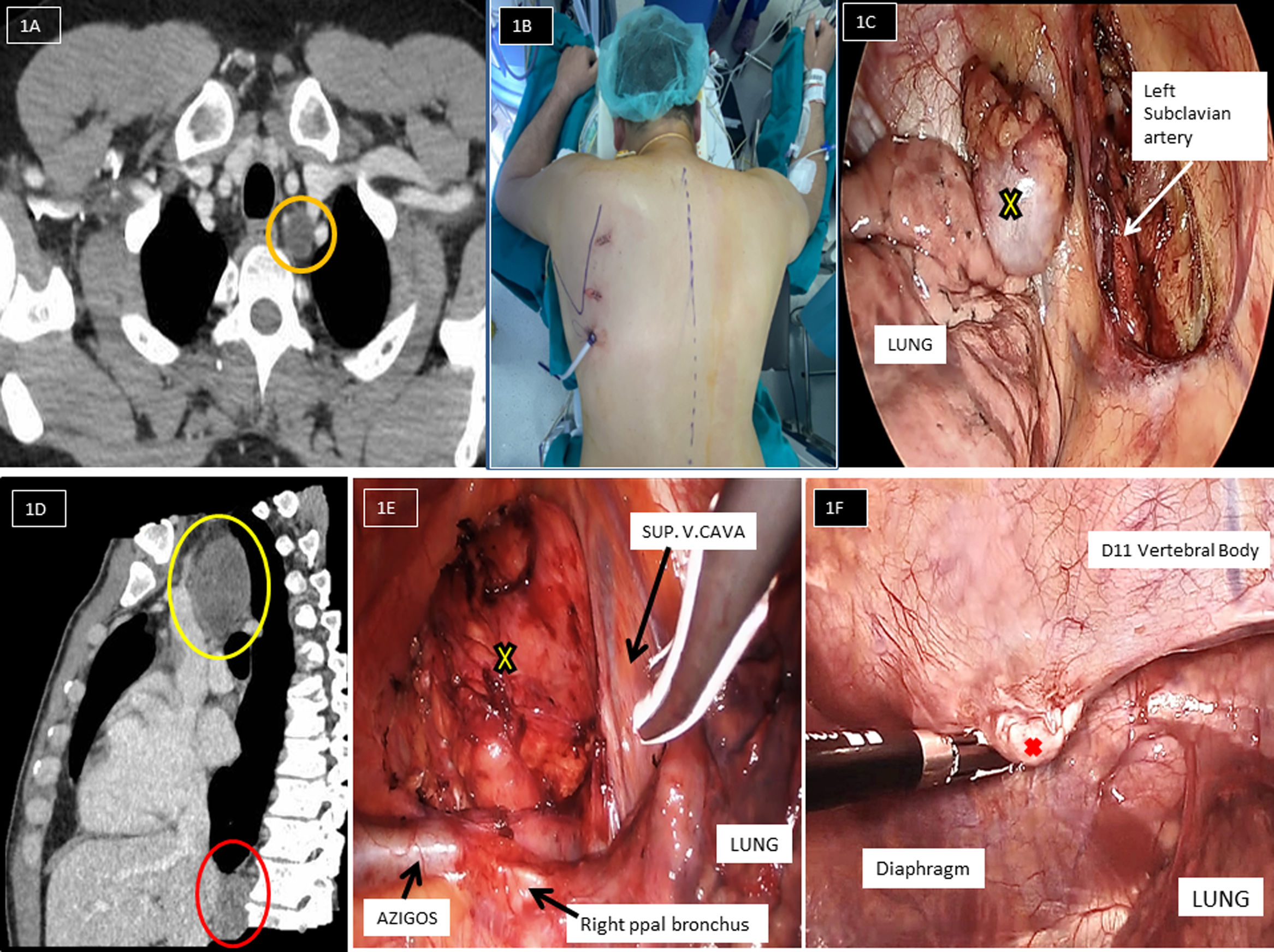
We present a 31-years-old male patient, operated for non-seminomatous testicular germ cell tumor (NSTGCT) type choriocarcinoma (stage IIIc). He underwent neoadjuvant chemotherapy and orchiectomy with retroperitoneal lymph nodes metastasis dissection. He was followed up for 2 years when a tomography scan revealed a left paratracheal mass (25mm×17mm×13mm), in contact with left subclavian artery (Fig. 1A). To resect this apical-posterior mediastinal mass, video-assisted thoracoscopic surgery (VATS) in standard position could be difficult for the presence of left subclavian artery. Finally, we decided a left thoracoscopic access with carbon dioxide insufflation in prone position (Fig. 1B). Under general anesthesia with selective intubation, the patient was placed prone decubitus. At the start of the intervention, carbon dioxide insufflation at pressures of 5–8mmHg was used to facilitate rapid and complete lung collapse. Three left thoracoscopic ports were utilized (Fig. 1B): 3th intercostal-space in parascapular line (5mm), 5th intercostal-space in parascapular line (5mm) and 7th intercostal-space in the inferior angle of the scapula (11mm). The left subclavian artery was dissected without any problems. This step was necessary to reach and to resect completely the left paratracheal mass (Fig. 1C). The histology confirmed metastatic teratoma.
(A) Axial contrast-enhanced computed tomography image of the chest shows a left posterior mediastinal mass (orange circle), between trachea and left subclavian artery. (B) This picture shows the patient position in prone and the thoracoscopic ports placed. (C) Left posterior mediastinal mass (yellow cross) dissection by left VATS in prone. (D) Sagittal contrast-enhanced computed tomography image of the chest shows a right paratracheal mass (yellow circle) behind to superior vena cava and the paravertebral mass (red circle). (E) Right paratracheal mass dissection (yellow cross) by right VATS in prone. (F) Right paravertebral mass dissection (red cross) by right VATS in prone.
The patient was a 30-years-old man. The diagnosis was NSTGCT type teratoma stage IIIb. Neoadjuvant chemotherapy and orchiectomy were performed. Twenty months later, recurrences of disease in posterior mediastinum on positron emission tomography and tomography scan follow-up were observed: right paratracheal mass (50mm×42mm×31mm) and right paravertebral mass in D11–D12 (20mm×15mm×8mm) (Fig. 1D). The most difficult anatomical regions to approach by conventional VATS are paravertebral zone, paraesophageal space and apico-posterior mediastinum. Therefore, we decided right VATS in prone position. The same technique was repeated again: anesthesia, position and thoracoscopic ports. The good exposure of the operative field was fine: lung and heart get down and right hemidiaphragm falls anteriorly from its normal position. The dissection the paratracheal mass (Fig. 1E) and the paravertebral relapse (Fig. 1F) were performed without any problem: lung and diaphragm retraction were not necessary. The histology confirmed necrotic (>95%) metastasis of teratoma.
Both patients were discharged at 48h after surgery and at the moment there is no evidence of local tumor recurrence.
DiscussionThe benefits and oncological outcomes of VATS for the diagnostics and therapy of many thoracic diseases have been widely described and published in the literature.1–3 The standard surgical approach is in lateral position. We reported an interesting solution to resect posterior mediastinal mass. To our knowledge, there are only two case reports about the technical and oncological feasibility of VATS in prone position in the literature.4,5 In both cases, paraesophageal mass resection was performed. We presented this approach in complex cases with excellent clinical and oncological outcomes: superior mediastinal tumors, D11 paravertebral mass and large tumors. The effects of gravity in prone position and carbon dioxide insufflation provide us excellent exposure of the anatomical structures of posterior mediastinum without the additional retraction help during dissection. Thus, we recommended VATS in prone position to posterior mediastinal surgical approach: it is a safe and feasible procedure.
Conflict of InterestsThe authors state that they have no conflict of interests.