In anesthesia for thoracic surgery, lung collapse by means of single-lung ventilation provides an immobile surgical field that improves surgical exposure.
During single-lung ventilation through a double-lumen tube, aspiration catheters are used to accelerate lung collapse and/or to improve oxygenation by either aspirating secretions or administering oxygen at low flows to the collapsed lung. Careful tracheal aspiration can become necessary upon re-establishing the bilateral ventilation after lung resection in order to clear away secretions and contribute to improved lung expansion.
We report a critical incident that happened when an aspiration catheter became included within the bronchial stump while a patient underwent left lower lobectomy with open surgery, and we analyze how this could have been avoided.
A 73-year-old male patient was proposed for left lower lobectomy due to a lung mass. In the pre-anesthesia office visit, the patient was cataloged as ASA III.
The surgical intervention was done under single-lung ventilation, and therefore the trachea was intubated with a double lumen tube (n 39 left, Rüsh, Germany) without any incidents, as confirmed with bronchoscopy (Pentax BF 9, Japan).
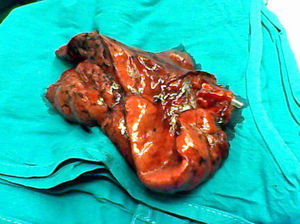
At one moment of the surgery, the surgeon requested that the bilateral ventilation be re-established. Upon doing so, the patient presented with audible secretions. Thus, when single-lung ventilation was reinitiated, the anesthesiologist inserted an aspiration catheter and aspirated secretions through the tracheal lumen first, then through the bronchial lumen. The patient then required the administration of the neuromuscular blocker, the catheter was forgotten within the bronchial lumen and, when the bronchial suture was performed, the catheter remained included in the stump. This became evident when the surgical piece was removed, so the surgeon opened the suture, released the catheter and redid the bronchial suture manually with stitches, covering the stump with parietal pleura (Fig. 1).
The patient was extubated in surgery and his clinical course was favorable and with no incidents; he was discharged 10 days later.
The anatomic pathology report of the surgical piece revealed the mass was a cavitating lung abscess, a benign disease.
This incident could have had fatal consequences (infection, dehiscence, bronchopleural fistula, short stump, etc.) and, more importantly, it should not have occurred, although there are reports of similar situations in the literature.1,2
It should not have happened because, before finishing the bronchial phase of a lobectomy, a test should be done in which the surgeon clamps the surgical bronchus in order to confirm the bronchial resection and the optimal ventilation of the remaining lung. To do so, the anesthesiologist unclamps the double-lumen tube, deflates the balloon of the bronchial blocker or withdraws the single-lumen tube, depending on the case, so the two lungs can be ventilated manually.3 No one stated or asked whether the test had been done. Prior to carrying out bronchial sutures is when devices that are in the airway and could become included in the suture line should be withdrawn or relocated.4
Communication among the members of the surgical team (surgeons and anaesthesiologists) is absolutely fundamental.
The distraction of the anesthesiologist brought about a mistaken choice of priorities. First, the patient should have been aspirated before initiating the bilateral ventilation, which should also have been communicated. Second, it was more important to administer the neuromuscular blocker to the patient (who was coughing) than to withdraw the aspiration catheter, which had done its function.
Regarding the use of aspiration catheters that accompany double-lumen tubes, we believe that in order to accelerate lung collapse there are effective maneuvers, such as checking the location of the tube with the bronchoscope, denitrogenating the lungs prior to initiating one-lung ventilation, releasing pleural adhesions or allowing apnea.
In order to improve oxygenation, it is more effective to apply CPAP to the proclive lung and/or PEEP to the declining lung, alveolar recruitment maneuvers, intermittently ventilate the proclive lung, or perhaps other forms of ventilation. Aspiration catheters should be used for what they have been designed for: the aspiration of secretions, when necessary, paying attention to the phase of the surgery.
Aspiration should be sterile, light and done with care. It should be brief, paying special attention to the hemodynamic response and the anesthetic state of the patient, always withdrawing the catheter when the aspiration is completed.
We conclude that, when in lung resections the surgeon requests that the bilateral ventilation be re-established, he/she should state whether the bronchial suture is going to be done in order to avoid that devices in the airway become trapped in the stump staples (bronchial blockers, left double lumen tube in a left pneumonectomy, aspiration catheters). Nevertheless, if nothing is said, then the anesthesiologist should ask.
Please cite this article as: Álvarez N, Fernández AB. Análisis de cómo una sonda de aspiración es incluida en la sutura bronquial durante cirugía de resección pulmonar. Arch Bronconeumol. 2012;48:342-3.