More than 10 years ago, Archivos de Bronconeumologia published an editorial entitled “Bronchiectasis: Still an Orphan Disease?”.1 The author referred to a significant increase in the number of diagnoses, to the extent that, from an epidemiological point of view, bronchiectasis could no longer be defined as an orphan disease.2 However, it was still “orphan” from a scientific point of view, given the worrying lack of clinical trials at that time. What has changed in the last decade to prompt the sudden interest in bronchiectasis? The growing number of bronchiectasis diagnoses is probably due to the wider availability of improved imaging techniques and the aging of the population,3 but beyond that, 2 main reasons account for this resurgence: on the one hand, some groups of researchers chose to dedicate themselves to the investigation of this disease, and on the other, the interest of the scientific societies and the commercial development of emerging therapies for bronchiectasis have attracted more investment in teaching and research.
In recent years, SEPAR has supported research in bronchiectasis. The outcome has been the formation of a growing group of researchers who continue to face important challenges, such as raising awareness among health professionals of the importance of this disease and the need for accurate and early diagnosis and treatment, and developing multiple lines of research. In fact, SEPAR was the first group worldwide to publish specific guidelines on bronchiectasis (2008),4 defining to a large extent the optimal treatment still used today. A new edition of these guidelines, prepared with the same spirit of innovation and advancement, has been recently published.5,6 SEPAR's efforts also led to the creation of the Spanish bronchiectasis registry in 2002. This database now contains data on more than 2000 patients, and was recently updated (2014) with follow-up data from RIBRON, a computerized registry of Spanish bronchiectasis patients7; this information will facilitate many future studies conducted in Spain. Renewed interest in bronchiectasis is not confined to Spain. For many years now, various groups of European researchers have been making important scientific contributions. In 2010, the British Thoracic Society published the first British bronchiectasis guidelines.8 In 2012, a collaboration group sponsored by the European Respiratory Society, in which several SEPAR members participated, launched an extensive research and teaching project, culminating with the publication of the European Bronchectasis Guidelines9 and the creation of a European registry, the European Multicentre Bronchiectasis Adult and Research Collaboration (EMBARC), that has already enrolled 10,000 patients. Like our Spanish registries, this valuable database will play a key role in productive, collaborative research in the future.10 In the US, the Bronchiectasis Research Registry was set up in 2008, and more than 1800 patients have been included.11 And finally, in Asia and Latin America, interest in bronchiectasis has been growing in recent years, and the number of publications from these regions is increasing. The result is that it is now impossible to imagine a respiratory medicine congress without a bronchiectasis interest area, reflecting our need to deepen our insight into a disease that has already become common in our respiratory medicine clinics and wards. The high level of attendance and participation in the second World Bronchiectasis Congress held in July this year, 2017, would have been unheard of several years ago.12
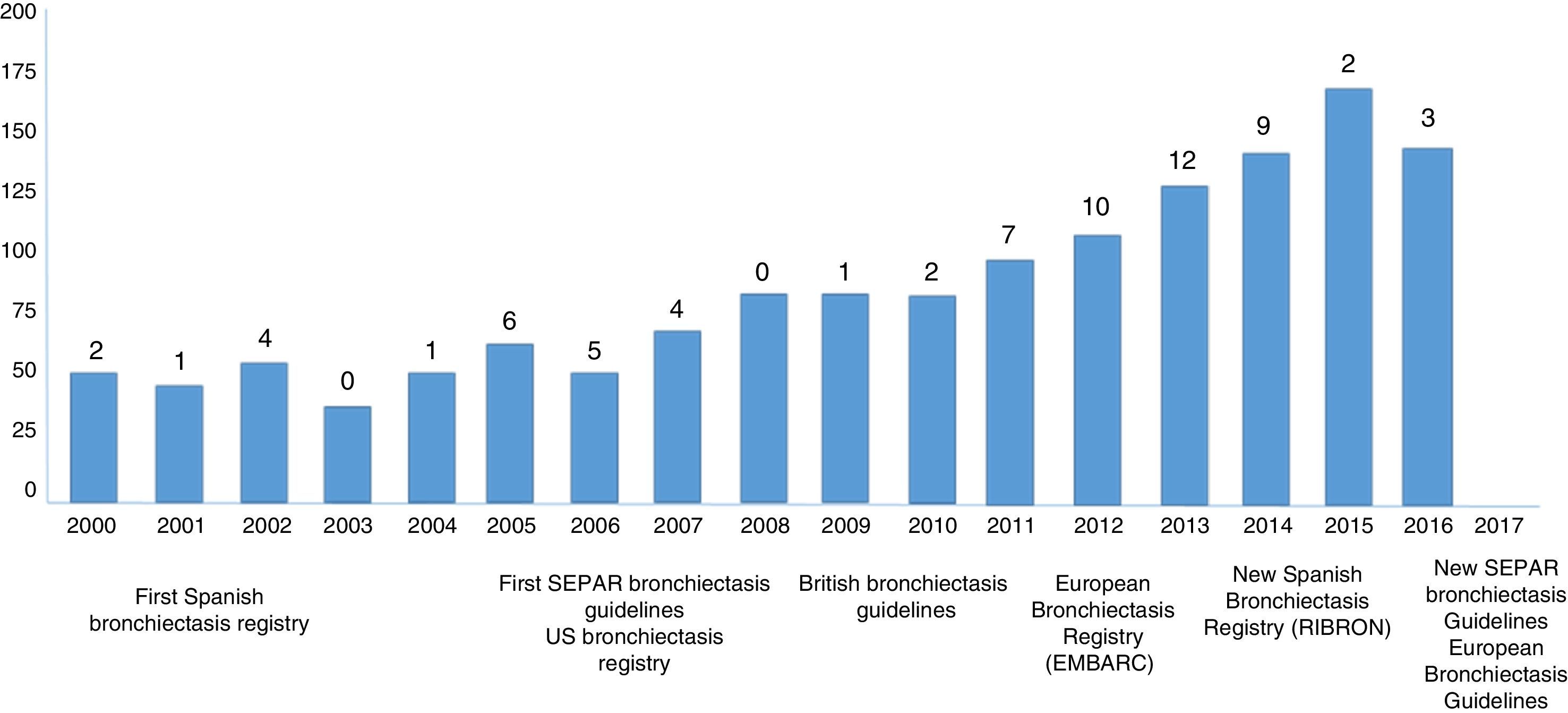
Although the driving force behind our increased understanding of this disease has clearly been the curiosity of our physicians and the needs of our patients, it is undeniable that another key factor has been the support of industry and the scientific societies, without which it would be difficult to implement teaching or scientific activities. While the accumulated scientific evidence appears rather scant compared to that available for other airway diseases, such as COPD, asthma, and cystic fibrosis (for example, the scientific evidence surrounding cystic fibrosis is vastly greater, even though its prevalence is 10 times lower than that of bronchiectasis due to other causes), the number of clinical trials conducted in bronchiectasis has increased considerably (Fig. 1). Moreover, more than 50% of clinical trials have been performed since 2010. The most notable studies are those which explore the effect of macrolides and inhaled antibiotics. Macrolides have shown a clear benefit in these patients,13 and 3 specific formulations of antibiotics for inhalation are already on the market and widely used (and others are expected to follow), pending the accumulation of sufficient scientific evidence to establish a formal indication in bronchiectasis.14
Bibliometric analysis of bronchiectasis publications in the 21st century. The bars represent the number of annual publications on bronchiectasis indexed in PubMed, and the numbers above the bars represent the number of clinical trials performed. The specific year of publication or creation of bronchiectasis guidelines or registries appears at the bottom of the chart.
Of course, there is still a long way to go and many goals must still be achieved in the management this disease, which, due to its varied presentation and frequent comorbidities, sometimes presents a therapeutic challenge for medical professionals. If management is to be effective, we must elucidate current epidemiological trends, determine the impact of bronchiectasis on any underlying causative disease, make progress in the pathophysiological and microbiological study of the entity (including the microbiome), explore the different phenotypes and endotypes of patients to provide more individualized treatment, create simple, useful, inexpensive tools that simultaneously take into account the severity criteria (multidimensional scores), impact (quality of life), and activity (biomarkers) of the disease, explore the problem of exacerbations, and above all, improve our therapeutic knowledge. To achieve these goals, it is essential to clarify cost-effectiveness, type, dosing or indications of the treatments commonly used in bronchiectasis, such as bronchodilators and combinations, inhaled steroids and antibiotics, and other non-pharmacological treatments.15 First though, we need to agree on a number of definitions that will allow subsequent studies to be comparable, starting with the definition of bronchiectasis itself, chronic bronchial infection, eradication, and radiological or clinical severity criteria, among others.
In recent years, we have seen a strong resurgence in bronchiectasis. In the next decade, we hope to consolidate our scientific knowledge and standardize our management of this disease, so that in our next editorial on bronchiectasis we can confirm that almost all the foregoing gaps in our knowledge have been filled, to the benefit of our patients. Large amounts of hard work, enthusiasm, and increasing international cooperation in this area are all needed to achieve this goal.
Please cite this article as: Martínez-García MÁ, de la Rosa-Carrillo D. Bronquiectasias: resurgiendo de sus propias cenizas. Arch Bronconeumol. 2018;54:59–60.