To examine the relationship between severe vitamin D deficiency, asthma control, and pulmonary function in Turkish adults with asthma.
MethodsOne hundred six asthmatic patients underwent pulmonary function tests (PFT) skin prick test, peripheral blood eosinophil counts, IgE, body mass index (BMI) and vitamin D levels were determined. Patients were divided into 2 subgroups according to vitamin D levels (vitamin D level <10ng/ml and vitamin D level ≥10ng/ml). Asthma control tests (ACTs) were performed.
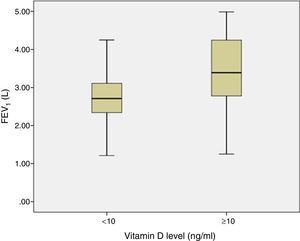
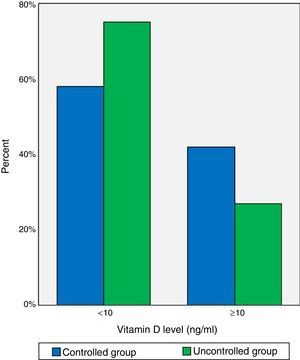
ResultsThe mean age of subgroup I (vitamin D level <10) was 37±10 and the mean age of subgroup II (vitamin D level ≥10ng/ml) was 34±8. Sixty-six percent of patients had severe vitamin D deficiency (vitamin D level <10ng/ml). There was a significant trend toward lower absolute FEV1 (L) values in patients with lower vitamin D levels (P=.001). ACT scores were significantly low in the severe deficiency group than the other group (P=.02). There were a greater number of patients with uncontrolled asthma (ACT scores <20) in the severe vitamin D deficiency group (P=.040). Patients with severe vitamin D deficiency had a higher usage of inhaled corticosteroids than the group without severe vitamin D deficiency (P=.015). There was a significant trend toward lower absolute FEV1 (L) (P=.005, r=0.272) values in patients with lower vitamin D levels. Vitamin D levels were inversely related with body mass index (BMI) (P=.046).
ConclusionThe incidence of severe vitamin D deficiency was high in adult Turkish asthmatics. In addition, lower vitamin D levels were associated with poor asthma control and decreased pulmonary function.
Examinar la relación existente entre el déficit grave de vitamina D, el control del asma y la función pulmonar en adultos turcos asmáticos.
MétodosCiento seis pacientes asmáticos se sometieron a pruebas de función pulmonar (PFP), pruebas intraepidérmicas y determinaciones de eosinófilos en sangre periférica, IgE, índice de masa corporal (IMC) y concentraciones de vitamina D. Las concentraciones de vitamina D se dividieron en 2 grupos (concentración de vitamina D <10ng/ml y ≥10ng/ml). Se practicaron pruebas de control del asma (ATC).
ResultadosLa media de edad de los pacientes fue de 37±10años en el primer grupo (concentración de vitamina D <10ng/ml) y de 34±8años en el segundo (concentración de vitamina D ≥10ng/ml). El 66% de los pacientes presentaban déficit grave de vitamina D (concentración de vitamina D <10ng/ml). Los pacientes con concentraciones bajas de vitamina D mostraron una tendencia significativa a presentar valores absolutos más bajos de FEV1 (l) (p=0,001). Las puntuaciones ATC fueron significativamente más bajas en el grupo con déficit grave de vitamina D que en el segundo grupo (p=0,02). En el grupo con déficit grave hubo un mayor número de pacientes con asma incontrolada (puntuaciones ACT<20) (p=0,040). Los pacientes con déficit grave de vitamina D habían utilizado muchos más corticoides inhalados que los que no presentaban déficit grave (p=0,015). En los pacientes con concentraciones más bajas de vitamina D se observó una tendencia significativa a presentar valores absolutos más bajos de FEV1 (l) (p=0,005, r=0,272). Se observó una relación inversa entre las concentraciones de vitamina D y el IMC (p=0,046).
ConclusiónLa incidencia de déficit grave de vitamina D fue elevada en adultos asmáticos turcos. Además, las concentraciones más bajas de vitamina D se asociaron con descensos del control del asma y de la función pulmonar.
Vitamin D deficiency has become more prevalent and is mainly attributed to diet, lifestyle, and behavioral changes. Recent reports have shown how decreased vitamin D levels may adversely influence asthma outcomes.
Vitamin D plays a key role in regulating the innate immune system, and is a major player in the production of antimicrobial peptides that kill microorganisms. Vitamin D deficiency has been linked to a predisposition to respiratory infections, which are major triggers for asthma attacks.1,2 Previous studies have shown that children with mild to moderate asthma who also had low serum vitamin D levels had poor asthma control, more exacerbations,3 more hospitalizations in the previous year, decreased lung function, reduced responses to inhaled corticosteroids (ICS), and consequently, increased ICS use.4–8 Furthermore, it has been reported that serum vitamin D levels are positively related with FEV1% predicted and the ratio of FEV1 to FVC. In addition, serum Vitamin D is inversely related with increased airway responsiveness, airway remodeling, and response to glucocorticosteroids.9,10
Little is known of the effect of severity of vitamin D deficiency in asthma patients. The aim of this cross-sectional study was to investigate the potential relationship between severe vitamin D deficiency, pulmonary function, and asthma control in Turkish adult patients with asthma.
MethodsStudy SubjectsThis cross-sectional, prospective study included individuals aged 18 years and older who were seen at the Asthma Clinic of Marmara University Hospital in Istanbul, Turkey for bronchial asthma. Entry criteria included physician diagnosed asthma and evidence of disease from a bronchodilator reversibility test.11 Approval for the study was obtained from the institutional review board and all patients provided written informed consent prior to taking part in the study. A power analysis was carried out to determine sample size.
One hundred twenty-four patients meeting the above criteria were screened between September 2012 and April 2013. Patients were excluded due to pregnancy or evidence in their medical records of comorbidities, including diabetes mellitus, coronary artery disease, cancer, and chronic obstructive pulmonary disease (COPD), or reported use of vitamin D supplements, ≥10 pack years of cigarette smoke exposure that could overlap with COPD, or hospitalization for asthma in the previous month. Additionally, 3 individuals refused to provide informed consent, leaving a final study population of 106 participants.
Study MeasurementsAll patients agreed to provide their medical history, undergo a physical examination, and then perform spirometry in line with the American Thoracic Society criteria12 to assess forced expiratory volume in 1s (FEV1) and other pulmonary function parameters (MIR Spirolab II, ITALY). We assessed current medication (ICS, long-acting beta-2 agonists, anti-leukotrienes, and theophyllines) and whether the patient had been treated in the emergency department or had required inpatient care for asthma in the previous year. The patient's height (cm), weight (kg), and body mass index (BMI, kg/m2) were determined.
During the physical examination, blood samples for vitamin D measurements were collected in EDTA tubes, then centrifuged, aliquoted, and stored at −80°C. Plasma 25-hydroxyvitamin D was measured using the Tandem test (liquid chromatography/mass spectrometry–mass spectrometry, Zivak Technologies, Turkey). Patients were divided into 2 subgroups (vitamin D level <10ng/ml and vitamin D level ≥10ng/ml).
A skin prick test was defined as positive when a wheal measuring >3mm was produced in response to aeroallergens (SAY ILAC, Turkey). An IgE level of >100IU/l was defined as high, measured by chemiluminescence immunometric assay (Immulite 2000, Siemens Healthcare Diagnostics, USA). Peripheral blood eosinophil counts were determined on peripheral blood smears, and patients with counts ≥3% were categorized as ≥eosinophilic.
Asthma control was assessed using the Turkish translation of the asthma control test (ACT).13 The ACT is a standardized, validated questionnaire that assesses asthma control on a scale of 5 to 25.14
Statistical AnalysesA one-way analysis of variance (ANOVA) was used to compare mean values of continuous variables between groups, and categorical variables were compared using Pearson Chi-square analyses. After adjusting for the potential confounding effects of sex, age, BMI, smoking, and allergic status, we conducted a linear regression assessment of the correlation between vitamin D levels, asthma control and pulmonary function parameters. Strengths of association were assessed using the Pearson correlation test. IgE levels were logarithmically transformed. All P values were two-tailed, and P<.05 was accepted as statistically significance. Stata version 20 was used for statistical analyses.
ResultsCharacteristics of the SubjectsThe main characteristics of the study participants are summarized in Table 1, stratified according to vitamin D levels. Thirteen percent of subjects had intermittent asthma and were being treated only with beta-2 agonists as required. The remaining patients had persistent asthma and were using ICS, with or without a long-acting beta-2 agonist, alongside rescue medication. Four patients had a clinical history of emergency department visits/hospitalizations, and 1 patient had used a systemic corticosteroid in the previous year. Based on the GINA guidelines, 53 patients (50%) were determined to have controlled and partly controlled asthma and the remaining 53 had uncontrolled asthma. Allergic rhinitis was reported in 58.5% of the patients. Thirty-seven of the 106 patients (35%) were allergic to at least 1 common allergen, determined by skin prick testing.
Body Mass Index, Lung Function Parameters, Asthma Control Test Scores, Inhaled Corticosteroid Use and Atopy in Patients with Asthma.
| Vitamin D | P | ||
|---|---|---|---|
| <10 (ng/ml) | ≥10 (ng/ml) | ||
| Number of patients (n) | 70 | 36 | .001 |
| Age (yr) | 37±10 | 34±8 | .148 |
| Male % | 30% | 70% | .001 |
| BMI, kg/m2 | 29±6 | 27±5 | .046 |
| ACT | 18±4 | 20±4 | .02 |
| ICS n (%) | 65 (93%) | 27 (75%) | .015 |
| FEV1 (L) | 2.75±0.7 | 3.40±0.9 | .001 |
| FEV1 (%) | 98±19 | 101±19 | .041 |
| FEV1/FVC (%) | 78.6±8.8 | 80.4±8.6 | .306 |
| FEF25–75 (l/s) | 2.67±1.2 | 3.41±1.2 | .004 |
| FEF25–75 (%) | 72±31 | 83±18 | .078 |
| Allergic rhinitis (%) | 51 | 62 | .040 |
| Skin prick test positive (number) | 24 | 13 | .046 |
| Eosinophil % | 2±1 | 2±1 | .075 |
| IgE (IU/l) | 50 (30–80) | 88 (50–110) | .025 |
The statistically significant parametres are in bold.
Patients were divided into 2 subgroups, according to vitamin D levels: subgroup I: severe vitamin D deficiency (vitamin D level <10ng/ml); subgroup II: no severe vitamin D deficiency (vitamin D level ≥10ng/ml). According to stratification of vitamin D levels, 70 patients had severe vitamin D deficiency.
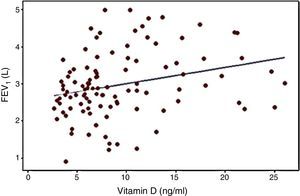
Pulmonary Function ParametersThere was a significant trend toward lower absolute FEV1 (L) (P=.001) values in patients with lower vitamin D levels (Fig. 1).
Asthma ControlSerum vitamin D levels were not correlated with ACT.
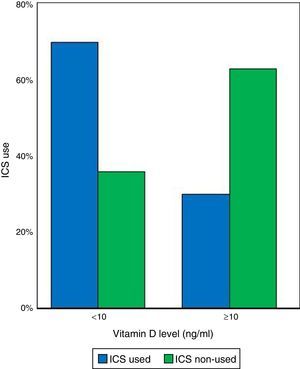
Patients were divided into 2 subgroups according to vitamin D levels (vitamin D level <10ng/ml and vitamin D level ≥10ng/ml). ACT scores were significantly lower in the severe deficiency group than the second group (P=.02). A greater number of patients had uncontrolled asthma (ACT scores <20) with severe vitamin D deficiency (P=.040). However, serum vitamin D levels were not correlated with ACT, even when considered separately as vitamin D level <10ng/ml and vitamin D level ≥10ng/ml. Forty of the 53 patients with uncontrolled asthma had severe vitamin D deficiency (Fig. 2). Patients with severe vitamin D deficiency had significantly higher usage of ICS than the group without severe vitamin D deficiency (P=.015, Fig. 3).
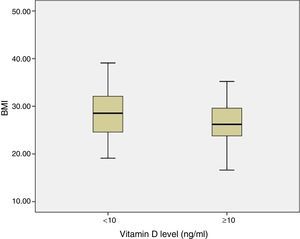
Association Between Serum Vitamin D LEVELS and FEV1, Body Mass Index, Sex, Allergic StatusThere was a significant trend toward lower absolute FEV1 (L) (P=.005, r=0.272) values in patients with lower vitamin D levels (Fig. 4). There was an inverse relationship between BMI (kg/m2) and serum vitamin D levels (P<.046; Fig. 5). There was a significant difference between female and male patients in terms of severity of vitamin D deficiency: 90% of females had severe vitamin D deficiency (P=.001).
Thirty-seven of the 106 patients (35%) were allergic to at least 1 common allergen (mite, aspergillus, grass, etc.), determined by skin prick testing. There was no clear association between serum vitamin D level and age, smoking status, or skin prick test positivity. However, IgE levels were positively correlated with vitamin D (P=.025). Similarly, patients without severe vitamin D deficiency were more prone to allergic rhinitis than patients with severe vitamin D deficiency (P=.04).
DiscussionWe found that a high prevalence of Turkish adult asthmatics suffered from severe vitamin D deficiency. We believe that this is the only study to have assessed the effect of vitamin D levels on asthma control in Turkish adult asthmatics. Lower vitamin D levels were associated with uncontrolled asthma and higher ICS usage in Turkish adults with asthma. We observed correlations between serum vitamin D level and FEV1 (L) pulmonary parameters. In addition, vitamin D levels were inversely related with BMI.
Several previous epidemiologic investigations have shown a link between low serum vitamin D and asthma in pediatric patients, but few have examined the immediate effects of vitamin D levels in adult asthmatics.3,4,6–9,15,16 Turkish pediatric asthmatics have lower vitamin D levels than control subjects, and 90.6% of pediatric asthmatics have a deficiency or insufficiency of vitamin D.2 The high prevalence found in our series is similar to that previously reported in Chinese and Costa Rican adult asthmatic populations, and is consistent with reported epidemics of hypovitaminosis D in developing countries.15,16 It is arguable that without the use of supplements, the threshold of 30ng/ml for vitamin D sufficiency would not be attainable for most of the sun-averse population of Turkey.
The mechanisms underlying the role of vitamin D in the pathogenesis of asthma are unclear. Vitamin D has been related to innate and adaptive immunity and airway remodeling.10,17–20 Higher vitamin D levels were associated with better FEV1 and FVC values in adults in the USA (16). Similarly, we found that low vitamin D levels were associated with lower FEV1 (L). Conversely, the relationship between vitamin D and FEV1 (L) was not statistically significant in a Costa Rican study (P<.07).16 These variations may be due to different sample sizes and different ethnic populations. Vitamin D is known to effect the muskulosketal system, and it also plays a role in cancer, infectious diseases, cardiovascular diseases, diabetes, and respiratory diseases. In a recent study, the authors reviewed the physiology of vitamin D, the pathophysiological effects associated with its deficiency, and its role in respiratory diseases.21
Elevated serum IgE levels are known to be a risk factor for asthma.22 The National Health and Nutrition Examination Survey of children and adults in the USA (2005–2006) reported that vitamin D deficiency was associated with higher levels of IgE sensitization in both the pediatric and adolescent groups, but not in adult asthmatics.23,24 Furthermore, the association between vitamin D and total IgE was subsequently reported in adult asthmatics in China, Costa Rica, and Germany.15,16,25 Similarly, we found no inverse correlation between vitamin D and IgE levels; we found a positive correlation. The discrepancy between this finding and previous studies can be mainly attributed to a non-linear link between vitamin D and IgE levels, with a cut-off effect in which abnormal vitamin D levels are associated with elevated IgE concentrations.23
Importantly, patients with severe vitamin D deficiency had lower ACT scores. Similarly, several studies noted a positive association between vitamin D levels and asthma control in children, as set out by the ACT and the Global Initiative for Asthma (GINA) guidlines.7,10 Vitamin D insufficiency has been shown to put patients at greater risk of severe asthma exacerbations and hospitalization.4,8 In addition, children with insufficient serum vitamin D levels have an increased risk of hospitalization, emergency department visits, and severe asthma exacerbations, regardless of their use of ICS.4–6,8,9 A study of Turkish pediatric asthmatic patients found that asthma severity increased in parallel with a decrease in vitamin D levels, and emergency department visits and hospitalization rates increased.2 These associations were also observed in adult asthmatic patients. One explanation for these previously reported results and those from this study is that lower vitamin D levels may contribute to increasing asthma severity, resulting in the increased use of pharmacological agents, and an increase in the number of hospitalizations. We found lower ACT scores in patients in the vitamin D <10ng/ml group than in the vitamin D ≥10ng/ml group; however, this association did not show any linear correlation. It is hard to pinpoint the reasons for this discrepancy, but it may be due to the wide range of vitamin D values in the study population. Unfortunately, we found few studies in severe vitamin D deficiency in asthma patients.
The VIDA (Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma) trial was a randomized, double-blind, parallel-group, placebo-controlled trial that studied adult patients with symptomatic asthma and serum 25-hydroxyvitamin D levels less of below 30ng/ml. The VIDA results indicated that therapeutic vitamin D3 supplementation failed to improve asthma control in adults.26 Nevertheless, little is known about vitamin D levels and their impact on disease control and airway function in Turkish adults with asthma.
In vitro studies have demonstrated how the vitamin D pathway “cross-talks” with the corticosteroid pathway.9,27,28 In this study, we showed that lower vitamin D levels are associated with increased use of ICS. Most patients with low vitamin D levels used inhaled corticosteroids. The use of daily maintenance ICS, oral corticosteroids, oral theophyllines, and leukotriene antagonists was significantly associated with lower vitamin D in children and adults.10 In another study, low vitamin D levels were weakly associated with greater lung function decline in adults with asthma, and stronger associations were observed in never smokers and non-ICS users.29
Population studies in North America and Europe have shown an association between BMI and lower vitamin D levels across all age groups in adults.30 In addition, BMI has a significant inverse correlation with serum vitamin D levels in children and adults with asthma.9,25,27,31 Similarly, in our study, we showed that lower vitamin D levels were linked with higher BMI values. Low vitamin D levels were not associated with airway obstruction in most asthma adults, with the exception of men with asthma but with no allergic rhinitis.32 It is also interesting to note that vitamin D concentrations were higher in men in a National Health Survey in the USA.31 Among all patients with asthma, patients with vitamin D insufficiency have a greater likelihood of being female.4,15 The results from our study have shown that female gender and overweight were both associated with low vitamin D. This may be because female and obese patients often spend less time engaged in outdoor activities.
Study LimitationOne limitation of our study is that vitamin D levels were measured between December and February, which is a time when skin production of vitamin D is low. This may have biased the results. It is also possible that people with reduced lung function have physical limitations and therefore spend less time exercising outdoors, and because of this, may have shorter periods of sun exposure. This may result in reverse causation. In addition, the number of subjects enrolled in this study was small, they may have constituted a selected population, and there was an imbalance in the number of females and males. We did not have detailed information on the socioeconomic and sociocultural status of the participants.
ConclusionWe found a high incidence of severe vitamin D deficiency among Turkish adult asthmatics (approximately 90%). We believe that this is the only study to have assessed the effect of vitamin D levels on asthma control and pulmonary function in Turkish adult asthmatics. Our results indicate that lower levels of vitamin D are linked to uncontrolled asthma, lower absolute FEV1 values, female sex and increased ICS use in Turkish adults with asthma. Further randomized controlled trials are required to demonstrate that vitamin D supplementation in asthmatics with vitamin D deficiency will lead to improved asthma outcomes.
Conflict of InterestsThe authors declare that they have no conflicts of interest.
The authors gratefully acknowledge Hatce Senol for helping to recruit subjects and for her assistance with testing, and William Vollmer for his help with statistical analyses and preparation of this manuscript.
Please cite this article as: Beyhan-Sagmen S, Baykan O, Balcan B, Ceyhan B. Asociación del déficit grave de vitamina D con la función pulmonar y el control del asma. Arch Bronconeumol. 2017;53:186–191.