Forced spirometry (FS) is one of the principal diagnostic procedures in the study of patients with respiratory symptoms. Though considered a simple technique, it requires patient collaboration and must be performed by a highly qualified technician1. Nowadays, it is commonly performed in primary care, but difficulties in achieving appropriate quality levels are becoming apparent. Although the role of this procedure in respiratory medicine is well established, some controversy has arisen regarding the quality of results and underuse of the technique2–4.
New technologies have now emerged that facilitate technician training and the submission and monitoring of results to be performed online. We first became familiar with this approach when we participated in a multicenter study on the introduction of a telemedicine program for quality control of spirometries that included 12 centers in Spain5. We subsequently demonstrated how this program could be implemented in a public health service6, and how it could be cost-effective7, since failure to obtain quality spirometries generates additional expenses associated with overdiagnosis and overtreatment8.
This telemedicine program was implemented in our public health system in 2010. The application provides training in the performance of spirometry based on clinical guidelines1 and in the use of the computer application itself. After a 4-h training session, technicians submit the tests performed in their usual practice and these are evaluated according to the established quality standards1. This working practice means that technicians are offered continuous training.
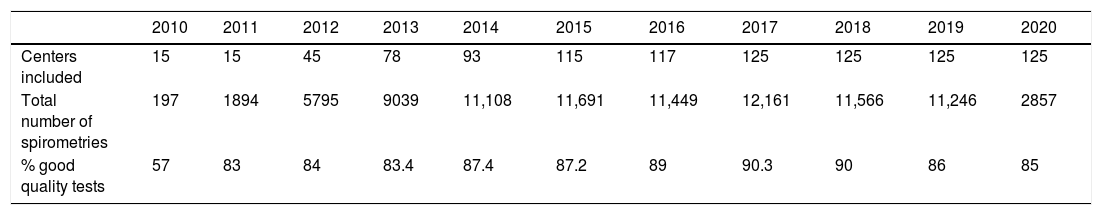
The program has now been in place for 10 years and a total of 125 primary care centers have been included (75% of all health system centers) and 500 nurses have been trained. In the first year (2010), 15 centers were incorporated. At the beginning of the program, 57% of spirometries performed in these centers were good quality, a figure that rose to 78% at 6 months and to 83% at 9 months (P < .001)6. Since then, quality has been evaluated annually, and the rates of good quality tests (83%–90%) have been maintained over the years since the implementation of the program (Table 1). In 2020, specifically since March, we observed a significant decrease in the number of tests performed due to Covid-19 restrictions (Tables 1 and 2). Thanks to this program, we have been able to streamline the spirometry protocol in the different centers, following the recommendations of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR)9, and we have reintroduced testing with the appropriate safety measures in place. In their editorial, Burgos et al.10 commented that once the first wave of Covid-19 in March 2020 had passed, the activity of both hospital and primary care lung function laboratories would have to resume.
Total number of sites included, number of tests, and percentage of good quality spirometries.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Centers included | 15 | 15 | 45 | 78 | 93 | 115 | 117 | 125 | 125 | 125 | 125 |
| Total number of spirometries | 197 | 1894 | 5795 | 9039 | 11,108 | 11,691 | 11,449 | 12,161 | 11,566 | 11,246 | 2857 |
| % good quality tests | 57 | 83 | 84 | 83.4 | 87.4 | 87.2 | 89 | 90.3 | 90 | 86 | 85 |
Number of spirometries performed per month between 2019 and 2020.
| Total | ||
|---|---|---|
| January | 2019 | 985 |
| 2020 | 1040 | |
| February | 2019 | 1019 |
| 2020 | 1264 | |
| March | 2019 | 1001 |
| 2020 | 425 | |
| April | 2019 | 1018 |
| 2020 | 1 | |
| May | 2019 | 1118 |
| 2020 | 6 | |
| June | 2019 | 1005 |
| 2020 | 22 | |
| July | 2019 | 715 |
| 2020 | 12 | |
| August | 2019 | 511 |
| 2020 | 0 | |
| September | 2019 | 843 |
| 2020 | 9 | |
| October | 2019 | 1101 |
| 2020 | 17 | |
| November | 2019 | 1086 |
| 2020 | 26 | |
| December | 2019 | 844 |
| 2020 | 35 | |
| Total | 2019 | 11,246 |
| 2020 | 2857 |
Various studies have assessed the use of telemedicine programs in the quality control of spirometries. The Alliance study11 collected a large number of spirometries (20,757), but confirmed that deficiencies observed in standard practice do not improve unless a training program is implemented. A high percentage of poor-quality tests was reported in this study. Mass et al.12 found that with telemedicine quality spirometries could be performed, even remotely, without direct contact with the patient, but this study was only applicable to a local setting. The same approach was used by Berlinski et al.13, who evaluated 38 patients and 50 spirometries, of which 84% were good quality. Represas et al.14 carried out a training program based on theoretical and practical workshops, improving technicians’ skills, but the quality of the studies declined over time. Thijssing et al.15 reported a telemedicine program that included telespirometry. They performed 227 spirometries over a period of 3 years, of which 31% were poor quality according to their guidelines, although these are not specified in the article.
The quality of spirometry performed in primary care in our setting has always been controversial because of the difficulty of achieving acceptable levels of quality. In Navarra, Hueto et al.3 found that very few procedures were performed according to guidelines, and that the quality of 76% of the tests was unacceptable. Naberan et al.4 reported that availability of the technique in primary care centers was limited and training was substandard, resulting in poor adherence to the guidelines. In our study, the quality evaluation at the beginning of the program after professionals had completed face-to-face training program in their own health center was 57%6, a level that we interpret as representative of our setting, although it must be borne in mind that the professionals were motivated and had attended an initial training workshop. Even so, these findings show that a one-off intervention cannot immediately yield optimal results, and support the idea that continuous training is more effective, especially in routine clinical practice.
The design of our program is practical, as it includes a single training session at the beginning, backed up by continuous ongoing training. In this way, centers can be included progressively. Our program offers the possibility of including a large number of spirometries, so it can be considered a universal application in any health area. This study shows that a telemedicine system for spirometry monitoring can achieve and maintain high levels of quality (greater than 80%) in the primary care setting over 10 years within a public health system. The implementation of this program was recognized as good practice by the Chronic Obstructive Pulmonary Disease Strategy of the National Health System in 201516.
Guidelines highlight the importance of training in helping the spirometry technician achieve appropriate test quality levels. This program ensures a unified, guideline-based1, training program for all technicians who perform this procedure in our health system. This intervention has helped reduce the proportion of poor-quality spirometries over the years, resulting in a cost-effective program7; it has had a major impact on the quality of spirometries, and provides clinicians with a valid instrument to reach a correct diagnosis.
FundingThe program is included in the Osakidetza (Basque Public Health Service) portfolio of services.
Conflict of interestsThe authors state that they have no conflict of interests.
We thank Juan Carlos Bayón and Asunción Gutiérrez (Osteba) for their review of our costing data.
Please cite this article as: Marina N, López de Santa María E, Martinez A, Andia J, Iriberri M, Gonzalez N, et al. Programa de telemedicina para el control de calidad de espirometrías en un sistema público de salud durante 10 años. Arch Bronconeumol. 2021;57:724–725.