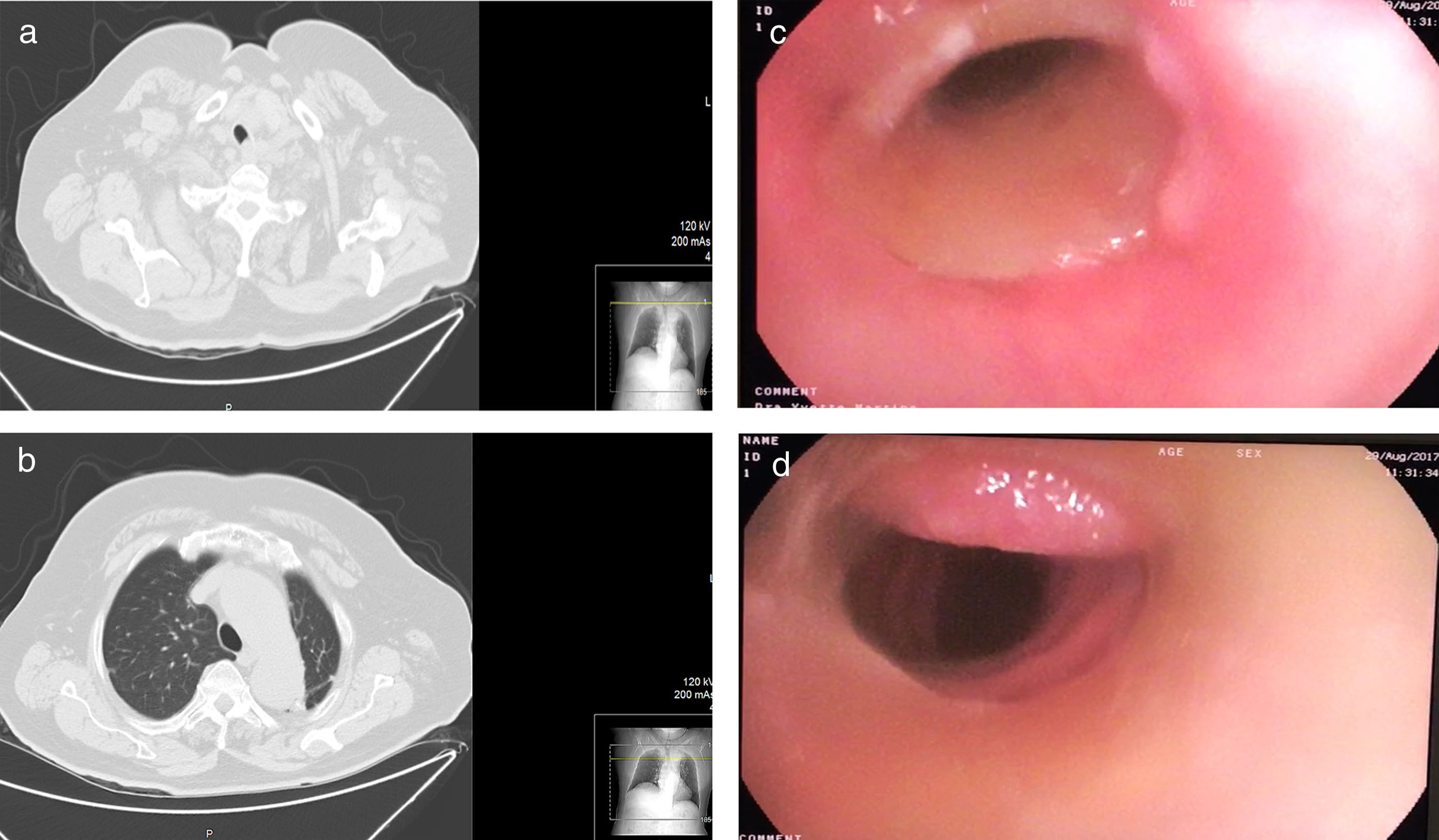
A 94-year-old woman presents to the emergency department in 2010 for progressive dyspnea and stridor over a period of 3 weeks. Thoracic computed tomography scan shows tracheal stenosis >50% (Fig. 1a) and generalized ectasia of the thoracic aorta (Fig. 1b). Bronchofibroscopy showed extrinsic compression of the lateral and anterior left wall of the trachea, 2cm from vocal chords, and 3cm in extension. Tracheal stenting (HOOD BSP-1430-M-S®) with rigid bronchoscope was successfully performed. Seven years later (missed follow-up visits) is again admitted to the emergency department due to respiratory infection. A reassessment bronchofibroscopy was performed revealing a well implanted stent, 1cm from the vocal chords (Fig. 1c – proximal view from vocal chords) with discrete granulation tissue in the left lateral wall of the trachea (Fig. 1d – distal view). Stents can cause long-term complications including excess granulation tissue, migration, recurrent infections or even stent fracture.1 Most stents are intended for palliative purposes and there is no abundance of data on the longevity of these devices. This case describes an unexpected stent duration (total of 7 years) without major complications. The endoscopic approach allowed significant and lasting symptomatic relief and reduction in morbidity.
(a) Axial cut of chest CT scan showing narrowing of the trachea resulting in stenosis >50%. (b) Axial cut of chest CT scan showing ectasia of the aorta and a fibrotic streak in left upper lobe. (c) Proximal endoscopic view from between vocal chords (left vocal chord seen as a white shadow on the right) showing a well implanted stent with discrete granulation tissue in the left lateral wall of the trachea. (d) Distal endoscopic view of the stent showing discrete granulation tissue in the posterior wall of the trachea.