Benign laryngotracheal tumours of the minor salivary glands are rare,1 so experience in their treatment and evolution is limited. Indeed, we did not find any evidence of previous publication of a case of monomorphic adenoma in a subglottic location (PubMed, keys words: subglottic/laryngotracheal adenoma; larynx salivary adenoma; monomorphic/basal cell adenoma. Period covered: 1979–2012. Updated 17/11/2012).
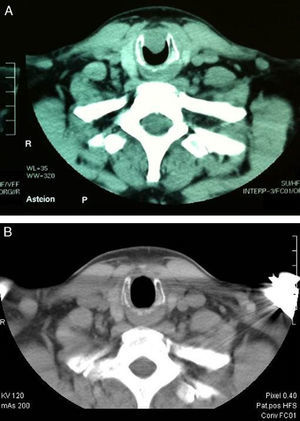
We describe the case of a 50-year-old man who attended due to a three-month history of progressive dyspnoea on moderate and heavy exertion, with mild inspiratory stridor. A history of previous intubation due to two collarbone surgeries two years previously was noted. Nasofibrolaryngoscopy showed a right anterior subglottic lesion; its extension was determined by computed axial tomography (CT) (Fig. 1A). Rigid bronchoscopy and laser resection (Neodymium-YAG) was scheduled; during surgery, biopsies were taken and partial vaporisation of the lesion was performed. The histopathological result was consistent with a pleomorphic adenoma, so subglottic resection was carried out using an open approach in a second surgical procedure: the trachea was exposed with an incision over the second ring, similar to a tracheotomy; cricothyroid membrane incision; vertical connection of the left side of both incisions (cricoid arch and tracheal ring section), lifting a flap to visualise the lesion directly (15cm in diameter, situated along the inside of the cricoid arch up to the height of the upper border of the first tracheal ring). Tumour excision was completed with partial cricotracheal resection (cricoid arch and anterior portion of the first tracheal ring). The defect was closed by primary reconstruction with sternothyroid muscle plasty over a Montgomery silicone T-tube (8mm) and layered wound closure. After five days, the patient was discharged with mild-moderate cervical subcutaneous emphysema, which persisted for five weeks, odynophagia, requiring a soft diet for one month, and dysphonia due to the placement of the upper rim of the stent on the vocal cords. The definitive histopathological study was a benign salivary gland tumour, consistent with basal cell adenoma (monomorphic adenoma), with clear margins. The T-stent was removed after four months. Vocal granulomas were detected, which disappeared in two weeks after treatment with oral prednisone (30mg in tapered dosage), and the voice returned to normal. The case has been monitored by nasofibrolaryngoscopy and radiological follow-up (Fig. 1B) for the last 1.5 years, with no evidence of recurrence to date.
Despite its rarity, the possibility of a benign salivary gland tumour should not be excluded when there is a subglottic lesion, even in cases in which more common lesions such as granulomas are suspected.1,3 The endoscopic surgical approach (laryngoscopy, rigid bronchoscopy or flexible fibrobronchoscopy) for biopsy and histopathological study enables monomorphic adenoma to be diagnosed and differentiated from polymorphic adenoma, a more common tumour, and from basal cell carcinoma.1–3 Diagnostic bronchoscopy occasionally permits complete excision of the lesion1 or reduction of the tumour mass if this is not possible, which in this case achieved clinical improvement until definitive treatment using an open approach.3 Laryngotracheal resection and laryngotracheoplasty have been widely described in the literature by Grillo and Mathisen4 and other authors.5 In the case reported, reconstruction of the laryngeal (anterior cricoid) and tracheal (first ring) defect was performed using prelaryngeal muscles over a Montgomery T-tube, as anastomosis of the distal trachea to the remaining cricoid was impossible. The use of a T-tube as a stent for the laryngotracheal lumen (with a good result in this case) may be controversial, and to date, there are no precise indications. Although it ensures the airway in case of eventual laryngotracheomalacia or stenosis, it is not always essential after laryngotracheoplasty,4,5 and is not exempt from complications, mainly endoluminal granulomas in 19%–41% of cases, depending on the series.6 In conclusion, for benign tumours of the minor salivary glands in an anterior subglottic location, if endoscopic treatment is not possible, an open approach with partial laryngotracheal resection and immediate reconstruction with muscle plasty over a T-stent may be a satisfactory alternative, permitting the voice to be conserved, with relatively low morbidity.
Please cite this article as: Larrosa F, Canalís E. Adenoma de células basales subglótico: resección laringotraqueal-laringotraqueoplastia. Arch Bronconeumol. 2013;49:314–5.