pulmonary auscultation revealed general hypoventilation with scattered rhonchi. Examination of other organs did not yield any findings of interest. Laboratory tests revealed the following: mild inflammatory syndrome, repeated negative sputum examinations and negative ELISA HIV antibody test. The chest X-ray showed patchy consolidation with air bronchogram. A diagnosis of bacterial pneumonia was established, and broad spectrum antibiotic treatment was administered (cephalosporin followed by levofloxacin). After two weeks, corticosteroids were added, with a slight but brief improvement in symptoms. Four weeks after admission, since the patient's condition worsened, anti-tuberculosis treatment was initiated, without first obtaining bacteriological tests. The patient's condition continued to deteriorate, the chest pain increased and major dyspnoea appeared, so in December 2011 he was transferred to a regional hospital, where he underwent a chest computed tomography (CT) scan. The chest CT images revealed patchy consolidation with air bronchogram (Fig. 1). For the first time, possible lung carcinoma was suspected. The patient was transferred to the National Respiratory Medicine Institute in January 2012 for confirmation by bronchial biopsy. At the centre we tried to perform a bronchoscopy, but it could not be done due to severe respiratory failure during the anaesthesia; the patient was transferred to the intensive care unit, where he died six days later. Histopathological examination showed the presence of bronchioloalveolar carcinoma.
The special feature of this case of bronchioloalveolar carcinoma is the fact that the patient only experienced symptoms in the final stage of the disease. Furthermore, the histopathological tumour type is uncommon in male patients, among whom a higher incidence of small cell lung cancer is documented.1–4 In young adults, pneumonia is the most common cause of dyspnoea, but the absence of clinical characteristics of the entity (fever with cough and purulent sputum) should point towards another diagnosis early on. The second erroneous diagnosis (tuberculosis) was considered because an aetiological factor could not be established, and because the multifocal distribution of the consolidation persisted during the broad spectrum antibiotic therapy. Nonetheless, on this occasion, the clinical and laboratory findings were not consistent with the diagnosis either (in tuberculosis, haemoptysis is usually an early symptom, but it was absent in the patient described); a radiological finding such as that in Fig. 1 is associated with the presence of Mycobacterium tuberculosis in the sputum examination. In an immunocompetent host, the clinical condition more similar to a consumptive syndrome, progression of the pulmonary infiltrate until destruction of the host parenchyma, absence of fever and haemoptysis, and major chest pain should have led to an earlier suspicion of carcinoma.
In conclusion, we would like to emphasise the fact that chest X-ray is not usually sufficient to establish the diagnosis and that laboratory findings must correlate with the patient's clinical condition5; the diagnosis of lung cancer is thus often delayed in young patients, thereby missing the opportunity to instigate curative treatment.
FundingThe authors have not received any financial aid.
Conflict of InterestsThe authors have not declared any conflict of interests.
We would like to thank Professor Dr. Miron Bogdan for his support and contribution.
Please cite this article as: Paraschiv B, et al. Carcinoma broncoalveolar en un paciente joven: caso clínico. Arch Bronconeumol. 2013;49:315–6.