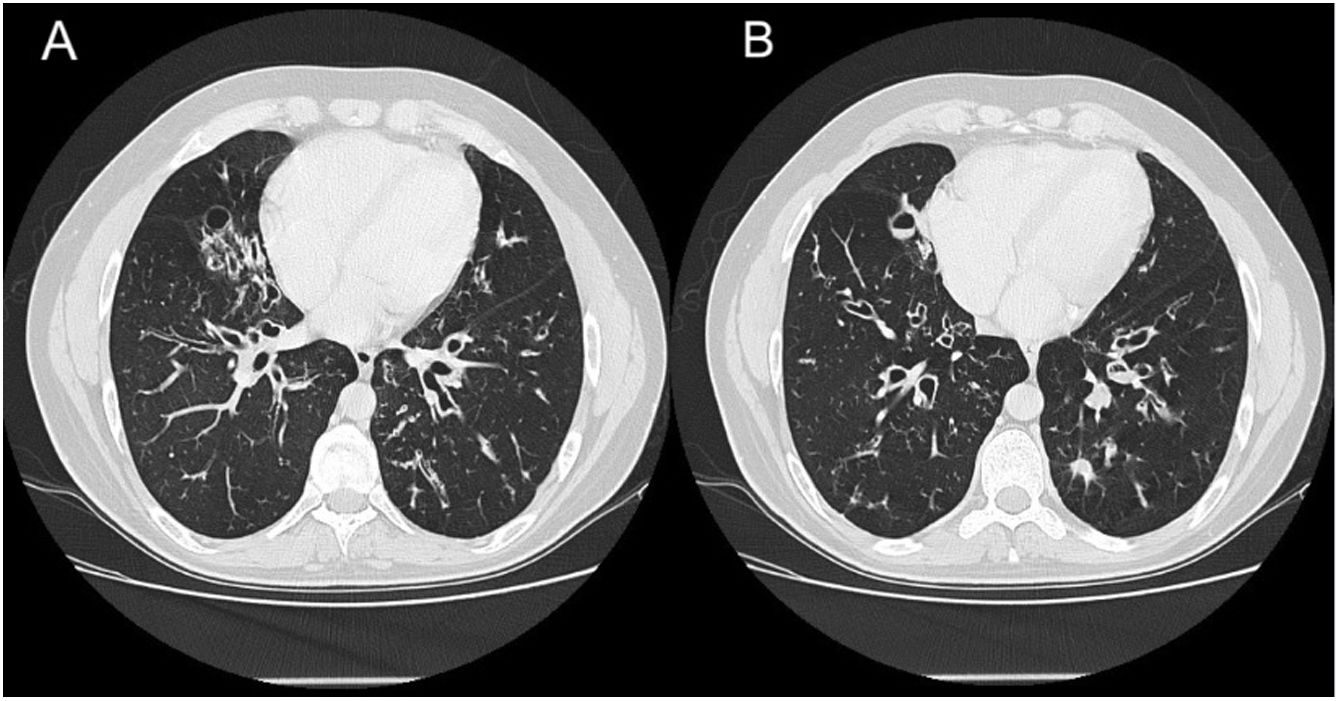
We report the case of a 34-year-old man, referred to the pulmonology department for multiple recurrent respiratory infections since childhood. Other issues include obesity, polydactyly, hypogonadism, mental retardation, and retinitis pigmentosa. He reported persistent productive cough. The study was completed with a computed tomography scan of the chest (Fig. 1A, B) that showed images of bilateral bronchiectasis and bronchiolectasis predominantly in the middle fields and lower lobes of both hemithoraces. Spirometry showed moderate airflow obstruction, a bronchodilator test was negative, and intermittent Streptococcus pneumoniae infection limited to exacerbations was detected. A sweat test and full laboratory tests were performed, including immunoglobulins, all of which were negative; however, in view of his morphological characteristics, the patient was referred to the genetics department, where he was finally diagnosed with Bardet–Biedl syndrome.
(A, B) Computed tomography images showing bilateral bronchiectasis and bronchiolectasis predominantly in the middle fields and lower lobes of both hemithoraces. Other findings included distal branched images and centriacinar nodules measuring around 1mm, associated with distal airway involvement.
Bardet–Biedl syndrome (BBS), first described at the beginning of the 20th century by Bardet and Biedl,1 is an autosomal recessive disease characterized by truncular obesity accompanied by other disorders, the major criteria being gonadal hypoplasia, mental retardation, retinitis pigmentosa, postaxial polydactyly, and renal malformations. Other minor criteria of the disease are hypertension and diabetes, but the finding of bronchiectasis in this syndrome is exceptional. Incidence of BBS varies geographically, ranging from 1/160,000 in northern Europe to 1/13,500 among some Kuwaiti communities.1 In Spain, estimated prevalence is 1:407,000 with a male:female ratio of 1.4:1.2
The BBS is one of the ciliopathies, a group of clinically and genetically heterogeneous diseases caused by alterations in the formation and function of the primary cilia.3 These changes compromise the mucociliary clearance of both the upper and lower respiratory tract and predispose to chronic respiratory infections. This might suggest that bronchiectasis would be common in all ciliopathies, but in fact they are only described very exceptionally in BBS,4 as in our case.
The diagnosis is clinical. Four major criteria or 3 major and 2 minor criteria, as determined by Beales et al.,1 are required, and BBS can be confirmed by genetic sequencing in a high percentage of cases.
More than 20 genes associated with BBS have been described to date, including BBS1, BBS2, BBS4, BBS5, BBS7, BBS8, BBS9, BBS18ARL6/BBS3, and SDCCAG8/BBS16, which encode proteins that form a structural or functional part of the primary cilia.2,3
BBS is very rare and, given its multisystem involvement and variable clinical presentation, requires a multidisciplinary approach. Patients must be evaluated and followed up by a nephrologist, ophthalmologist, endocrinologist, nutritionist, and psychopedagogy consultant among other specialists. They must be carefully and regularly monitored for changes in weight, blood pressure, blood glucose, kidney function, liver, lipids, and thyroid, and must receive intensive treatment for frequent comorbidities, such as high blood pressure or diabetes mellitus.
Specific treatment is not yet available, so research into future therapeutic targets is essential.
In the literature, only 3 other cases of BBS associated with bronchiectasis have been described, underlining the unusual nature of our case.5
Conflict of interestsThe authors state that they have no conflict of interests.