Elastofibroma dorsi (ED) is an uncommon, non-encapsulated, non-benign tumor characterized by the proliferation of elastin fibers in a stroma of collagen and fatty connective tissue.1 It is typically seen in people over the age of 602 and in women, with a male to female ratio of 13:1.3 We report two cases of a rare presentation for this type of pathology.
The first case is a 57-year-old symptomatic woman, with right elastofibroma measuring 5cm×4cm that was satisfactorily removed surgically. Two years later, the patient presented a new mass measuring 2.3cm×2.3cm, although without symptoms, which was extirpated. The second case is that of a 51-year-old man presenting bilateral subscapular masses. They were resected sequentially. Both in the first as well as in the second case, the anatomopathologic results were elastofibroma.
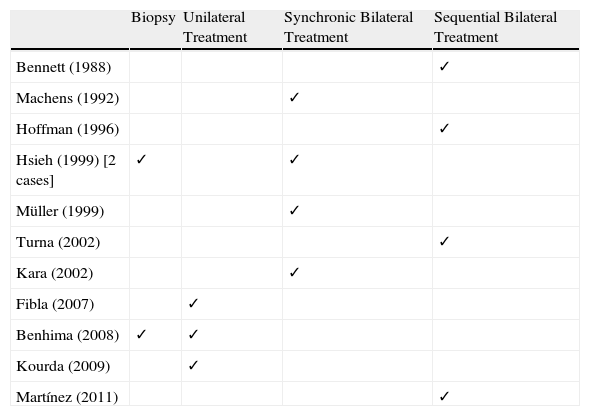
Although the estimated prevalence of ED is 2%2 in asymptomatic patients, in series of autopsies individuals over the age of 50 seem to present a prevalence of subclinical ED (<3cm) reaching 24% in women and 11% in men.1 In practice, within the exceptional nature of this type of tumors, a bilateral occurrence is extremely rare, and in the literature there are only 11 preceding clinical reports (Table 1), although in the series of autopsies there is also an observed prevalence of bilaterality that is greater than expected (7%).4
Management of Bilateral ED According to Different Authors.
| Biopsy | Unilateral Treatment | Synchronic Bilateral Treatment | Sequential Bilateral Treatment | |
| Bennett (1988) | ✓ | |||
| Machens (1992) | ✓ | |||
| Hoffman (1996) | ✓ | |||
| Hsieh (1999) [2 cases] | ✓ | ✓ | ||
| Müller (1999) | ✓ | |||
| Turna (2002) | ✓ | |||
| Kara (2002) | ✓ | |||
| Fibla (2007) | ✓ | |||
| Benhima (2008) | ✓ | ✓ | ||
| Kourda (2009) | ✓ | |||
| Martínez (2011) | ✓ |
Diagnosis by imaging studies is usually begun with radiography, which can detect either a soft tissue mass or an elevation of the scapula. On ultrasound, a sub- and pre-scapular mass with a fibrillar, fasciculated appearance is usually observed. On CT, it is seen as a non-encapsulated mass that is lenticular in shape, isodense with the surrounding musculature, and with hypodense striations that correspond with dense fat. Lastly, MRI, which is considered the main imaging technique for its diagnosis, shows the ED as a fatty and fibrous lesion, as seen in a heterogeneous image with areas of intensity similar to muscle tissue (the fibrous part), together with others that are hyperintense in strata alternating with the fibrous layers.1
Classically, there was an indication for the need to carry out biopsy.1,2,5 Today, due to the greater specificity of the imaging tests in making the diagnosis, this need has been relegated to the exceptional atypical presentation that can make more difficult the differential diagnosis with pathologies such as sarcoma, desmoid tumors, lipoma, fibroma, schwannoma or hemangioma.2,6
Surgical treatment is usually reserved for symptomatic cases larger than 5cm.1,2,6 In our cases, surgery was indicated sequentially due to the metachronic presentation in the first case and in order to avoid greater patient morbidity in the second. In the literature, synchronic as well as sequential or unilateral approaches (not contralateral) have been used (Table 1), each with favorable evolution and with no relapses. We may therefore conclude that the method of choice is that which best fits the characteristics and needs of the patient.
In conclusion, it is suffice to state that bilaterality in ED, although rare, is possible and should be contemplated at the time of diagnosis.
Please cite this article as: Martínez Hernández NJ, et al. Elastofibroma dorsi bilateral: una muy rara presentación para una rara patología. Arch Bronconeumol. 2011;47:536–7.